Overview
Universal screening programs have been implemented across the United States. Hearing loss occurs often enough in the general population to justify the legislation for universal hearing screening programs across the United States.
Hearing loss is one of the most common congenital anomalies, occurring in approximately 2-4 infants per 1000. Prior to implementation of universal newborn screening, testing was conducted only on infants who met the criteria of the high-risk register (HRR). It was found that the HRR was not enough, given that as many as 50% of infants born with hearing loss have no known risk factors. Reliable screening tests that minimize referral rates and maximize sensitivity and specificity are now readily available.
Early identification and intervention can prevent severe psychosocial, educational, and linguistic repercussions. Infants who are not identified before 6 months of age have delays in speech and language development. Intervention at or before 6 months of age allows a child with impaired hearing to develop normal speech and language, alongside his or her hearing peers.
A study from the Centers for Disease Control and Prevention (CDC) found that in the United States between 2006 and 2012, in newborns screened for hearing loss, the rate of hearing impairment diagnoses for those who did not pass their final screening test rose from 4.8% to 10.3%, while the rate of enrollment in early intervention services among children diagnosed with hearing loss grew from 55.4% to 61.7%. According to the study, however, reporting is inconsistent with regard to diagnostic test results (as opposed to screening results) and enrollment in early intervention. [1]
A study by Neumann et al involving 158 countries (containing nearly 95% of the world’s population) indicated that approximately 38% of infants are born in countries where newborn and infant hearing screening (NIHS) is minimal or absent. In addition, less than a third of newborns and infants were found to be enrolled in universal NIHS programs than encompass 85% of more of a region or country’s babies. [37]
See Table 1 below for common misconceptions held by the public about hearing loss and its identification in infants. Universal newborn hearing screening is essential to the normal speech and language development in the large number of infants born with hearing loss in the United States each year.
Table 1. Common Misconceptions Held by the Public and the Clinical Facts (Open Table in a new window)
Misconception |
Clinical Fact |
Parents will know if their child has a hearing loss by the time their child is 2-3 months of age. |
Prior to the universal screening, the average age at which children were found to have a hearing loss is 2-3 years. Children with mild-to-moderate hearing loss were often not identified until 4 years of age. |
Parents can identify a hearing loss by clapping their hands behind the child's head. |
Children can compensate for a hearing loss. They use visual cues, such as shadows or parental expressions and reactions, or they may feel the breeze caused by the motion of the hands. |
The HRR is all that is needed to identify children with hearing loss. |
The HRR misses approximately 50% of all children with hearing loss. |
Hearing loss does not occur often enough to justify the use of universal screening programs. |
Hearing loss affects approximately 2-4 per 1000 live births, and it has been estimated to be one of the most common congenital anomalies. |
Tests are not reliable and cause too many infants to be referred to specialists. |
Referral rates are as low as 5-7%. |
There is no rush to identify a hearing loss. The loss does not need to be identified until a child is aged 2-3 years. |
Children identified when they are older than 6 months can have speech and language delays. Children identified when they are younger than 6 months do not have these delays and are equal to their hearing peers in terms of speech and language. |
Children younger than 12 months cannot be fitted with hearing aids. |
Children as young as 1 month of age can be fit with and benefit from hearing aids. |
An image depicting newborn hearing screening can be seen below.
Prevalence of Hearing Loss
The ability to hear during the early years of life is critical for the development of speech, language, and cognition.
Retrospective studies of large universal newborn hearing screening programs have shown that permanent hearing loss is one of the most common abnormalities present at birth. In 1999, the American Academy of Pediatrics Task Force on Newborn and Infant Hearing stated, "significant bilateral hearing loss has been shown to be present in approximately 1 to 3 per 1000 newborns in the well-baby nursery population, and in approximately 2 to 4 per 1000 infants in the intensive care unit population." [2] Data from the newborn hearing-screening programs in Rhode Island, Colorado, and Texas show that 2-4 of every 1000 neonates have hearing loss (see Table 2 below). [3, 4, 5] A retrospective study conducted by Connolly et al in 2005 found that 1 of every 811 infants without risk factors and 1 of every 75 infants with risk factors have hearing loss. [6]
In the aforementioned study by Neumann et al, NIHS programs found the prevalence of infant permanent childhood hearing loss to range internationally from 0.3–15.0 cases (median 1.70) per 1000 infants. [37]
Table 2. Studies Regarding the Prevalence of Hearing Loss in Newborns (Open Table in a new window)
Investigator, Year |
State |
Rate of Hearing Loss |
Study Population |
Connolly, 2005 [6] |
Mississippi |
1.00 / 811 (no risk) 1.00 / 75 (high risk) |
17,602 |
Finitzo, 1998 [5] |
Texas |
3.14 / 1000 |
54,228 |
Vohr, 1998 [3] |
Rhode Island |
2.00 / 1000 |
53,121 |
Downs, 1995 [4] |
Colorado |
3.20 / 1000 |
14,404 |
The prevalence of hearing loss has been shown to be greater than that of most other diseases and syndromes (eg, phenylketonuria, sickle cell disease) screened at birth. The occurrence of hearing loss has been estimated to be more than twice that of other screenable newborn disorders combined (see Table 3 below).
