Overview
Cancers in the head and neck region commonly metastasize to cervical lymph nodes. The term "neck dissection" refers to a surgical procedure in which the fibrofatty contents of the neck are removed for the treatment of cervical lymphatic metastases. Neck dissection is most commonly used in the management of cancers of the upper aerodigestive tract. It is also used for malignancies of the skin of the head and neck area, the thyroid, and the salivary glands as depicted in the images below. [1]
 Selective neck dissection for thyroid cancer: selective neck dissection VI, or anterior neck dissection.
Selective neck dissection for thyroid cancer: selective neck dissection VI, or anterior neck dissection.
 Selective neck dissection for posterior scalp and upper posterolateral neck cutaneous malignancies: selective neck dissection II-V, postauricular, suboccipital, or posterolateral neck dissection.
Selective neck dissection for posterior scalp and upper posterolateral neck cutaneous malignancies: selective neck dissection II-V, postauricular, suboccipital, or posterolateral neck dissection.
Radical neck dissection was the original surgical procedure described for treatment of metastatic neck cancer. Crile described the operation in 1906, and until recently, radical neck dissection was considered the standard procedure for management of both occult and clinically positive neck disease. In the last 2 decades, a shift toward the use of more conservative surgical procedures has occurred. This shift is predicated upon the following 2 important insights that developed over a period of time: 1) the removal of lymphatic tissue is not hindered by preserving adjacent nonlymphatic structures; and 2) the specific nodal groups at risk for metastatic disease are predictable on the basis of the size, location, and other features of the primary tumor
Neck dissection with conservation of nonlymphatic structures was shown by Bocca, Gavilan, and others to yield equivalent oncologic outcomes, with improved functional results. [2, 3] Experimental studies of lymphatic drainage, coupled with clinical studies of the specific location of nodal metastasis within neck dissection specimens, provided the rationale for more targeted surgery. [4, 5, 6] The data allowed for reliable prediction of the lymph node groups most likely to be involved with metastatic disease from specific primary tumor location and established which lymph node groups carry negligible risk of involvement and may be safely preserved. As a result, a great variety of surgical procedures have been described for use in various clinical situations.
In order to bring uniformity to the terminology used to describe these operations, the American Academy of Otolaryngology-Head and Neck Surgery (AAO-HNS) sponsored the Committee for Head and Neck Surgery and Oncology to develop a classification system for neck dissections. In 1991, the committee published the first classification schema. This schema, later modified in 2002 and 2008, has become universally accepted and is currently endorsed by both the AAO-HNS and the American Head and Neck Society. [7, 8, 9, 10, 11]
A retrospective study by van Lanschot et al indicated that in patients with early stage oral cavity squamous cell carcinoma, 5-year regional recurrence–free survival (RRFS) rates are lower in patients with depth of invasion of 4 mm or more who are not treated with elective neck dissection. Those treated with elective neck dissection had an RRFS rate of 89.0%, compared with 69.9% for those who did not undergo dissection. [12] These findings correlate well with results from a randomized, controlled trial by D’Cruz et al. In this, the disease-free and absolute overall survival benefits were 23.6 and 12.5 percentage points, respectively, in patients with T1 or T2 invasive squamous cell carcinoma of the tongue, floor of the mouth, or buccal mucosa (lateralized to one side of the midline) who underwent elective neck dissection at the time of primary surgery. [13]
Relevant Anatomy
The lymphatic drainage of the mucosal surfaces and other tissues of the head and neck is directed to the lymph nodes located within the fibroadipose tissue that lies between the investing (superficial) layer of the deep fascia superficially and the visceral and prevertebral layers underneath. In this space, these lymph nodes tend to be aggregated around certain neural and vascular structures such as the internal jugular vein, spinal accessory nerve, and transverse cervical artery. [14]
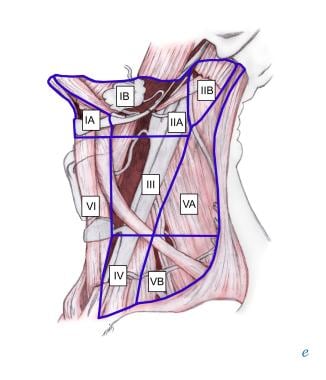
In his 1964 study of lymphatic drainage of this area, Fisch, using the technique of lymphography, was able to improve upon the anatomic classification proposed by Rouviere. [6] Fisch classified these lymph nodes into the following 5 categories: junctional, jugular, spinal, supraclavicular, and retroauricular. However, the nomenclature in popular use today comes from the Memorial Sloan Kettering Cancer Center. This classification was used to describe the patterns of metastatic dissemination observed in more than 1000 patients who were treated at the center with radical neck dissection. Lymph nodes in the neck are grouped into levels I-V, corresponding with the submandibular and submental nodes (level I); upper, middle, and lower jugular nodes (levels II, III, IV); and posterior triangle nodes (level V). Refer to the following image.
