Background
The mimetic muscles direct facial movements. Under the control of the seventh cranial nerve (CN VII), the movement of these muscles correlates with the communication of human thought, emotion, and expression. Loss of this capacity is disfiguring and dysfunctional. At rest, an unnatural relaxation of the eyelid, cheek, and corner of the mouth is seen. Movement accentuates disfigurement. The lack of function leads to dry eye, ectropion, and conjunctivitis. Furthermore, alar collapse, nasal obstruction, muffled speech, and drooling occur. Cosmetically, the face is asymmetrical. The eyebrow, eyelids, cheeks, and lips droop. The frontal creases are lost, and the nasolabial fold flattens.
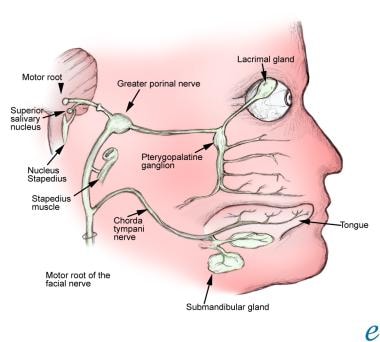
Several techniques have evolved to correct these deficits, including dynamic techniques such as nerve grafting and muscle transposition, and static techniques with fascial or alloplastic slings. [1, 2] Each technique has limitations, but each provides some restoration of both form and function and can be used in combination to optimize results. See the image below.
History of the Procedure
Three general categories for surgical techniques in facial reanimation exist: neural suturing and grafting, muscle transfer, and static techniques. These 3 techniques can be used either alone or in complementary combinations. Establishing a treatment plan depends on the mode of facial nerve injury, resultant deficit, prognosis for recovery, and wishes of the patient.
Neural techniques
Nerve repair is a dynamic reanimation technique. Within a distinct time frame, direct nerve repair by suture or graft can lead to good results. Rehabilitation of the facial nerve and subsequent reinnervation of the mimetic muscles is achieved. Direct suturing of the nerve endings can be accomplished in laceration injuries (eg, traumatic, iatrogenic) and is best accomplished immediately after injury, before the development of fibrosis and scarring. Primary repair is not always possible, however, in the context of life-threatening injuries. Severed nerves can be identified with clips or suture (nonabsorbable) to assist in later identification and repair.
Nerve-grafting techniques
These techniques are employed when direct suturing to the nerve trunk cannot be achieved without tension or following ablative procedures or trauma with resultant segmental nerve deficits. Donor sites for cable grafts include the great auricular nerve at the Erb point, the sural nerve, or the cervical plexus (C3, C4). Nerve crossover is another method for restoring function and is typically attempted with CN IX, XI, or XII. Crossover is useful, especially when the peripheral branches are intact, and the main trunk of the facial nerve is inaccessible.
Muscle transfer
Muscle transfer also is a dynamic reanimation technique. The use of muscle transfer is particularly useful with atrophy of the mimetic muscles and/or facial fat. Transfer of muscle can be accomplished in combination with neural grafting. Several different regional transfers have been described, but the masseteric and temporalis transfers remain the workhorses in muscle transfer techniques. Other regionally transferred muscles include frontalis, platysma, sternocleidomastoid, and trapezius. The masseteric transfer provides reanimation of the lower face with separate muscle slips sutured to the upper lip, oral commissure, and lower lip. The temporalis transfer allows correction at the orbit as well, or it can be used for restoration of the lower face. In each procedure, the muscle is divided into slips and is attached to the submucosa or subdermis.
Overcorrection is necessary to achieve satisfactory results, especially at the corner of the mouth. Within 3-6 weeks, the overcorrection resolves. The scalp defect after temporalis harvest can be corrected with an implant placed at the time of muscle transposition. In a 1995 report, Cheney describes harvesting the midportion of the temporalis muscle, then tightly suturing the residual muscle fascia to close the defect. [3] In his hands, this obviates the need for an implant at this site. Others have not reported the same experience. Microvascular free flaps provide another dynamic technique for facial reanimation. The free flap is often used in combination with a nerve crossover technique. Donor muscles include the extensor digitorum brevis, gracilis, latissimus dorsi, pectoralis minor, and serratus anterior. The advantage of free muscle transfer over regional muscle transfer has not been established.
