Practice Essentials
Squamous cell carcinoma (SCCA) of the aerodigestive tract is the most frequently encountered malignancy of the head and neck. Regional metastases to cervical lymph nodes are common. A patient with N3 disease of the neck is defined as having a lymph node measuring greater than 6 cm, which is categorized as having stage 4b disease regardless of primary site tumor size. Therefore, diagnosing an N3 neck must be supported by clinical or radiologic measurement of the node in accordance with nodal classifications of the American Joint Committee on Cancer (AJCC) and International Union Against Cancer.
Patients with distant metastasis have the worst prognosis, and, according to Spiro et al, patients with bilateral neck disease, fixed nodes, and level 5 nodes have a survival rate of less than 15%. [1] If the treatment goal is to cure the patient, the management strategy should be aggressive and multimodal.
The decision to treat the patient with an N3 neck or with stage 4b disease must be realistically weighed and supported with good data. The management decision must be individualized or tailored to each individual patient, as follows:
-
Patient - Medical condition and risk factors
-
Performance status and nutrition
-
Pathology - Histology, stage of the disease, location, extent of the disease, and resectability
-
Patient's realistic expectations
-
Procedure - Curative versus palliative
-
Post-treatment survival expectation, locoregional control rates, and quality of life
The above-mentioned parameters must be evaluated or optimized in a multidisciplinary approach to achieve the ultimate goal of either cure or palliation. The following are the treatment options:
-
Surgical resection of the primary tumor and neck dissection (if operable and resectable), followed by radiation or chemoradiation therapy
-
Concurrent chemoradiation therapy followed by planned neck dissection, regardless of nodal response (This option is applicable if the primary tumor has a complete response to chemoradiation therapy based on clinical examination, endoscopic examination, and biopsy of the primary lesion.) [2]
-
Concurrent chemoradiation therapy followed by surgical resection of persistent or recurrent disease [3]
Signs and symptoms of N3 neck disease
The following may be presenting symptoms:
-
Neck mass
-
Otalgia
-
Nerve deficit
-
Horner syndrome
-
Dysphagia
-
Airway obstruction
Workup in N3 neck disease
Laboratory studies
Laboratory studies should include the following:
-
Basic metabolic panel
-
Complete blood count (CBC)
-
Liver function tests
-
Prealbumin and albumin
-
Coagulation panel
-
Blood type and cross-match
-
P16 testing on biopsy specimen of oropharyngeal primary (surrogate test for human papillomavirus [HPV])
Imaging studies
Evaluation of N3 neck disease can be performed with the following modalities:
-
Computed tomography (CT) scan with contrast - Useful in determining resectability and the extent of the primary tumor and nodal disease
-
Magnetic resonance imaging (MRI) with gadolinium - Can demonstrate soft tissue changes and reveal perineural spread
-
Positron emission tomography (PET)–CT fusion study - May be helpful in patients who present with N3 nodes with an unknown primary tumor
Diagnostic procedures
These include the following:
-
Fine-needle aspiration biopsy (FNAB) of the neck mass - The only required test for the diagnosis
-
Open biopsy procedure - Necessary only if the diagnosis cannot be attained with FNAB and a lymphoma is suspected
-
Panendoscopy, including direct laryngoscopy, bronchoscopy, and esophagoscopy - Has classically been performed to assess the primary tumor and to identify the presence of synchronous primary tumors
Management of N3 neck disease
Medical therapy
Local control with chemoradiation therapy has been reported to be as high as 90%. Concurrent chemoradiation therapy has survival rates similar to those of surgical therapy and preserves the function of important structures. Surgical therapy, however, carries better locoregional control rates.
In the presence of a partial or incomplete response in the neck to chemoradiation, a completion neck dissection is mandatory (assuming the primary site is controlled or is resectable).
Surgical therapy
Surgery for a stage N3 neck should always be in conjunction with chemoradiation or radiation (performed either preoperatively or postoperatively).
Although a modified neck dissection may be possible in some cases, the classic radical neck dissection is necessary in most cases of the N3 neck.
The treatment options in the management of cervical metastasis that involves the carotid artery include the following:
-
Permanent occlusion can be performed if collateral circulation is adequate
-
Resection with carotid shunt and reconstruction can be performed if collateral circulation is inadequate
-
Nonsurgical palliation is an option if collaterals are inadequate and reconstruction is not possible
History of the Procedure
Surgery followed by radiation has long been the criterion standard treatment option for advanced stage squamous cell carcinoma (SCCA) of the head and neck. Treatment has consisted of resection of the primary site, radical neck dissection, reconstruction as needed, and postoperative radiotherapy. To minimize the morbidity of radical neck dissection, Bocca (1967) introduced the concept of modified radical neck dissection, preserving the sternocleidomastoid muscle, internal jugular vein, and spinal accessory nerve, when possible. [4]
However, a modified radical neck dissection is often not possible in the N3 neck. Given the potential morbidity associated with radical surgery, surgeons and oncologists alike began looking for nonsurgical options for treating advanced stage head and neck cancer. Many chemoradiation trials have been conducted, with the Department of Veterans Affairs Laryngeal Cancer Study Group (1991) trial beginning the push for nonsurgical treatment of advanced stage head and neck cancer. To this end, many centers consider organ preservation chemoradiation as the standard treatment for advanced stage head and neck cancer.
Problem
A patient with N3 disease of the neck is automatically categorized as having stage IVb disease, and the average 2-year survival rate, considering all head and neck sites, is approximately 20%. [1] Patients with N3 disease also have a high rate of distant metastasis, up to 30%. [5] In addition, both radical surgery and concurrent chemoradiation bring morbidity to the patient. The goal of treatment in most patients with this degree of disease is palliation, but cure may still be possible.