Level I
This level has been defined as being bound by the body of the mandible superiorly, the stylohyoid muscle posteriorly, and the anterior belly of the digastric muscle on the contralateral side anteriorly. However, the 2008 classification revision proposed that, as an alternative to the stylohyoid muscle, the vertical plane marked by the posterior edge of the submandibular gland be used as a boundary between levels I and II. [11]
Level I may be divided into level Ia, which refers to the nodes in the submental triangle (bound by the anterior bellies of the digastric muscles and the hyoid bone), and Ib, which refers to the submandibular triangle nodes (see image below). The nodes of level Ia are at greatest risk of harboring metastasis from cancers that arise from the floor of mouth, anterior tongue, anterior mandibular alveolar ridge, and lower lip, while the nodes of level Ib often receive metastasis from cancers of the oral cavity, anterior nasal cavity, soft tissue structures of the midface, and submandibular gland.
Closely related, although not strictly a part of the level I group of nodes, are the perifacial nodes, related to the facial vessels above the mandibular margin, and the buccinator nodes, which may become involved with metastasis from tumors in the buccal mucosa, nose, and soft tissues of the cheek and lips.
Level II
Level II lymph nodes are related to the upper third of the jugular vein, extending from the skull base to the inferior border of the hyoid bone. The posterior border of level II is the posterior border of the sternocleidomastoid muscle, while the anterior border of level II has been defined as the stylohyoid muscle. As mentioned above, however, the 2008 classification revision proposed that the vertical plane marked by the posterior edge of the submandibular gland be used as an alternative to the stylohyoid muscle boundary. [11]
The spinal accessory nerve, which travels obliquely across this area, is used as a landmark to subdivide this group into IIb, the portion above and behind the nerve, and IIa, the part that lies anteroinferiorly and closer to the internal jugular vein as depicted below. The nodes in level II are at greatest risk of harboring metastasis from cancers that arise from the oral cavity, nasal cavity, nasopharynx, oropharynx, hypopharynx, larynx, and parotid gland.
Level III
Level III nodes are located between the hyoid superiorly and a horizontal plane defined by the inferior border of the cricoid cartilage. The sternohyoid muscle marks the anterior limit of level III, and the posterior border of the sternocleidomastoid muscle is the posterior border. Level III most commonly receives metastasis from cancers that originate in the oral cavity, nasopharynx, oropharynx, hypopharynx, and larynx. See the image shown below.
Level IV
This refers to the group of nodes related to the lower third of the jugular vein. These nodes are located between the inferior border of the cricoid cartilage and the clavicle, and, like level III, the anterior boundary is the sternohyoid muscle, and the posterior border is the posterior border of the sternocleidomastoid muscle. The nodes of level IV commonly harbor metastasis from cancer that originates in the larynx, hypopharynx, thyroid, [15] and cervical esophagus as shown below.
A literature review by Weisz Shabtay and Ronen reported that in patients with clinically negative neck (cN0) oral tongue squamous cell carcinoma, level IV involvement was found in just 16 out of 498 patients, with the incidence of skip metastases, that is, metastases that bypassed levels I-III and spread directly to level IV, also being low. Therefore, the investigators recommended that patients with cN0 oral tongue squamous cell carcinoma undergo elective neck dissection of levels I-III. [16]
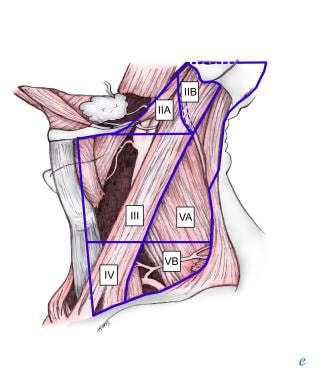
Level V
This refers to the lymph nodes located in the posterior triangle of the neck. These include the spinal accessory, transverse cervical, and supraclavicular group of nodes. Level V is bound anteriorly by the posterior border of the sternocleidomastoid muscle and posteriorly by the anterior border of the trapezius muscle. Level V extends from the apex of the convergence of the sternocleidomastoid and trapezius muscle superiorly to the clavicle inferiorly as shown below. This level is subdivided by a plane defined by the inferior border of the cricoid cartilage into level Va superiorly and level Vb inferiorly.
