Background
Laryngeal and tracheal stents are solid or hollow absorbable or nonabsorbable tubes of various shapes, sizes, and materials. Stents are used as primary treatment for lumen collapse or to stabilize a reconstructive effort of the larynx or trachea to prevent collapse. [1] Stents can be used for the larynx and the trachea individually, or they can be used interchangeably or concomitantly. This article reviews (1) various laryngeal, tracheal, and combination stents; (2) disease processes for which stents are used; and (3) new stent designs. [2]
An image depicting laryngeal and tracheal stents can be seen below.
For excellent patient education resources, see eMedicineHealth's patient education article Bronchoscopy.
History of the Procedure
The word stent is derived from Charles B. Stent, a British dentist who practiced in the late 19th century. Stent developed material that was used for dental impressions and, later, to support skin grafts. In current practice, the word stent refers to material that supports some form of tissue against collapse. Most often, stent describes devices that maintain the lumens of tubular organs.
In 1965, Montgomery described the use of silicone prostheses for tracheal stenting. Surgeons in other subspecialties, such as gastroesophageal, genitourinary, and vascular surgery, developed stents that remain useful in expanding lumens in these areas. This evolution increased the interest of otolaryngologists to develop stents for the larynx and tracheobronchial tree.
Problem
See the Indications section.
Indications
Laryngeal stents are often used to keep the airway expanded after surgical reconstruction or trauma. [3] Occasionally, laryngeal stents can be used for expansion of a disease process. Stents can be used for similar reasons in the trachea, especially to maintain lumen patency to prevent death. Stenting in the tracheobronchial tree is usually used as a last resort for severe conditions such as recurrent carcinoma and severe tracheal collapse that results in periods of prolonged apnea.
The most common indication for laryngeal stenting follows reconstruction of laryngotracheal stenosis (LTS; see the Medscape Drugs & Diseases articles Glottic Stenosis and Subglottic Stenosis in Children). Laryngeal stents can be used to keep the laryngeal lumen open and the reconstruction supported and stable. Occasionally, laryngeal stents are used following trauma to the larynx resulting in laryngeal fracture or injury. Stenting may help to maintain lumen patency and prevent mucosal lacerations from scarring.
In a study of 30 children who underwent tracheal disease surgery, either for congenital tracheal stenosis (25 patients) or acquired lesions (5 patients), Arcieri et al found that 19 patients (63%) required endoscopic reinterventions, including 13 (43.3%) in whom stent positioning was performed. [4]
A retrospective study by Nagano et al using multivariate analysis indicated that in cases of severe central airway obstruction caused by advanced cancer, stenting tends to achieve better outcomes in patients with a good prestenting performance status (PS). The mean poststenting survival period in patients who, before stenting, had a poor PS was 38.2 days, compared with 147.8 days in those with a good PS. [5]
Laryngotracheal stenosis
The first reason to use stents in cases of LTS is to support the larynx, typically with some form of autologous cartilage, after a reconstructive technique has been performed. A stent can be used to stabilize the cricoid plate once it has been divided anteriorly or posteriorly, with or without cartilage placement, to keep the complex in an expanded formation during healing. Stenting to help stabilize the laryngeal structure normally lasts for 2-6 weeks. Zalzal has showed that when a cartilage graft is inserted, the minimum time necessary for a posterior cricoid split to heal in a distracted manner is 2 weeks. If stenting is performed for a shorter duration, the graft may prolapse into the lumen.
For anterior graft placement only, stenting commonly lasts for a week or less, which usually occurs while a patient is endotracheally intubated in an intensive care unit (ICU). If the cartilage graft is made into a boat formation with flanges over the edge of the intraluminal portion of the graft, thus providing stabilization and preventing prolapse, see the images below, then ventilation with an endotracheal tube is not necessarily used for support but for protection of the airway while the edema resolves and the air leak around the reconstructive effort seals.
