Practice Essentials
The treatment of patients with N0 squamous cell carcinoma (SCCA) of the head and neck (ie, SCCA of the head and neck in which no cancer has been found in nearby lymph nodes) remains controversial. The negative impact of regional lymph node metastases on the survival in patients with SCCA of the upper aerodigestive tract has been well established. The presence of lymph node metastases is the most important prognostic factor for survival in head and neck SCCA. Histologically proven lymph node metastasis increases the stage to 3 and may decrease survival by 50%.
Watchful waiting until a patient with an N0 neck develops detectable neck disease has been shown to significantly decrease survival. Elective or prophylactic neck dissection improves regional control, and the results of salvage surgery for N0 necks that were observed and that progressed to N+ necks, are poor. Therefore, the challenge of caring for patients with an N0 neck lies in identifying which patients are at risk for developing lymph node metastases in order to treat those patients prophylactically and to decrease the risk of neck failure.
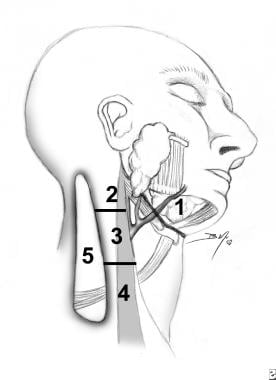
The levels of metastasis to cervical lymph nodes can be seen in the image below.
Signs and symptoms
The following signs and symptoms should increase the index of suspicion for possible malignancy:
-
Nerve deficit
-
Obstruction (nasal, airway, digestive)
-
Persistent sore throat
-
Persistent globus sensation
-
Hoarseness
-
Stridor
-
Leukoplakia
-
Erythroplakia
-
Neck node
-
Masses or nodules in the head and neck region
-
Ulceration
Workup
Chest radiography is standard in the pretreatment evaluation of patients with head and neck cancer.
Regardless of the type of imaging chosen, cervical lymph nodes must be considered to harbor metastasis if the any of the following criteria are met:
-
Node larger than 1 cm (or >1.5 cm in the jugulodigastric area)
-
Round node instead of oval
-
Internal central or peripheral attenuation suggestive of necrosis
-
Poorly defined mass in the lymph node–bearing area
-
The combination of ill-defined borders and loss of plane between mass and normal adjacent neck structures
-
Retropharyngeal node larger than 1 cm
-
Extracapsular extension
Management
Medical therapy
If the likelihood of metastasis is low (< 15%), watchful waiting is appropriate. However, if the primary tumor contains aggressive characteristics such as perineural invasion, deep penetration (more than 3 mm in the oral cavity), or angiolymphatic invasion, prophylactic treatment is necessary. [1]
Radiation has been shown to control regional recurrences in 95% of cases in which the primary site remains free of disease.
Surgical therapy
Selective neck dissection is the mostly commonly used surgical therapy today in treating the N0 neck.
Supraomohyoid neck dissection includes levels 1, 2, and 3 and is used to treat cancer of the oral cavity, some oropharyngeal cancers, and other cancers that drain to this nodal basin.
Lateral neck dissection includes levels 2, 3, and 4 and is used in patients with cancer of the hypopharynx or larynx or other cancers that drain to this nodal basin.
Modified radical neck dissection involves dissection of nodal basins 1-5, with preservation of the internal jugular vein, sternocleidomastoid muscle (SCM), and spinal accessory nerve.
Epidemiology
Frequency
The basic rule for prophylactic treatment of the N0 neck is to treat any patient whose risk of occult lymph node metastases is greater than 15-20%. The risk of regional lymph node metastases varies according to primary site and stage. Areas such as the glottis carry a relatively low risk (< 4% for a T1 lesion), whereas the risk in a site such as the tongue base is as high as 55%. The prevalence of occult neck metastases by site is as follows:
-
Floor of mouth - 25%
-
Oral tongue - 60%
-
Buccal mucosa - 20%
-
Retromolar trigone - 20%
-
Hard palate - 15%
-
Alveolus - 15%
-
Tonsil - 36%
-
Tongue base - 55%
-
Epiglottis - 15%
-
False vocal cord - 15%
-
Aryepiglottic fold - 30%
-
True vocal cord - 15%
-
Pyriform sinus - 65%
Pathophysiology
The following are the lymphatic drainage nodes and the corresponding tumor locations from which they receive drainage:
-
Level 1A nodes
Lip
Anterior mandibular alveolar ridge
Floor of the mouth
-
Level 1B nodes
Oral cavity
Anterior nasal cavity
Soft tissues and structure of the mid face
-
Level 2 nodes
Oral cavity
Nasal cavity
Nasopharynx
Oropharynx
Hypopharynx
Larynx
Parotid gland
-
Level 3 nodes
Oral cavity
Nasopharynx
Oropharynx
Hypopharynx
Larynx
-
Level 4 nodes
Hypopharynx
Larynx
Cervical esophagus
-
Level 5 nodes
Nasopharynx
Oropharynx
-
Level 6 nodes
Thyroid gland
Larynx (glottic and subglottic)
Apex of the pyriform sinus
Cervical esophagus
-
Retropharyngeal nodes
Nasopharynx
Maxilla
Tonsil
Oropharynx
Hypopharynx
Pyriform sinus
Parathyroid cancer
Cervical esophagus
Presentation
Obtain patient's history and perform a complete head and neck physical examination. Although detailing a proper history taking for a head and neck examination is beyond the scope of this chapter, the following signs and symptoms should increase the index of suspicion for possible malignancy:
-
Nerve deficit
-
Obstruction (nasal, airway, digestive)
-
Persistent sore throat
-
Persistent globus sensation
-
Hoarseness
-
Stridor
-
Leukoplakia
-
Erythroplakia
-
Neck node
-
Masses or nodules in the head and neck region
-
Ulceration
Indications
The indication for treating the N0 neck with surgery or radiation is a risk of occult metastases in excess of 15-20%.