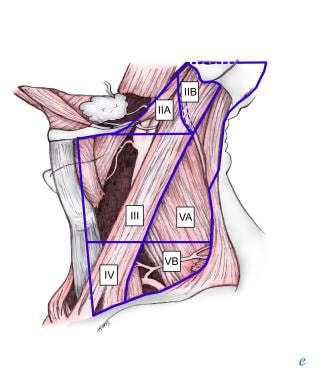 Selective neck dissection for posterior scalp and upper posterolateral neck cutaneous malignancies: selective neck dissection II-V, postauricular, suboccipital, or posterolateral neck dissection.
Selective neck dissection for posterior scalp and upper posterolateral neck cutaneous malignancies: selective neck dissection II-V, postauricular, suboccipital, or posterolateral neck dissection.
Level Va contains the nodes associated with the spinal accessory nerve, and level Vb contains the transverse cervical and supraclavicular nodes. The posterior triangle nodes are at greatest risk for harboring metastasis from cancers that arise in the nasopharynx, oropharynx, and skin of the posterior scalp and neck.
Level VI
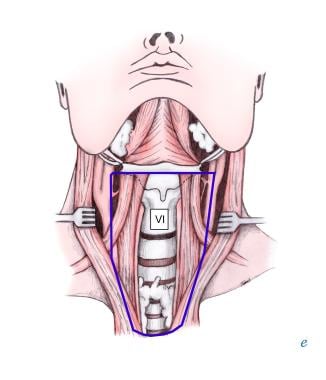
This refers to lymph nodes of the anterior, or central, compartment of the neck. Defined by the carotid arteries laterally, the hyoid bone superiorly, and the suprasternal notch inferiorly, it is rich in lymphatics that drain the thyroid gland, subglottic larynx, cervical trachea, hypopharynx, and cervical esophagus. Lymph nodes in this compartment are located in the tracheoesophageal groove (paratracheal nodes), in front of the trachea (pretracheal nodes), around the thyroid gland (parathyroidal nodes), and on the cricothyroid membrane (precricoid or Delphian node). Lymph nodes in the central compartment are not routinely excised in radical neck dissection; most commonly, they are removed during surgery for thyroid, laryngeal, and hypopharyngeal cancer. See image shown below.
Classification of Neck Dissections
Principles of Classification
The current classification of neck dissections developed by the Committee for Head and Neck Surgery and Oncology of the American Academy of Otolaryngology-Head and Neck Surgery is based on the following governing principles:
-
Radical neck dissection is the standard basic procedure for cervical lymphadenectomy, and all other procedures represent one or more modifications to this procedure.
-
When modification of the radical neck dissection involves preservation of one or more nonlymphatic structures, the procedure is termed a modified radical neck dissection (see the Medscape Reference article Modified Radical Neck Dissection).
-
When the modification involves one or more lymph node groups that are routinely removed in the radical neck dissection, the procedure is termed a selective neck dissection.
-
When the modification involves removal of additional lymph node groups or nonlymphatic structures relative to the radical neck dissection, the procedure is termed an extended radical neck dissection.
Radical Neck Dissection
Originally described by Crile in 1906, this procedure is an en bloc clearance of all fibrofatty tissue from one side of the neck, including the lymph nodes from levels I-V and lymph nodes that surround the tail of the parotid gland, the spinal accessory nerve, the internal jugular vein, and the sternocleidomastoid muscle. Radical neck dissection does not include the removal of the postauricular, suboccipital, perifacial, buccinator, retropharyngeal, or central compartment nodes. Previously used for neck disease of any stage, from microscopic to bulky nodal disease, this procedure is now limited to patients with advanced neck disease, recurrent disease after chemoradiation, or gross extracapsular spread to the spinal accessory nerve, sternomastoid muscle, and the internal jugular vein.
Modified Radical Neck Dissection
This operation involves the removal of the same lymph node groups as those involved in the radical neck dissection (levels I-V) but requires preservation of 1 or more of the following 3 nonlymphatic structures: the spinal accessory nerve, the internal jugular vein, and the sternomastoid muscle. The structure or structures preserved should be specifically indicated in the name of the procedure (eg, modified radical neck dissection with preservation of accessory nerve and internal jugular vein). [17]
Modified neck dissection is indicated for clinically palpable metastatic neck disease. Conversion to the radical neck dissection becomes necessary upon gross involvement of the nerve, vein, and muscle, although the involvement of all 3 is unusual, except in very advanced (N3) disease. Comprehensive neck dissection is a term that frequently appears in the literature. This term refers to any type of neck dissection that involves removal of lymph nodes from levels I-V and corresponds, therefore, to radical neck dissections and modified radical neck dissections, according to the Academy's classification.