 Note the diamond-shaped internal intraluminal component. The shape of the rib is seen on the reverse side of the carved-out diamond-shaped wound.
Note the diamond-shaped internal intraluminal component. The shape of the rib is seen on the reverse side of the carved-out diamond-shaped wound.
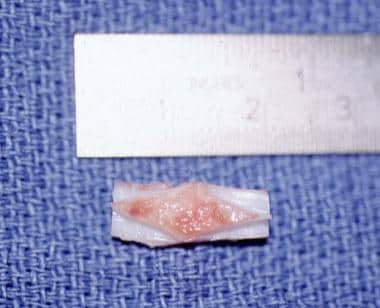 Another anterior graft with a diamond shape. Note that it is approximately 1.7 mm long. Again, the intraluminal site is seen facing up.
Another anterior graft with a diamond shape. Note that it is approximately 1.7 mm long. Again, the intraluminal site is seen facing up.
This helps prevent pneumomediastinum, pneumothorax, or both in concert. Often, a child can be extubated within a few days following surgery. With this graft design, a stent is not always required because the reconstructive area is already stabilized, provided no air leak has developed.
The second reason for stent placement in LTS repair is to counteract scar contraction. Theoretically, this requires stenting for a 6-month period. In general, guidelines to determine the duration of stenting depend on the consistency of the stenosis, the anatomical distortion of the disease process, and the stability of the reconstructive areas.
Laryngeal web or atresia
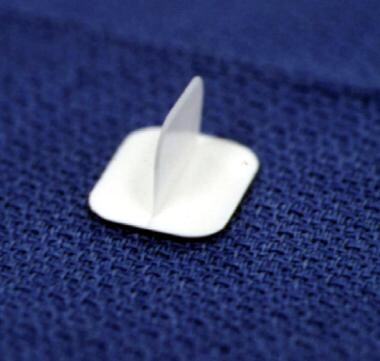
For a child with laryngeal web or atresia, a keel stent, shown below, is often placed to prevent the laryngeal web from reforming. Frequently, this stent is left in place for several weeks.
Tracheal lesions
The purpose of stenting for tracheal lesions varies from palliation, to cure, to stabilization while a reconstructive effort heals. In adults, primary cancer of the tracheobronchial tree or cancer from the head, neck, or chest that extends into the tracheobronchial tree frequently causes lumen compromise and airway obstruction.
The intraluminal component can be removed with laser treatment, mechanical debulking, electrocautery, brachytherapy, photodynamic therapy, or cryotherapy. A stent can then be placed to maintain the airway lumen following debridement to counteract collapse or edema. Alternatively, stents can be placed that help compress any lesion extending into the trachea or bronchi, without the need for debulking. Stents have been used successfully to palliate patients with inoperable bronchogenic cancer, primary tracheal tumors, and metastatic malignancies. Placing a stent in a patient with a terminal illness allows that patient to breathe comfortably and prevents death from asphyxiation.
In a retrospective study of 10 patients, Li et al reported that a single Y-shaped, self-expandable, metallic tracheal stent can alleviate a combination of carinal stenosis and stenosis of the right main and intermediate bronchi. Using a modified Borg scale to assess dyspnea in the study’s patients, all of whom had esophageal or lung cancer, the investigators found that the mean dyspnea score fell from 7.6 (prestenting) to 0.8 (poststenting). Moreover, no stenosis was seen on chest computed tomography (CT) scanning 3-5 days after stent placement. Patients had a mean poststenting survival time of 103 days. [6]
Tracheomalacia and bronchomalacia
Tracheomalacia and bronchomalacia (sometimes called tracheobronchomalacia) may be primary or secondary in nature. These conditions usually occur in children, but they can be observed in adults. Tracheomalacia and bronchomalacia are termed primary if they arise from primary cartilage abnormalities of the trachea, such as immature formation of the cartilaginous rings in neonates or relapsing polychondritis in children and adults. Primary tracheomalacia is often observed with a tracheoesophageal fistula.