Table 3. Prevalence of Metabolic Disorders Screened at Birth in Texas* (Open Table in a new window)
Disorder |
Rate per 100,000 |
Adrenal hyperplasia |
2 |
Galactosemia |
2 |
Phenylketonuria |
3 |
Hypothyroid disease |
28 |
Sickle cell disease |
47 |
*Finitzio, 1999 |
|
In the at-risk population, which includes neonates who spend time in the newborn intensive care unit (NICU), the occurrence of hearing loss is even higher. Risk factors for hearing loss specifically found in this population include, but are not limited to, use of high frequency ventilation, hyperbilirubinemia, low birth-weight, and exposure to ototoxic medications. [7] While these infants are at-risk for hearing loss at birth, studies have shown increased risk in this population for progressive and/or late-onset hearing loss. In a comprehensive study of extremely low birth-weight children, the incidence and severity of hearing impairment increased significantly from 5% to 13% (P=0.01) over a 24-year period. As these infants are identified as being at-risk for progressive or late-onset hearing loss, it is essential that they are not only screened at birth, but are followed regularly for audiological assessment and are not lost to follow-up. [8]
The High-Risk Register
Prior to the implementation of universal newborn hearing screening, only infants identified as being at high risk for hearing loss on the basis of the high-risk register (HRR) were routinely screened. According to the Joint Committee on Infant Hearing (JCIH) 2000 Position Statement, the risk factors for newborns are as follows: [9]
-
Family history of permanent childhood sensorineural hearing loss
-
In utero infection such as cytomegalovirus, rubella toxoplasmosis, or herpes
-
Craniofacial anomalies, including those with morphological abnormalities of the pinna and ear canal
-
Neonatal indicators, specifically hyperbilirubinemia at a serum level requiring exchange transfusion, persistent pulmonary hypertension of the newborn (PPHN) associated with mechanical ventilation, and conditions requiring the use of extracorporeal membrane oxygenation (ECMO)
-
Postnatal infections associated with sensorineural hearing loss, including bacterial meningitis
-
Stigmata or other findings associated with a syndrome known to include a sensorineural or conductive hearing loss or eustachian tube dysfunction
-
Syndromes associated with progressive hearing loss such as neurofibromatosis, osteopetrosis, and Usher syndrome
-
Neurodegenerative disorders, such as Hunter syndrome, or sensory motor neuropathies, such as Charcot-Marie-Tooth syndrome
-
Parental or caregiver concern regarding hearing, speech, language, and/or developmental delay
-
Head trauma
-
Recurrent or persistent otitis media with effusion lasting for at least 3 months
Use of the HRR as the primary indicator for screening of newborns for hearing loss was inadequate. In 1999, Finitzio and Crumley reported that, according to the identification rates currently reported from widespread screening programs, approximately 8,000-16,000 newborns are born with hearing loss each year. [10] Of these, 50% are discharged home from the well-baby nursery with no known risk factors for hearing loss, according to the National Institutes of Health (NIH). [11] Although these risk factors should not be ignored, a program in which only neonates meeting the HRR criteria are screened was found to exclude as many as 50% of newborns with significant congenital hearing loss.
