Overview
To understand the physiology of the nose, its functions must be understood. The nose serves as the only means of bringing warm humidified air into the lungs. It is the primary organ for filtering out particles in inspired air, and it also serves to provide first-line immunologic defense by bringing inspired air in contact with mucous-coated membranes that contain immunoglobulin A (IgA). Inspired air is brought high into the nasal cavity to come in contact with the olfactory nerves, thereby providing the sense of smell, which is intimately associated with the taste sensation. Dysfunction of any of these systems can lead to symptoms of nasal dysfunction (eg, congestion, postnasal drainage, facial pressure, headaches, sinus infections). See the image below.
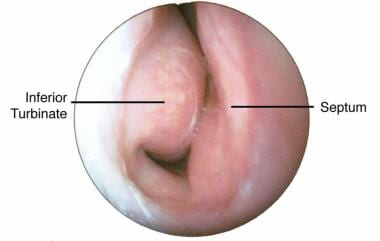 Endoscopic view from nares of right nasal passage. The turbinate is mildly swollen, the mucosa is pale, and the turbinate is impinging onto nasal septum.
Endoscopic view from nares of right nasal passage. The turbinate is mildly swollen, the mucosa is pale, and the turbinate is impinging onto nasal septum.
Awareness of the interrelationship between the upper and lower airways has increased; this concept is now known as the unified airway. The respiratory tract is considered to be an integrated system and whatever processes affect one also affect the other. Hence, changes in the physiology of the nose and paranasal sinuses can and will affect the lower airways and visa versa. [1]
Anatomy of the Nose
The external nose consists of paired nasal bones and upper and lower lateral cartilages. Internally, the nasal septum divides the nasal cavity into a right and left side. The lateral nasal wall consists of inferior and middle turbinates and occasionally a superior or supreme turbinate bone. The opening of the sinuses also is found under the middle turbinates on the lateral nasal wall. The lacrimal system drains into the nasal cavity below the anterior inferior aspect of the inferior turbinates.
As in the rest of the upper respiratory tract, nasal membranes are composed of ciliated pseudostratified glandular columnar epithelium. Cilia beat in unison to propel mucus from the nasal cavity and paranasal sinuses toward the nasopharynx where it can be swallowed. Mucociliary transport relies on mucus production and ciliary function. Normally, the nose and paranasal sinuses produce approximately 1 quart of mucus in 24 hours. The amount of mucus produced can more than double when the nose and/or sinuses are inflamed. Mucus contains IgA, immunoglobulin E, and muramidase. A study by Uzeloto et al indicated that mucociliary clearance is negatively impacted by active and passive smoking. [2]
Blood and autonomic nerve supply control secretions and the level of congestion of nasal membranes. General innervation to the nose is from the autonomic nervous system; the parasympathetic nerves supply the resting tone and control secretions. Contributions of nerve supply are from the facial nerve originating at the inferior salivatory nucleus and following along the distribution of the facial nerve through the sphenopalatine ganglion. Blood supply to the nose comes from branches of the internal and external carotid artery systems. Terminal branches of the internal maxillary artery supply most mucosal surfaces of the nasal cavity. Contributions from the ophthalmic artery of the internal carotid artery system supply the posterior aspect of the nasal cavity.
Olfactory nerve endings originate in the olfactory bulb under the frontal lobe and pass directly through the cribriform plate as second-order neurons entering the nasal cavity. Olfactory nerves are found on the superior portion of the septum, superior turbinates, and cribriform region. Information on the anatomy of the nose also can be found in the Medscape Reference articles Nasal Anatomy and Olfactory System Anatomy.
Nasal Airflow
Air flows superiorly into the nares, determined by its position and the anterior nasal valve. The airstream then turns posteriorly approximately 90° and flows into the nasopharynx. The airstream then turns inferiorly 90° through the pharynx and larynx and flows into the trachea toward the lungs. The anterior nasal valve is located 1.5-2 cm posterior to the anterior nares and is the narrowest portion of the upper airway. The narrow portion of the upper airway allows close contact between the airstream and mucosal surfaces. Humidification occurs by evaporation of moisture from the mucosal blanket. Air is humidified to 75-80%. Warming of inspired air to 36°C results from contact between air and the rich blood supply of the nasal membranes, especially the inferior turbinate mucosa.
Adults condition more than 14,000 liters of air per day, requiring more than 680 grams of water, approximately 20% of our daily water intake. [3]
The sniff is also an important part of nasal airflow; it provides a way to force air into the superior nasal vault and into better contact with the olfactory mucosa. Information on nasal airflow also can be found in the Medscape Reference article Nasal Aerodynamics.
With regard to the human nasal cycle, Williams and Eccles proposed a model for the central control of airflow patterns, in which in-phase and reciprocal airflow changes are explained through incorporation of a hypothalamic center and two brainstem half centers. [4, 5]
Abnormal Nasal Physiology
Environmental allergies are the most common causes of inflammation of nasal membranes, followed by inhaled irritants (eg, cigarette smoke, perfumes, various chemicals, and other noxious odorants).
Nonallergic, or vasomotor, rhinitis results from dysfunction of the autonomic nervous system or blood flow changes from iatrogenic or drug-related causes. [6] Increases in blood flow or parasympathetic tone or decreases in the sympathetic tone increase congestion and drainage of the nasal cavity. Conversely, reduction of blood flow, suppression of the parasympathetic system, and stimulation of the sympathetic system decrease nasal congestion and discharge. Supplemental female hormones or hormonal changes caused by pregnancy or menstruation may affect nasal systems. Any medications taken for hypertension or cardiac dysfunction may affect nasal physiology.