Secondary tracheomalacia or bronchomalacia is caused by extrinsic compression from a structure in the mediastinum. These structures may be normal vascular structures (eg, aortic artery, heart) or abnormal vascular structures (eg, aortic arch ring, pulmonary artery sling, other congenital vascular abnormality). Additionally, secondary tracheomalacia or bronchomalacia can be caused by mediastinal cysts or neoplasms, including teratomas, lymphomas, and neuroblastomas.
Stenting of the trachea following surgical resection or reconstruction
If tracheomalacia or stenosis occurs following the resection of lesions, stents can be placed in the trachea to prevent scarring or to provide support for the operated segment while it heals.
In most situations, surgical correction as primary treatment for a disease process is preferred to stenting alone because complications are decreased. However, situations arise in which patients cannot undergo formal corrective surgery, and stent placement is the only way to prevent a severe apneic event or death. Tracheal stents have been placed following unsuccessful tracheal repairs, postanastomotic stricture after sleeve resection for lung transplantation, and following malacia from infections such as tuberculosis.
Following lesion excision
Any time the airway is opened to excise a lesion of the larynx, a stent can be considered for stabilization, scar prevention, or airway protection while edema resolves and the area heals. Frequently, this requires several days of intubation in the ICU, with the endotracheal tube acting as a temporary stent.
Types of stents
Different stents have different indications. Types include primarily laryngeal stents, primarily tracheal stents, combination tracheal and laryngeal stents, and stents that can be used either in the larynx or trachea.
Laryngeal stents
If stenosis is confined to the larynx (ie, glottis, subglottis), stenting can be short- or long-term. Short-term stenting is defined as stenting for less than 6 weeks. Long-term stenting is defined as stenting for more than 6 weeks.
Place a short stent for 6 weeks or less because granulation tissue forms at the lower end of the stent above the tracheotomy, potentially leading to tracheal stenosis or collapse above the tracheotomy site. Use short-term stenting for stabilization of cartilage grafts following laryngotracheal reconstruction (LTR) and/or for separation of mucosal surfaces during healing following laryngeal trauma, repair of web formation or atresia, or excision of a laryngeal lesion. Stents for these indications include Aboulker stents, silicone stents, Montgomery laryngeal stents, endotracheal tubes, and laryngeal keels. See the images below.
 Representative (noninclusive) sample demonstrating various sizes of Aboulker stents, ranging from 15 mm in diameter on the left to 3 mm in diameter on the right. These stents are hollow and coated with Teflon.
Representative (noninclusive) sample demonstrating various sizes of Aboulker stents, ranging from 15 mm in diameter on the left to 3 mm in diameter on the right. These stents are hollow and coated with Teflon.
 An end view of an Aboulker stent, showing the central opening. These stents are hollow and coated with Teflon.
An end view of an Aboulker stent, showing the central opening. These stents are hollow and coated with Teflon.
Occasionally, long-term stenting is required when the trachea above the tracheotomy tube requires stenting for either collapse or stenosis following reconstruction. In this case, a long stent wired to the trachea, shown in the images below, or a tracheal tube (T-tube), such as the Montgomery T-tube, shown below, can be used.
 Radiographic lateral neck view of a long stent connected to a metal Jackson tracheotomy tube at the bright inferior portion of the picture. The stent is seen in the airway as an oblong translucent area, with a rim of opacification around it that extends up through the larynx. A thin wire is seen connecting the stent and the tracheotomy tube.
Radiographic lateral neck view of a long stent connected to a metal Jackson tracheotomy tube at the bright inferior portion of the picture. The stent is seen in the airway as an oblong translucent area, with a rim of opacification around it that extends up through the larynx. A thin wire is seen connecting the stent and the tracheotomy tube.
