Background
Thyroid storm, also referred to as thyrotoxic crisis, is an acute, life-threatening, hypermetabolic state induced by excessive release of thyroid hormones (THs) in individuals with thyrotoxicosis. Thyroid storm may be precipitated by the stress of surgery, anesthesia, or thyroid manipulation and may be prevented by pretreatment with antithyroid drugs (ATDs). [1] Improved preoperative management has markedly decreased the incidence of this complication. [2] Today, thyroid storm occurs more commonly as a medical crisis rather than a surgical crisis.
Heat intolerance and diaphoresis are common in simple thyrotoxicosis but manifest as hyperpyrexia in thyroid storm. Extremely high metabolism also increases oxygen and energy consumption. Cardiac findings of mild-to-moderate sinus tachycardia in thyrotoxicosis intensify to accelerated tachycardia, hypertension, high-output cardiac failure, and a propensity to develop cardiac arrhythmias. Similarly, irritability and restlessness in thyrotoxicosis progress to severe agitation, delirium, seizures, and coma. GI manifestations of thyroid storm include diarrhea, vomiting, jaundice, and abdominal pain, in contrast to only mild elevations of transaminases and simple enhancement of intestinal transport in thyrotoxicosis.
Diagnosis is primarily clinical, and no specific laboratory tests are available. Patients with a Burch–Wartofsky Point Scale (BWPS) of ≥45 or Japanese Thyroid Association (JTA) categories of thyroid storm 1 (TS1) or thyroid storm 2 (TS2) with evidence of systemic decompensation require aggressive therapy. The decision to use aggressive therapy in patients with a BWPS of 25–44 is based on clinical judgment. [1]
According to the guidelines of the American Thyroid Association (ATA), a multimodality treatment approach should be individualized to the patient and includes β-adrenergic blockade, ATD therapy, inorganic iodide, corticosteroid therapy, cooling with acetaminophen and cooling blankets, volume resuscitation, nutritional support, respiratory care, and monitoring in an intensive care unit. [1]
ATA guidelines also recommend that patients undergoing thyroidectomy be rendered euthyroid with methimazole preoperatively and that potassium iodide (KI) be given in the immediate preoperative period. The recommendation to render patients euthyroid with antithyroid medication is an effort to reduce the risk of thyroid storm that the stress of surgery could precipitate. KI is recommended to reduce thyroid gland vascularity with the goal of improving operative visualization and reducing operative complications. [1]
Pathophysiology
Thyroid storm is a decompensated state of thyroid hormone–induced, severe hypermetabolism involving multiple systems and is the most extreme state of thyrotoxicosis. The clinical picture relates to severely exaggerated effects of thyroid hormones (THs) due to increased release (with or without increased synthesis) or, rarely, increased intake of TH. [3]
Although the exact pathogenesis of thyroid storm is not fully understood, the following theories have been proposed:
-
Patients with thyroid storm reportedly have relatively higher levels of free THs than patients with uncomplicated thyrotoxicosis, although total TH levels may not be increased.
-
Adrenergic receptor activation is another hypothesis. Sympathetic nerves innervate the thyroid gland, and catecholamines stimulate TH synthesis. In turn, increased THs increase the density of beta-adrenergic receptors, thereby enhancing the effect of catecholamines. The dramatic response of thyroid storm to beta-blockers and the precipitation of thyroid storm after accidental ingestion of adrenergic drugs such as pseudoephedrine support this theory. This theory also explains normal or low plasma levels and urinary excretion rates of catecholamines; however, it does not explain why beta-blockers fail to decrease TH levels in thyrotoxicosis.
-
Another theory suggests a rapid rise of hormone levels as the pathogenic source. A drop in binding protein levels, which may occur postoperatively, might cause a sudden rise in free hormone levels. In addition, hormone levels may rise rapidly when the gland is manipulated during surgery, during vigorous palpation during examination, or from damaged follicles following RAI therapy.
-
Other proposed theories include alterations in tissue tolerance to THs, the presence of a unique catecholaminelike substance in thyrotoxicosis, and a direct sympathomimetic effect of TH as a result of its structural similarity to catecholamines.