Nasal physiology also is affected by anatomic deformities that may have a varying effect on congestion, drainage, and olfaction. Septal deviation and enlarged turbinates can affect airflow into the nasal cavity, transforming it from a laminar pattern to a more turbulent pattern (see the images below). Turbulent airflow causes further irritation to nasal membranes, with a resultant increase in nasal drainage and congestion.
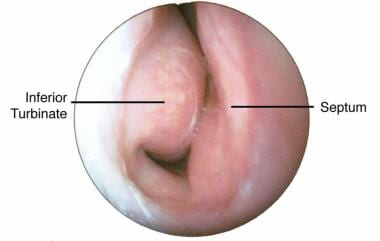 Endoscopic view from nares of right nasal passage. The turbinate is mildly swollen, the mucosa is pale, and the turbinate is impinging onto nasal septum.
Endoscopic view from nares of right nasal passage. The turbinate is mildly swollen, the mucosa is pale, and the turbinate is impinging onto nasal septum.
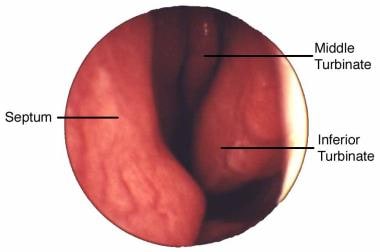 Endoscopic view from nares of left nasal passage. A mildly deviated septum is shown with a normal-appearing middle and inferior turbinate in view.
Endoscopic view from nares of left nasal passage. A mildly deviated septum is shown with a normal-appearing middle and inferior turbinate in view.
Nasal airway obstruction from turbinate hypertrophy, secondary to upper respiratory illness (URI) or allergic response, is the most common cause of temporary loss of smell. The sense of smell is important for quality of life, for taste, and for detecting smoke and other harmful odorants that could be life threatening.
In the upper airways, nasal cavities and paranasal sinuses are the main sources of nitric oxide (NO). Although the exact role of NO in nasal physiology remains poorly understood, the functions are thought to be host defense, ciliary motility, and an improved ventilation-perfusion ratio in the lungs by auto-inhalation. Low NO concentrations were reported in certain diseases, such as primary ciliary dyskinesia, cystic fibrosis, and acute and chronic maxillary sinusitis, whereas high concentrations were detected in upper airway infection, allergic rhinitis, and nasal polyposis.
Tests of Nasal Physiology
Tests of nasal physiology include studies of airflow, ciliary function, and olfaction.
Rhinomanometry attempts to quantify nasal airflow and total nasal area during exclusive nasal breathing. Differential pressure measurements are obtained by placing a nasal catheter into the nasopharynx. Nasal resistance measurement assesses all resistive components of the nasal airway from the anterior nares to the nasopharynx and is sensitive to small changes in airway caliber. This technique has been validated and is most useful for documenting changes in nasal patency caused by pharmaceutic or surgical interventions. It is moderately invasive, slow to perform, and requires patient assistance to complete.
Acoustic rhinometry is a newer technique for evaluating the cross-sectional area of the nose and the volume of the nasal cavity by analysis of incident and reflected sound during a brief cessation of nasal breathing. This technique also has been validated and is also useful for documenting changes in nasal patency caused by pharmaceutic or surgical interventions. It is minimally invasive, quick to perform, and requires little patient cooperation.
Rhinomanometry and acoustic rhinometry can be used clinically to evaluate nasal patency in a number of situations. [7] Either test may be used for a general evaluation of nasal airflow and to compare premorbid conditions with changes that may occur after medical or surgical therapy. Additionally, these tests can compare nasal passages for medical or surgical planning.
However, a critical analysis by Clement et al indicated that of three tests—active anterior rhinomanometry (AAR), four-phase rhinomanometry (4PR), and acoustic rhinometry—AAR is the best means of objective evaluation of nasal patency. The investigators also concluded that while acoustic rhinometry, which measures different parameters than AAR does, has certain limitations and cannot be used in place of AAR, it can be employed as a complementary test. In addition, Clement and colleagues maintained that although 4PR may be capable of supplying supplementary information, the open technical and mathematical inconsistencies conjoint with it have not been completely elucidated. [8]
Radiologic imaging with CT or MRI also can assess the cross-sectional area of nasal passages (see the Medscape Reference article Nasal Cavity Anatomy, Physiology, and Anomalies on CT Scan).
Studies by Leong et al [9] and Liu et al [10] conclude that computational fluid dynamic studies of nasal airflow and physiology have improved the understanding of the complex nasal anatomy and the implications of disease and surgery on physiology.
The saccharin test evaluates ciliary function by measuring the time it takes for a drop of saccharin to be tasted in the back of the throat when applied to the anterior tip of the inferior turbinate. [11, 2]
Multiple tests of olfaction are available, but the University of Pennsylvania Smell Identification Test (UPSIT) is used most commonly. [12] The UPSIT is a 40-item scratch-and-sniff test and is highly validated by age and sex.
Recent research into exhaled nitric oxide suggests that in the future, these measurements may prove valuable as non-invasive objective tools for the assessment and management of normal nasal physiology and nasal and sinus disorders. [13]
-
Endoscopic view from nares of right nasal passage. The turbinate is mildly swollen, the mucosa is pale, and the turbinate is impinging onto nasal septum.
-
Endoscopic view from nares of left nasal passage. A mildly deviated septum is shown with a normal-appearing middle and inferior turbinate in view.