In addition, an Australian study found that the ages of diagnosis of congenital hearing loss following universal newborn screening, risk factor screening, and opportunistic screening were 8.1, 16.2, and 22.5 months, respectively. [12]
An updated HRR is still used to identify children who are at risk for hearing loss. All newborns should be screened, regardless of risk. If a newborn passes the newborn hearing screening but has an identified risk for sensorineural and/or conductive hearing loss, these infants should be closely monitored for any changes in hearing status. Many states recommend that at-risk children should be evaluated by an audiologist every 6 months for the first 3 years of life. This helps to quickly identify hearing status changes so that intervention can occur, limiting any impact the hearing loss has on speech and language development.
Efficacy of Early Identification and Intervention
As recently as 1988, the age at which hearing loss was identified in children in the United States was estimated to be 2.5 years. Although children who had severe-to-profound hearing loss or multiple disabilities were identified at or before age 2.5 years, children with mild-to-moderate hearing loss were often not identified until school age. [9] The implementation of universal hearing screening programs is beginning to lower this age. A study conducted by Connolly et al in 2005 indicated that, as a result of the universal newborn hearing screening program in place from 1997-2001, the mean age of diagnosis was 3.9 months, with a mean age of intervention of 6.1 months. [6]
Children with hearing loss typically experience significant delays in language development and academic achievement. Although the impact of a severe or profound hearing loss is well recognized, children with mild or moderate hearing loss also experience deficits in speech and language development. Studies have shown that hearing-impaired high school graduates have significantly lower average reading scores than those of their hearing peers, with deaf and hard-of-hearing students scoring at the fourth or fifth grade level.
The definition of early identification and intervention has evolved over the years. In the recent past, early identification was defined as intervention before the age of 18 months. The implementation of universal screening programs throughout the United States has caused the definition of early identification and intervention to be re-examined. Early identification can now be defined as diagnosis as early as age 3 months, with intervention by age 6 months. In 1994, Bess and Paradise challenged the need for earlier identification and intervention, stating that no evidence support the notion "that outcomes in children with congenital hearing loss are more favorable if treatment is begun early in infancy rather than later in childhood." [13] Since then, many groups have refuted this statement.
In 1987, White and White reported that, in severely and profoundly deaf children, language scores were significantly better in those whose hearing loss was identified at an average age of 11.9 months, compared with scores in those whose loss was identified at an average age of 19.5 months. [14]
In 1995, Apuzzo and Yoshinaga-Itano found that infants identified when they were younger than 2 months had significantly higher language scores than those identified when they were older than 2 months, despite similar interventions in both groups. [15] In 1995, Robinshaw reported that children who were identified and who wore hearing aids by the age of 6 months acquired age-appropriate vocal communicative and linguistic skills well before children who were identified at a later age. [16]
Although all of the above studies demonstrate the importance of early identification and intervention, a study conducted in 1998 at the University of Colorado truly established the critical period of early identification and intervention, namely, younger than 6 months. [17, 18] In 1998, Yoshinaga-Itano and Sedey et al compared receptive and expressive language abilities in children with various degrees of hearing impairment with those of children with no hearing loss. Significant findings were as follows:
-
Children with hearing loss that is identified by age 6 months had significantly higher receptive, expressive, and total language quotients than those of children identified at 7-12, 13-18, 19-24, and 25-34 months.
-
This statistical difference was independent of the following demographic variables: age, sex, ethnicity, communication mode, degree of hearing loss, socioeconomic status, and presence or absence of other disabilities.
-
No significant differences in language ability were found among groups of children who were identified when they were older than 6 months.
In other words, even children identified as early as age 7-12 months had lower receptive and expressive language quotients than those of children identified by age 6 months. No significant difference was found between children identified at age 7-12 months and those identified at age 25-30 months.
The importance of early identification and intervention has been clearly demonstrated. Identification and intervention before age 6 months can have a significant impact on the development of expressive and receptive language. The finding that language scores were not significantly different between the children identified later truly establishes the critical period of early identification and intervention to be within the first 6 months of life.
Legislation
Healthcare professionals have long supported the need for early identification and intervention in infants and children with hearing loss. The main goal of early identification and intervention programs is to improve the speech and language development of infants and children who are deaf or hard of hearing, thereby improving their academic and vocational achievements. Although the need for successful universal newborn hearing screening programs cannot be denied, the legislative support, technology, and expertise needed to implement such programs on a national level has only recently been realized.
