Practice Essentials
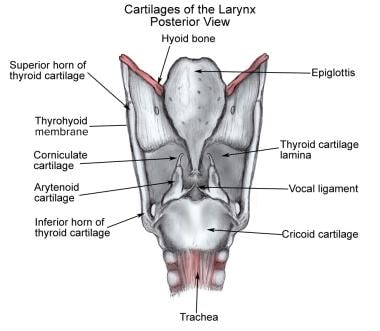
Function of the cricoarytenoid (CA) joint depends on the complex interaction of several cartilaginous, muscular, and ligamentous structures. Any process affecting the normal neuromuscular inputs, supporting connective structures, or joint space may result in altered function and immobility. As a broad entity, CA (vocal-fold) immobility has dissonant etiologies, including central nervous system (CNS) pathology, neuromuscular disease, malignancy, local trauma, and psychogenic causes. Among these, cricoarytenoid (CA) joint fixation is a recognized, albeit relatively uncommon, entity. The terms cricoarytenoid (CA) immobility and cricoarytenoid (CA) fixation are often used inexactly and interchangeably; such use blurs their distinctions. See the image below.
This discussion is limited to cricoarytenoid (CA) fixation resulting from altered function of the cricoarytenoid (CA) joint, which must be distinguished from other causes of vocal fold immobility to allow for timely diagnosis and effective treatment.
Workup in cricoarytenoid fixation
Operative direct laryngoscopy is the criterion standard for clinical evaluation of cricoarytenoid (CA) joint mobility.
Electromyography of the thyroarytenoid, cricothyroid, and posterior cricoarytenoid (CA) muscles help to clarify the status of laryngeal innervation, while videostroboscopy, electromyography, and computed tomography (CT) scanning may help to distinguish a fixed cricoarytenoid (CA) joint from an immobile vocal fold resulting from another cause.
Management of cricoarytenoid fixation
In general, acute cricoarytenoid (CA) rheumatoid arthritis is treated medically with anti-inflammatory and analgesic medications (with or without systemic steroid therapy).
Surgical procedures addressing arytenoid fixation can be organized into two categories. Techniques in the first group attempt to mobilize the cricoarytenoid (CA) joint in a manner analogous to joint mobilizations in the limbs. Techniques in the second group are based on the concession that the joint is irreparably fixed; they focus on improving the airway by alternative means.
Problem
Cricoarytenoid (CA) fixation, in contrast to other forms of vocal fold immobility, is a direct result of restricted joint motion without regard for the neuromuscular integrity of the larynx. This discussion is limited to processes affecting the joint space and resulting in loss of mobility.
Etiology
After cricoarytenoid (CA) joint fixation is diagnosed, determining the etiology is of paramount importance for therapeutic decision making. Following are the 3 general categories of causes of cricoarytenoid (CA) fixation:
Arthritides, primarily rheumatoid arthritis, account for many clinical diagnoses of cricoarytenoid (CA) fixation. Other known causes of joint arthritis include gout, Reiter syndrome, and ankylosing spondylitis. Anecdotal evidence suggests a mumps-associated laryngeal arthritis. This category also may include fixation secondary to radiation therapy.
Direct bacterial involvement of the joint space with infectious agents, such as streptococcal species, with resultant ankylosis is recognized.
Direct or external laryngeal trauma may result in joint injury. Mechanisms of intubation-related joint injury are suggested. These include posterior or anterior arytenoid displacement secondary to the distal tip of the endotracheal tube engaging the arytenoid during intubation. Some have noted the possibility of posterior dislocation resulting from extubation with a partially inflated endotracheal tube cuff. Another potential cause is arytenoid chondritis secondary to prolonged endotracheal intubation, which ultimately results in fibrosis. Zhong et al reported on a patient who experienced arytenoid dislocation following anterior cervical corpectomy and fusion. [1]
Previous authors have speculated that long-term paralysis with resultant cricoarytenoid (CA) immobility may lead to joint fixation, as observed in other diarthrodial joints in the body. However, histologic studies have failed to demonstrate this association.
A study by Tanaka et al reported that in transoral videolaryngoscopic surgery for hypopharyngeal and supraglottic cancer, resection of the medial and lateral pyriform sinus can lead to postoperative voice impairment; consequent to the operation, scar contracture around the cricoarytenoid joint can fix the arytenoid cartilage toward the lateral position and patients can experience insufficient glottic closure. [2]
It has also been found that the prolonged intubations experienced by patients with severe coronavirus disease 2019 (COVID-19) infection have resulted in more patients with vocal fold mobility impairment from various degrees of arytenoid fixation. [3, 4]
Pathophysiology
Laryngeal manifestations of arthritis, specifically rheumatoid arthritis, have been recognized for more than a century. The pathologic features of laryngeal rheumatoid arthritis are identical to those of other involved joints in the body.
The soft tissues surrounding the joint may have typical rheumatoid stigmata, including rheumatoid nodules.
Presentation
History
The typical history of a patient with cricoarytenoid (CA) fixation is identical to that for patients with other forms of joint immobility. Depending on the position of the immobilized vocal fold and the unilateral or bilateral nature of the dysfunction, symptoms may range from mild dysphonia to frank aspiration and even acute airway compromise. The diagnosis is contingent on the exclusion of the many other causes of immobility, and appropriate confirmatory examinations and studies are necessary.
Physical
In patients with an appropriate clinical history for cricoarytenoid (CA) fixation, physical examination should include complete head-and-neck examination, indirect laryngoscopy, and at least a cursory musculoskeletal survey. Operative direct laryngoscopy is the standard for clinical evaluation and definitive diagnosis of cricoarytenoid (CA) joint fixation (see Diagnostic Procedures).
In laryngeal rheumatoid arthritis, indirect laryngoscopy in the acute phase reveals erythema and swelling of the arytenoid mucosa. On clinical evaluation, 17-33% of patients with rheumatoid arthritis have identifiable laryngeal disease. Manipulation of the larynx is painful if the patient is awake. In the chronic stages of the disease, pain is unusual, and mucosal changes are somewhat less pronounced than before because they appear rough and thickened. Lateral bowing of the cords in inspiration, an uncommon finding in laryngeal paralysis, may be observed in both acute and chronic phases if both joints are involved.
Relevant Anatomy
The cricoarytenoid (CA) joint is a diarthrodial joint that includes a synovial lining and a fluid-filled bursa. The joint capsule and the ligamentous attachments, including the cricoarytenoid (CA) ligament, vocal ligament, and false vocal folds, limit normal motion of the joint. Motion of the arytenoid is characterized primarily as the arytenoid rocking over the long axis of the cricoid facet and gliding parallel to the long axis, as well as a small component of axial movement pivoting on the cricoarytenoid (CA) ligament. Three-dimensional analysis of cricoarytenoid mobility has demonstrated that the arytenoid has rotated superiorly, posteriorly, and laterally in full abduction. [5]
-
Cartilages of the larynx, posterior view.