Relevant Anatomy
Larynx
When a laryngeal stent is necessary, place it through and above the true and false vocal cords or a significant distance below the true vocal cords. If the stent is placed directly under the true vocal cords, granulation tissue can form and scarring of the glottis can occur; if at all possible, avoid this problem because repair and correction of glottic stenosis is difficult.
Trachea
In infants, the trachea is short. Thus, a tracheotomy tube can often stent the airway open itself, occasionally almost down to the carina. If this does not suffice, then other corrective measures must be performed for tracheomalacia in an infant.
Contraindications
Larynx
Absolute contraindications for use of a laryngeal stent include patients who are medically unstable and not able to undergo general anesthesia or individuals who may have an allergic reaction to the material of a particular stent.
Relative contraindications include risks of particular stents in various patients that could result in a poor outcome or complications. Historically, concern has been voiced regarding use of the Montgomery T-tube in young children (see Montgomery stent).
Trachea
Absolute and relative contraindications for tracheal stents are similar to contraindications listed for laryngeal stents; however, tracheal stents are often used as a last resort to prevent death by asphyxiation when other measures have failed or are not feasible. Another relative contraindication is the placement of a nonabsorbable stent when other techniques are available.
-
Note the diamond-shaped internal intraluminal component. The shape of the rib is seen on the reverse side of the carved-out diamond-shaped wound.
-
Another anterior graft with a diamond shape. Note that it is approximately 1.7 mm long. Again, the intraluminal site is seen facing up.
-
Laryngeal keel.
-
Representative (noninclusive) sample demonstrating various sizes of Aboulker stents, ranging from 15 mm in diameter on the left to 3 mm in diameter on the right. These stents are hollow and coated with Teflon.
-
An end view of an Aboulker stent, showing the central opening. These stents are hollow and coated with Teflon.
-
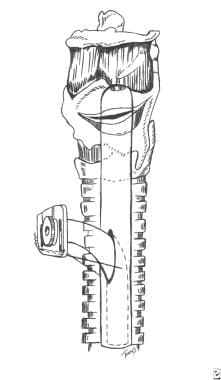
Side view of a Montgomery laryngeal stent.
-
Radiographic lateral neck view of a long stent connected to a metal Jackson tracheotomy tube at the bright inferior portion of the picture. The stent is seen in the airway as an oblong translucent area, with a rim of opacification around it that extends up through the larynx. A thin wire is seen connecting the stent and the tracheotomy tube.
-
A long Aboulker stent wired to a metal Jackson tracheotomy tube.
-
A Jackson tracheotomy tube wired to a long Aboulker stent.
-
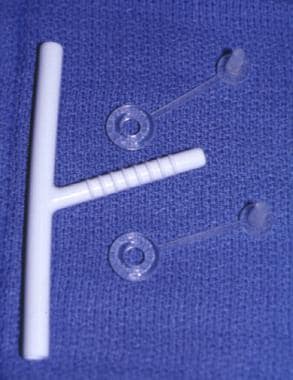
Montgomery T-tube (7 mm) stent with caps.
-
Intraoperative picture showing a solid dissolvable airway stent next to a trachea in a 3-kg New Zealand white rabbit.
-
Solid spiral dissolvable stent produced for the trachea of a rabbit. Scale is in centimeters.
-
Roll of silastic sheeting.
-
The Dumon stent with its opening for the right mainstem bronchus.
-
Palmaz stent expanded over a balloon superiorly and unexpanded inferiorly.
-
Balloon-expanded Palmaz stent placed into a pediatric airway under fluoroscopic guidance.
-
Endoscopic view of a deployed Palmaz stent. The carina is seen distal.
-
Strecker stent in different stages of deployment.
-
Gianturco-Z stent.
-
Metallic Wallstent.
-
Nitinol stent. The stent is loaded in the upper catheter and then expanded in the lower.
-
The Dumon stent.
-
A bifurcated dynamic airway stent. The stent is shown loaded on its delivery device inferiorly and in its open position in the airway above.