Following the Individuals with Disabilities Education Act of 1989, the Rhode Island Hearing Assessment Project (RIHAP) was developed in 1990 through funding from the US Department of Education and the US Public Health Service. This project was designed to systematically evaluate the effectiveness of transient evoked otoacoustic emissions (TEOAEs) in screening newborns for hearing loss.
In 1994, the Joint Committee on Infant Hearing (JCIH) released a position statement endorsing the goal of universal identification of infants with hearing loss as early as possible, with early identification by age 3 months and intervention by age 6 months. [19] In 2000, the JCIH modified the high-risk register (HRR) to aid in the identification of newborns at high risk for permanent hearing loss, particularly those at risk for progressive hearing loss, through age 2 years. [20] The JCIH 2000 Position Statement was designed to meet the goals of Healthy People 2000 (US Department of Health and Human Services Public Health Service, 1990) and 2010 (US Department of Health and Human Services, 2000), the 1993 NIH Consensus Statement, and the American Academy of Audiology position statement. [21, 11] The American Academy of Pediatrics endorsed this position statement.
Although all of these position statements support the need for early identification and intervention in infants with hearing loss, recommendations from both the JCIH and the American Academy of Audiology include the screening of all newborns for hearing loss prior to their discharge home from birthing hospitals.
The implementation of statewide systems for the universal hearing screening of newborns is gaining momentum. Currently, legislation for newborn hearing screening has been passed in many states. In some states, legislation has not passed but voluntary newborn hearing screenings are performed at most birthing hospitals.
The following states passed legislation for universal screening of hearing in newborns in the years indicated:
-
Alabama - 2008
-
Alaska - 2006
-
Arizona - 2005
-
Arkansas - 1999
-
California - 1998
-
Colorado - 1997
-
Connecticut - 1997
-
District of Columbia - 2001
-
Florida - 2000
-
Georgia - 1999
-
Hawaii - 1990
-
Illinois - 1999
-
Indiana - 1999
-
Iowa - 2003
-
Kansas - 1999
-
Kentucky - 2000
-
Louisiana - 1999
-
Maine - 1999
-
Maryland - 1999
-
Massachusetts - 1997
-
Michigan - 2002
-
Mississippi - 1997
-
Missouri - 1999
-
Montana - 2001
-
Nebraska - 2000
-
Nevada - 2000
-
New Hampshire - 2000
-
New Jersey - 2000
-
New Mexico - 2001
-
New York - 1999
-
North Carolina - 1999
-
Ohio - 2002
-
Oklahoma - 2000
-
Oregon - 1999
-
Pennsylvania - 2001
-
Rhode Island - 1992
-
South Carolina - 2000
-
Tennessee - 2008
-
Texas - 1999
-
Utah - 1998
-
Virginia - 1998
-
West Virginia - 1998
-
Wisconsin - 1999
-
Wyoming - 1999
The new JCIH 2007 Position Statement was released in early October 2007. [22] The following is a list of some of the significant changes from the previous statement:
The definition of targeted hearing loss was expanded to include neural hearing loss (eg. auditory neuropathy/dyssynchrony).
Separate protocols are recommended for neonatal intensive care units (NICUs) and well-baby nurseries. Auditory brainstem response screenings are recommended for all NICU babies, as well as babies admitted for greater than 5 days, so that neural hearing loss will not be missed.
Referrals should be made directly to an audiologist for comprehensive testing to include diagnostic auditory brainstem response (ABR) for all infants who do not pass ABR screening in the NICU.
Rescreening of all infants should include re-evaluation of both ears, even if the infant only failed one ear in the initial screening.
Audiologists with expertise in evaluating newborns should conduct diagnostic evaluations.
Children identified with hearing loss should be fit with amplification within 1 month of diagnosis.
A genetics consultation should be offered to families of infants diagnosed with hearing loss.
All children identified with hearing loss should undergo an evaluation by an otolaryngologist and have at least one examination to assess visual acuity with a pediatric ophthalmologist.
All children with any degree of bilateral or unilateral hearing loss should be considered eligible for early intervention services.
Families should be made aware of all communication options and available hearing technologies (presented in an unbiased manner).
Early intervention services should be provided by professionals with expertise in hearing loss.