Epidemiology
Frequency
N3 neck disease is uncommon. The rate of patients presenting with the N3 neck ranges from 1.7-9.5% in large series. [1, 5, 6]
Etiology
Squamous cell carcinoma (SCC) arising from the aerodigestive tract is the most common cause of cervical metastases. Primary tumors of the major and minor salivary glands can also present with cervical lymphadenopathy. The histopathology of malignant salivary gland tumors that have frequent neck disease include high-grade mucoepidermoid carcinoma, squamous cell carcinoma, carcinoma ex-pleomorphic, and high-grade adenocarcinoma. Thyroid carcinomas also manifest with cervical metastases, most commonly from papillary or medullary thyroid carcinomas. In addition, lymphoma can present with bulky lymphadenopathy.
Pathophysiology
As mentioned previously, N3 neck disease usually results from squamous cell carcinoma arising from the aerodigestive tract. Although the disease usually involves only structures in the neck, depending on the location of the involved node, it may extend into surrounding structures such as the skull base, clavicles, or mediastinum. In addition, patients presenting with N3 neck disease are at high risk for distant metastases. The lungs (83.4%), bone (31.3%), and liver (6%) are the most common site of distant metastasis, although the brain and other sites have been reported in the surgical literature. [7]
Presentation
Aside from evaluation of the primary tumor, patients with an N3 neck disease present in the following clinical scenarios:
-
N3 neck disease that has not been treated
-
N3 neck disease after chemoradiation or radiation with no response or partial response
-
N3 neck disease after chemoradiation with complete response
-
N3 neck disease with unknown primary tumor
A complete head and neck examination is warranted to check the following:
-
Identify primary site
-
Fixation of mass around bone or paraspinal muscles
-
Skin involvement
-
Mediastinal spread
-
Contralateral neck
The following may be presenting symptoms:
-
Neck mass
-
Otalgia
-
Nerve deficit
-
Horner syndrome
-
Dysphagia
-
Airway obstruction
Indications
The goals of treatment include palliation, improved quality of life, and cure, if possible. If the tumor is histologically proven to be squamous cell carcinoma based on findings of either fine-needle aspiration (FNA) of lymph node or biopsy of the primary tumor, the factors that influence treatment include operability and resectability of the both the primary tumor and the neck, the presence of distant metastases, as well as the presence of synchronous second primary tumors of either the head and neck or the lung. The exception to these considerations is nasopharyngeal carcinoma, which is treated with primary chemoradiation, regardless of the status of the neck. This should be the first step in assessing these patients.
The term operable refers to a reasonable degree of safety and chance of success. The term resectable refers to the ability to completely resect the tumor with adequate or clear surgical margins. Tumors that are inoperable or unresectable may still be treatable or even curable with nonsurgical therapy.
The treatment for the primary tumor dictates the management of neck disease. Therefore, if the primary tumor is treated surgically, then the neck disease will also be treated initially with neck dissection. If chemoradiation is the initial choice of therapy for the primary site, then the neck will also be treated with chemoradiation followed by completion neck dissection. However, if the goal is palliation, multimodality management (surgery, radiation, chemotherapy) is used to alleviate suffering and to minimize morbidity.
Operable primary tumors and N3 neck disease may be managed with surgical resection followed by radiation, with or without chemotherapy, to achieve the best chance of locoregional control.
Based on the head and neck surgeon's realistic and mature surgical judgment, and after the risk, benefits, alternative treatments, and potential complications are weighed, the ultimate decision concerning tumor resectability can sometimes be determined only at the time of surgery. During surgery, the surgeon should bear in mind that the execution of extended neck dissection, in which vital structures have to be sacrificed, has no benefit to the patient if the tumor cannot be completely resected. [8]
The indications for concurrent chemoradiation are as follows:
-
Inoperable and unresectable primary tumor and/or nodal disease
-
Organ preservation
-
Patient refuses surgical treatment
Chemotherapy is typically indicated with adjuvant radiation therapy after surgical treatment for pathologic findings of extracapsular spread and close (within 5 mm) or positive margins. [9]
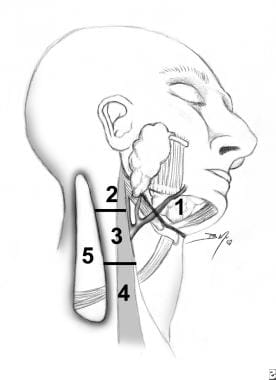
Relevant Anatomy
The cervical lymphatics have been divided into levels based on the patterns of spread of the primary tumor from different sites of the aerodigestive digestive site. [9] . Classification of the neck levels have helped to standardize surgical treatment of the neck as well as serve as a prognostic indicator of outcomes. The neck levels are as follows:
-
Level Ia - Submental triangle
-
Level Ib - Submandibular triangle
-
Level IIa - Jugulodigastric nodes from the skull base to the hyoid bone, anterior to CN IX
-
Level IIb - Jugulodigastric nodes from the skull base to the hyoid bone, posterior to CN IX
-
Level III - Jugulodigastric nodes from the hyoid bone to the cricoid cartilage
-
Level IV - Jugulodigastric nodes from the cricoid cartilage to the clavicle
-
Level Va - Posterior triangle nodes superior to the horizontal plane of the cricoid cartilage
-
Level Vb - Posterior triangle nodes inferior to the horizontal plane of the cricoid cartilage (supraclavicular nodes)
Contraindications
The following are contraindications to surgical management of N3 neck disease:
-
Carotid artery encasement
-
Paraspinous muscle invasion
-
Vertebral column invasion
-
Skull base invasion and/or extension
-
Horner syndrome
-
Phrenic nerve palsy
-
Brachial plexus palsy
-
Uncontrolled primary tumor site
-
Levels of metastasis to cervical lymph nodes.