Etiology
A precipitating factor usually is found with thyroid storm. Presently, the most common cause of thyroid storm is intercurrent illness or infection. [4, 5]
Some causes of rapidly increased thyroid hormone levels include the following:
-
Surgery, thyroidal or nonthyroidal
-
Radioiodine therapy
-
Withdrawal of antithyroid drug therapy
-
Vigorous thyroid palpation
-
Iodinated contrast dye
-
Thyroid hormone ingestion
Other common precipitants include the following:
-
Infection
-
Emotional stress
-
Tooth extraction
-
Diabetic ketoacidosis
-
Hypoglycemia
-
Trauma
-
Bowel infarction
-
Parturition
-
Toxemia of pregnancy
-
Pulmonary embolism
-
Cerebrovascular accident
-
Gestational trophoblastic disease
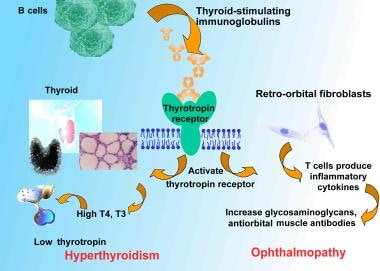
Although it can develop in toxic adenoma or multinodular toxic goiter, thyroid storm is more commonly seen in toxicity secondary to Graves disease. See the image below.
Epidemiology
United States statistics
Among 121,384 hospital discharges with thyrotoxicosis identified between 2004 and 2013, 19,723 (16.2%) were diagnosed with thyroid storm. [6] The incidence of thyroid storm is approximately 0.65 cases per 100,000 persons per year and 5.2 per 100,000 hospitalized patients per year. [6]
International statistics
In Japan, thyroid storm is a rare disorder occurring in approximately 1–5% of patients hospitalized for thyrotoxicosis. [4, 7]
Age- and sex-related demographics
Age and sex predilection depends on the etiology of thyrotoxicity. Graves disease more frequently develops in females (ie, male-to-female ratio ranges from 1:7 to 1:10); multinodular goiter more often manifests in the elderly population. In one study, the majority of patients with thyrotoxicosis were middle aged and white, and about 76% were female. [6]
Prognosis
Thyroid storm (TS) is an acute, life-threatening emergency. If untreated, thyroid storm is almost invariably fatal in adults (90% mortality rate). Death from thyroid storm may be a consequence of cardiac arrhythmia, congestive heart failure, hyperthermia, multiple organ failure or other factors, though the precipitating factor is often the cause of death.
With adequate thyroid-suppressive therapy and sympathetic blockade, clinical improvement should occur within 24 hours. Adequate therapy should resolve the crisis within a week. With treatment, mortality has been reported as 8-25%. [5, 8] In one retrospective study from Japan of 1324 patients who were diagnosed with thyroid storm, the following factors were associated with increased mortality risk in thyroid storm [9] :
-
Age 60 years or older
-
Central nervous system (CNS) dysfunction at admission
-
Lack of antithyroid drug and beta-blockade use
-
Need for mechanical ventilation and plasma exchange along with hemodialysis
In addition, CNS dysfunction of greater than mild severity appears to be a risk factor for mortality. [5, 8]
Complications
Cardiogenic shock (CS) is a rare complication of thyroid storm, which occurs more commonly in male patients with preexisting structural and atherosclerotic heart disease, and carries a very poor prognosis. In review of 41,835 patients with thyroid storm between 2003-2011, there was an increase in incidence of CS from 0.5% in 2003 to 3% in 2011 but a decrease in mortality from 60.5% in 2003 to 20.9% in 2011. The researches theorized that the decreased mortality rates were due to improved intensive care and increasing use of mechanical circulatory devices such as the intra-aortic balloon pump (IABP) and extra corporeal mechanical ventilation (ECMO). [10]
Patient Education
For patient education resources, see the Thyroid and Metabolism Center as well as Thyroid Problems, Thyroid Storm, and Graves Disease.
-
Pathophysiologic mechanisms of Graves disease relating thyroid-stimulating immunoglobulins to hyperthyroidism and ophthalmopathy. T4 is levothyroxine. T3 is triiodothyronine.