Based on data from 134 children, a study by Ghogomu et al indicated that institution of a universal newborn hearing screening program in Missouri reduced the mean age of detection of pediatric unilateral sensorineural hearing loss from 4.4 years to 2.6 years and increased the rate at which such hearing loss is detected by age 6 months from 3% to 42%. [23] According to a study involving patients at a pediatric teaching hospital in Canada, universal newborn hearing screening lowered the median age at which mild bilateral or unilateral hearing loss was detected from 5 years to 0.8 years. [24]
Methods of Screening
Auditory brainstem response (ABR), otoacoustic emissions (OAEs), and automated ABR (AABR) testing have all been used in newborn hearing-screening programs. For 20 years, manual or diagnostic ABR testing has been a reliable means of assessing auditory function from the eighth nerve through the auditory brainstem. A modified screening version of the ABR test, called the AABR test, has been available for screening since approximately 1987. The discovery of OAEs by David Kemp in 1978 allowed the development of an alternative screening technology that has become commonplace in hospitals across the nation. [25] The 2 methods used in most universal hearing-screening programs are automated OAEs and AABR. Behavioral audiometry is not sufficiently sensitive or specific for use in a screening program.
Otoacoustic emissions
OAEs are used to assess cochlear integrity and are physiologic measurements of the response of the outer hair cells to acoustic stimuli. They serve as a fast objective screening test for normal preneural cochlear function. To measure OAEs, a probe assembly is placed in the ear canal, tonal or click stimuli are delivered, and the OAE generated by the cochlea is measured with a microphone.
Currently, 2 types of evoked OAE measurements are used for newborn hearing screening: transient evoked otoacoustic emissions (TEOAEs) and distortion product otoacoustic emissions (DPOAEs). Provided that the patient's middle ear function is normal, these measurements can be used to assess cochlear function for the 500-6000 Hz frequency range. The presence of evoked OAE responses indicates hearing sensitivity in the normal to near-normal range. [26]
OAEs are fast, efficient, and frequency-specific measurements of peripheral auditory sensitivity. However, the effectiveness of the test is reduced by contamination with low-frequency ambient noise in a busy nursery, vernix in the ear canal, or any middle ear pathology.
OAEs are not a sufficient screening tool in infants who are at risk for neural hearing loss (eg, auditory neuropathy/dyssynchrony). Any infant in the NICU or in the hospital for more than 5 days should undergo an ABR screening so that the presence of auditory neuropathy is not missed. Cochlear function, and therefore OAE measurements, are usually normal in infants and children with this type of hearing loss.
Automated auditory brainstem response
AABR is an electrophysiologic measurement that is used to assess auditory function from the eighth nerve through the auditory brainstem. AABR measurements are generally obtained by placing disposable surface electrodes high on the forehead, on the mastoid, and on the nape of the neck (see the image below). The click stimulus (usually set at 35 dB hearing level [HL]) is delivered to the infant's ear via small disposable earphones designed to attenuate background noise. Most AABR systems compare an infant's waveform with that of a template developed from normative ABR infant data. A pass or fail response is determined from this comparison. Most commercially available systems can be used as an effective screening tool in infants younger than 6 months.
The AABR method produces a simple pass or fail result without requiring interpretation, and the test can be conducted in the presence of background noise. However, it lacks frequency-specific information and requires increased preparation time prior to testing.
The AABR test is solely a screening technique designed to identify infants who require follow-up testing. It cannot be used to determine the degree or nature of the hearing loss.
A study by Johnson et al reported that in healthy newborns, failure rates for AABR evaluation were lower when testing was delayed. The AABR failure rate in newborns tested less than 24 hours postnatally was 13.3%, compared with 3.8% in those tested at or after 48 hours. The investigators also found a greater repeat testing failure rate among infants who underwent initial AABR testing at age 36 hours or above than among those who were initially tested earlier. Moreover, 18.6% of neonates who failed a final AABR screening test at age 48 hours or older were diagnosed with sensorineural hearing loss, while this diagnosis was made in just 2.8% of those whose final screening took place prior to 48 hours. [27]
Diagnostic auditory brainstem response
Diagnostic ABR testing is generally not used in universal newborn hearing screening programs because of the length of the procedure, the cost, and the need for an audiologist to perform the test and interpret the results. Like AABRs, diagnostic ABRs are electrophysiologic measurements that reflect auditory function from the eighth nerve through the auditory brainstem.