Surgery (elective neck dissection) is indicated if the patient is undergoing surgery for the primary lesions. This approach allows accurate staging because it is supported by histologic studies.
A study by Pfisterer et al found that in patients with SCCA of the parotid gland who had an N0 neck, 5-year disease-specific survival was 78.3% for those who underwent elective neck dissection, compared with 51.1% for those who did not. The study used data from the Surveillance, Epidemiology, and End Results (SEER) registry. [2]
In a retrospective study, Philip and James recommended that level 1-3 ipsilateral neck dissection be performed in patients with intraoral maxillary SCCA with an N0 neck. The study, which included 39 patients, found that N0 patients who did not undergo neck dissection had a similar progression rate to disease development as patients with an N+ neck, while ipsilateral neck disease seemed to be resolved in N0 patients who underwent ipsilateral neck dissection. [3]
Radiation in N0 neck cases is indicated in the following situations:
-
Radiation of the primary site is possible.
-
The patient refuses surgery.
-
The patient has significant medical comorbidities such that surgery of this magnitude is contraindicated.
Relevant Anatomy
During physical examination or during neck dissection, anatomical boundaries are used to identify the lymph nodal levels. The radiologic boundaries are used as reference points during the reading of radiologic images and identification lymph node nodal levels.
The anatomical and radiologic nodal boundaries are as follows:
-
Level 1 (submental and submandibular lymph nodes)
Anatomic borders
Level 1A (submental nodes) boundaries include the anterior belly of digastric and hyoid bone.
Level 1B (submandibular nodes) boundaries include the anterior belly and posterior belly, body of the mandible, and the lymph nodes in the facial vessels.
Radiologic borders: Nodes are above the hyoid bone, superficial to the mylohyoid and anterior to the transverse line drawn through the posterior edge of the submandibular gland.
-
Level 2 (superior jugular nodes)
Anatomic borders
Lymph nodes are anterior to and behind the great vessels, extending from the skull base to the carotid bifurcation and between the sternohyoid muscle anteriorly and the posterior border of the sternocleidomastoid muscle posteriorly. Level 2 is further divided into A or B using CN 11 as an anatomical reference point.
Level 2A (nodes anterior to the spinal accessory nerves [CN 11])
Level 2B (nodes posterior to the spinal accessory nerve)
Radiologic borders: Lymph nodes are along the superior aspect of the jugular vein, extending from the skull base to the inferior aspect of the hyoid bone and between the back of the submandibular gland anteriorly and the posterior border of the sternocleidomastoid muscle posteriorly.
-
Level 3 (midjugular nodes)
Anatomic borders: Lymph nodes are along the middle third of the jugular vein. They are bounded superiorly by the carotid bifurcation, inferiorly by the omohyoid muscle, anteriorly by the sternohyoid muscle, and posteriorly by the border of the sternocleidomastoid muscle.
Radiologic borders: Lymph nodes are along the middle third of the jugular vein, extending from the bottom of the cricoid arch and between the sternohyoid muscle anteriorly and the posterior border of the sternocleidomastoid muscle posteriorly.
-
Level 4 (inferior jugular lymph nodes)
Anatomic borders: Lymph nodes are along the inferior aspect of the jugular vein and are bounded superiorly by the omohyoid muscle, inferiorly by the clavicle, anteriorly by the sternohyoid muscle, and posteriorly by the posterior border of the sternocleidomastoid muscle.
Radiologic borders: Lymph nodes are along the inferior aspect of the jugular vein, extending from the inferior aspect of the cricoid arch to the clavicle, and lying anterior to line connecting the posterior border of the sternocleidomastoid muscle and the posterolateral border of the anterior scalene muscle.
-
Level 5 (posterior triangle lymph nodes)
Anatomic borders
The posterior triangle lymph nodes are bounded anteriorly by the sternocleidomastoid muscle, posteriorly by the trapezius muscle, and inferiorly by the clavicle.
Level 5A: Nodes are superior to the level of the cricoid cartilage.
Level 5B: Nodes are inferior to the level of the cricoid cartilage.
Radiologic borders: Lymph nodes are bounded posteriorly by the trapezius muscle, inferiorly by the clavicle, anteriorly by the posterior border of the sternocleidomastoid muscle above the inferior border of the cricoid arch, and by the line connecting the posterior border of the sternocleidomastoid muscle and the posterolateral border of the anterior scalene muscle below the cricoid arch.
-
Level 6 (central compartment lymph nodes)
Anatomic borders: The lymph nodes are bounded superiorly by the hyoid bone, laterally by the carotid arteries, and inferiorly by the suprasternal notch.
Radiologic borders: Lymph nodes are bounded by the carotid sheath laterally, hyoid bone superiorly, and manubrium inferiorly.
-
Retropharyngeal nodes of Rouviere
Anatomic borders: The lymph nodes are posterior to the nasopharynx and oropharynx and medial to the carotid arteries.
Radiologic borders: Lymph nodes are from the skull base to T4 vertebrae.
-
Levels of metastasis to cervical lymph nodes.