Etiology
The various etiologies of facial paralysis can be classified into 3 major groups, ie, intracranial, intratemporal, and extracranial (see Relevant Anatomy). Regardless of the cause, the importance of establishing the degree and duration of weakness when evaluating a patient must be emphasized. An appreciation of these factors, along with the level of deficit at rest and level of dysfunction, are paramount to establishing an individualized treatment plan. Certainly, the goal of surgical intervention is to achieve an aesthetic appearance at rest, while contributing to sphincter control—ocular, nasal, and oral.
Etiology of facial paralysis
See the list below:
-
Birth - Dystrophia myotonica, forceps, Möbius syndrome
-
Iatrogenic - Anesthesia, surgery, vaccine
-
Idiopathic - Bell palsy, familial, Melkersson-Rosenthal syndrome
-
Infectious - Coxsackie virus, encephalitis, herpes, influenza, malaria, mastoiditis, mononucleosis, mumps, otitis, polio, sarcoid, syphilis
-
Metabolic - Diabetes mellitus, hyperthyroidism, pregnancy
-
Neoplastic - Acoustic neuroma, carcinoma, cholesteatoma, facial nerve tumor, glomus jugulare, hemangioma, Hand-Schüller-Christian disease, leukemia, meningioma, sarcoma, schwannoma, teratoma
-
Neurologic - Guillain-Barré syndrome, Millard-Gubler syndrome, muscular sclerosis (MS)
-
Toxic - Diphtheria, tetanus, thalidomide
-
Trauma - Altitude, facial injury, penetrating injury to middle ear, skull fracture
Relevant Anatomy
The mimetic muscles of the face are arranged in 4 layers. The muscles in the first 3 layers are innervated on their deep surfaces while the muscles of the fourth layer are innervated at their superficial surface. The main branches of the facial nerve are arranged consecutively deeper. The temporal branch is the most superficial while the zygomatic, buccal, and marginal branches lie in deeper layers. The muscles that comprise the 4 layers are as follows:
-
First layer - Depressor anguli oris, superficial portion of zygomaticus minor, orbicularis oculi
-
Second layer - Platysma, risorius, zygomaticus major, deep portion of zygomaticus minor, levator labii superioris alaeque nasi
-
Third layer - Levator labii superioris, orbicularis oris
-
Fourth layer - Levator anguli oris, mentalis, buccinator
Anatomic classification of facial paralysis
See the list below:
-
Intracranial - Agenesis or congenital abnormality, CNS degeneration, trauma, tumor, vascular abnormality
-
Intratemporal - Cholesteatoma, iatrogenic, infectious, trauma, tumor
-
Extratemporal - Iatrogenic, trauma, tumor
Contraindications
Several contraindications to dynamic facial reanimation exist, as follows: (1) absence of facial nerve branches or mimetic muscles of the face, (2) swallowing dysfunction, (3) denervated or excised temporalis and/or masseter muscles, and (4) compromised facial vasculature. Static reanimation can be accomplished with fascia or alloplastic material. Static reanimation allows for repositioning of the tissues that are affected by the pull of gravity. Resuspension by sling with multidirectional traction helps compensate for the complex contractions of the facial mimetic muscles. Furthermore, static reanimation may be an option for the debilitated patient who cannot withstand a longer operative procedure such as microvascular free flap or neural grafting techniques.
Contraindications for dynamic reanimation techniques
See the list below:
-
Ablation of distal facial nerve branch - Cable graft or nerve crossover CN X/VII
-
Absence of mimetic muscle (or atrophy) - Cable graft or nerve crossover CN X/VII
-
Damage to VII at brain stem - Cable graft or nerve crossover CN X/VII
-
Swallow dysfunction - Nerve crossover CN IX/VII
-
Absent or denervated temporalis - Muscle transposition
-
Absent or denervated masseter - Muscle transposition
-
Vascular compromise - Microvascular free flap
-
The facial nerve.