ABR recordings are generally obtained by placing disposable surface electrodes on the forehead and on both mastoids. Responses are typically measured from the forehead to the ipsilateral mastoid. ABR waveforms are obtained in response to abrupt click stimuli delivered in rapid pulse trains through insert earphones.
Unlike the AABR test, which elicits a response to a fixed 35-dB HL click, the intensity of the stimulus is varied in the manual ABR test to determine the lowest level required to evoke a clear and repeatable response. This form of ABR testing allows the audiologist to determine not only the severity of the hearing loss but also the nature of the hearing loss (ie, sensorineural, conductive, or neural) by using both air and bone conduction stimulation. When a click is used to evoke the ABR, information regarding hearing sensitivity is restricted to approximately 1000-4000 Hz. If necessary, an ABR can be elicited by tone burst stimulation to determine the configuration of a hearing loss.
The ABR is not used to assess hearing in a perceptual sense; rather, it helps in evaluating the integrity of the peripheral auditory system from which estimates of hearing can be derived.
Diagnostic ABR tests can be used to determine the degree of hearing loss and also the nature of the loss. However, they are not efficient for a screening program. ABR techniques should be used for follow-up diagnostic procedures.
Follow-up testing
Infants who do not pass an initial hearing screening at birth should return for follow-up testing within 1 month. This follow-up allows for multiple testing sessions, medical intervention, parent counseling, and appropriate amplification measures to be initiated before the age of 6 months. The goal for identification and intervention by 6 months is important for language development, and diagnosis before this critical age can prevent the need for sedation. As the age of an infant increases, the ability to obtain a full diagnostic test battery decreases. If follow-up is delayed, sedation may be required in order to obtain electrophysiological measures.
Diagnostic OAE and ABR testing is recommended for any infant who does not pass the second screening session. Both tests are necessary to differentially diagnose an infant's hearing impairment. OAE tests are used to assess the outer, middle, and inner ear portions of the auditory system. ABR testing helps in assessing the whole system, from the periphery to the auditory nerve and brainstem (see Table 4). Traditionally, diagnostic ABR results differentiate between conductive loss and sensorineural loss.
However, with the addition of OAEs, separating a purely sensory loss, which occurs in the cochlea, from a purely neural loss is now possible. For example, an infant may have an abnormal ABR with normal OAEs. This type of neural hearing loss is known as auditory neuropathy, or auditory dyssynchrony, and has been described by Sininger and Starr in 2001. [28]
If a child is identified with a hearing loss, another specialized test may be necessary to obtain frequency-specific information in order to amplify appropriately. This frequency-specific information can be obtained by conducting either tone burst–evoked ABR or by auditory steady-state response testing (ASSR). ASSR has been found to be a very useful tool for providing discrete, frequency-specific information, especially in the presence of moderate-to-profound hearing loss. [20]
The following audiologic test battery should be conducted on any infant identified with hearing loss: air conduction ABR, bone conduction ABR, high-frequency tympanometry, otoacoustic emissions, acoustic stapedial reflexes, tone burst ABR and/or ASSR, and behavioral audiometry (when appropriate) to assess functional hearing. Reversing polarity during all diagnostic air conduction ABR testing should also be conducted to ensure that the response is truly neural and to rule out auditory neuropathy. The comprehensive diagnostic information obtained from the full test battery is beneficial when a plan for intervention and amplification is implemented. This information provides medical caregivers with a total picture of the patient's auditory function, from the peripheral sensory structures through the brainstem.
Table 4. Assessment of the Auditory System by OAEs and ABRs/AABRs (Open Table in a new window)
Auditory Structure |
OAEs |
ABRs/AABRs |
Outer ear |
Yes |
Yes |
Middle ear |
Yes |
Yes |
Inner ear |
Yes |
Yes |
Auditory nerve |
No |
Yes |
Auditory brainstem |
No |
Yes |
Sensitivity and Specificity
The goal of any infant hearing screening program is to achieve a high level of both sensitivity and specificity. The ideal program should permit the identification of as many newborns as possible who do have a hearing loss (high sensitivity) and also to exclude as many newborns as possible who do not have a hearing loss (high specificity). With these goals in mind, the NIH Consensus Statement recommends that all screening programs should have a failure rate of no more than 5-7%, and the number of referrals be kept to a minimum. [11] In 2004, Hall, Smith, and Popelka reported an estimated sensitivity at 100%, specificity at 99.7%, overall referral rate of 2.0% and a positive predictive value of 83.3% in a study comprised of 300 infants. [29]
While AABR has been used for years on infants falling under the high-risk register (HRR), OAE screening has been shown to be a highly cost-effective tool. Several papers have described a combined AABR and OAE screening technique as an effective tool for maintaining low referral rates. [30, 31, 32, 33]
Programs in Rhode Island, Texas, and Colorado have demonstrated that a referral rate of 5-7% is obtainable. The TEOAE-based program in Rhode Island reported a higher average referral rate of 10% over a 4-year period. [3] Using AABR testing, the Colorado program reported a referral rate of 5%, whereas Texas hospitals achieved a 3.4% referral rate. [4, 5] Hospitals in Texas that used a 2-technology procedure of OAE testing followed by AABR testing had an average failure rate of 3% (see the image below). In a 2004 report, Hall, Smith, and Popelka suggest that a 2-stage approach can serve as a crosscheck to evaluate each type of testing. [29] A 2-stage AABR protocol used in Mississippi from 1997-2001 yielded a referral rate of 4.1% and a false-positive rate of 3.6%. [6] Some studies indicate that a 2-stage protocol may have a slightly higher referral rate than AABR alone, but a significant increase in referrals with TEOAEs and/or DPOAEs alone continued. [34]
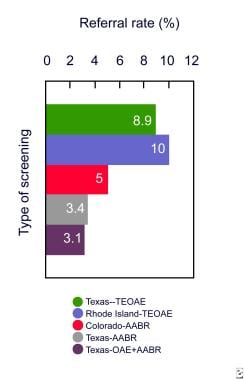 Referral rates of screening programs in Texas, Colorado, and Rhode Island. Texas referral rates are broken down by method used at 9 hospitals. In Texas with transient evoked otoacoustic emission (TEOAE) testing, n = 2,732; Rhode Island, n = 53,121; Colorado, n = 14,494; Texas with automated auditory brainstem response (AABR) testing, n = 3,016; and Texas with otoacoustic emission (OAE) and AABR, n = 11,357.
Referral rates of screening programs in Texas, Colorado, and Rhode Island. Texas referral rates are broken down by method used at 9 hospitals. In Texas with transient evoked otoacoustic emission (TEOAE) testing, n = 2,732; Rhode Island, n = 53,121; Colorado, n = 14,494; Texas with automated auditory brainstem response (AABR) testing, n = 3,016; and Texas with otoacoustic emission (OAE) and AABR, n = 11,357.
Referral rates will always vary depending on the method of screening used in the program. This variation must be kept in mind when a protocol for screening is established. Referral rates are often higher initially, at the onset of a screening program, but they tend to decrease with experience. Given the increased understanding and identification of auditory neuropathy, an AABR screening protocol is recommended in the NICU setting and with any other at-risk infants. Although OAE screening continues to be cost effective in the well-baby nursery, OAE screening followed by AABR is a reliable protocol that results in low referral rates.
Conclusions
The identification of all newborns with hearing loss before age 6 months has now become an attainable realistic goal. In the past, parents and pediatricians often did not suspect a hearing loss until the age of 2-3 years, after important speech and language milestones have not been met. By the time these milestones are missed, the hearing-impaired child has already experienced irreversible delays in speech and language development.
Based on information from 48 separate Early Hearing Detection and Intervention Information Systems (EHDI-IS), Sanchez-Gomez et al evaluated the quality of newborn hearing screening data around the United States. The results showed the need to improve the accuracy and completeness of demographic information among state EHDI programs. Moreover, it was found that hearing screening results were sometimes missing for infants admitted to the neonatal intensive care unit (NICU) or transferred from one birthing facility to another, owing to a lack of clarity among some birthing facilities regarding how to document such results for these patients. [35]
-
An infant's hearing is screened by measuring the automated auditory brainstem response (AABR).
-
Referral rates of screening programs in Texas, Colorado, and Rhode Island. Texas referral rates are broken down by method used at 9 hospitals. In Texas with transient evoked otoacoustic emission (TEOAE) testing, n = 2,732; Rhode Island, n = 53,121; Colorado, n = 14,494; Texas with automated auditory brainstem response (AABR) testing, n = 3,016; and Texas with otoacoustic emission (OAE) and AABR, n = 11,357.