Selective Neck Dissection
This term refers to a type of neck dissection in which one or more lymph node groups normally removed in a radical neck dissection are preserved. The 1991 classification schema classified selective neck dissections into the following categories: supraomohyoid neck dissection (levels I, II, III), lateral neck dissection (levels II, III, IV), anterior compartment neck dissection (VI), and posterolateral neck dissection (levels II, III, IV, V). Because of the increased use of selective neck dissection and the increased selectivity with which lymph node groups are removed, the Committee for Head and Neck Surgery and Oncology revised the classification of selective neck dissections in 2002.
Because the 1991 classification did not provide an accurate description of procedures in which the surgeon preserves certain sublevels, the 2002 classification excludes the above listed "named" selective neck dissections. In the 2002 classification, selective neck dissections are described with respect to the lymph node levels removed. For example, a supraomohyoid neck dissection is described as a selective neck dissection (I-III).
A retrospective study by Barzan et al indicated that selective neck dissection can be safely and effectively performed as primary and salvage surgery. The report involved 827 patients with primary head and neck tumors who underwent the selective operation, with just 22 of 40 neck cancer recurrences later arising on the dissected side of the neck. The incidence of recurrence was approximately the same after primary and salvage surgery (4.4% and 5.2%, respectively). [18]
United Kingdom (UK) National Multidisciplinary Guidelines from 2016 on the management of neck metastases in head and neck cancer included the following recommendations with regard to selective neck dissection [19] :
-
Selective neck dissection is as effective as modified radical neck dissection for controlling regional disease in N0 necks for all primary sites
-
Selective neck dissection alone is adequate treatment for pN1 neck disease without adverse histologic features
UK National Multidisciplinary Guidelines from 2016 regarding recurrent head and neck cancer included the following recommendations [20] :
-
Consider elective selective neck dissections in patients with recurrent primaries with N0 necks, especially in advanced cases
-
Selective neck dissection (with preservation of nodal levels, especially level V, that are not involved by disease) in patients with nodal (N+) recurrence appears to be as effective as modified or radical neck dissections
UK National Multidisciplinary Guidelines from 2016 for the management of thyroid cancer included the recommendation that patients with medullary thyroid cancer with lateral nodal involvement undergo selective neck dissection (IIa–Vb). [21]
UK National Multidisciplinary Guidelines from 2016 for the management of lateral skull base cancer included the recommendation that for patients undergoing surgery for squamous cell carcinoma, at least a superficial parotidectomy and selective neck dissection be carried out. [22]
Selective neck dissection for oral cavity cancer
Selective removal of the level I, II, and III lymph nodes is the surgical procedure of choice for management of N0 and N1 disease that originates from cancers of the oral cavity, as shown below. [23] However, because of the lymphatic drainage of the oral tongue, some authorities advocate selective neck dissection (I-IV) for cancers that originate from this subsite. The operation includes the resection of soft tissue in the submental triangle, along with the submandibular triangle contents, including the submandibular gland and the fibrofatty tissue along the internal jugular vein from the skull base to the omohyoid muscle (or clavicle). The dissected contents include the fascia that covers the medial aspect of the sternomastoid muscle; the muscle itself is laterally retracted and preserved. These neck contents are peeled off from the internal jugular vein and from around the accessory nerve, sparing these structures (see the image below).
Selective neck dissection for oropharyngeal, hypopharyngeal, and laryngeal cancer
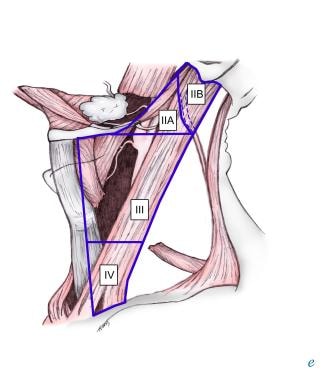
Selective neck dissection (II-IV) is the surgical procedure of choice in the elective treatment of neck disease in patients with cancers that originate in the oropharynx, hypopharynx, or larynx (refer to image below). [24]
The spinal accessory nerve, sternomastoid muscle, and internal jugular vein are spared in this operation, while the lymph nodes are removed from the skull base superiorly to the clavicle inferiorly, and from the cutaneous branches of the cervical plexus at the posterior border of the sternocleidomastoid muscle posteriorly to the sternothyroid muscle anteriorly. If the jugular chain nodes above the spinal accessory nerve were preserved, the procedure would be named selective neck dissection (IIa, III, IV).
Selective neck dissection for cancer of the midline structures of the anterior lower neck
This operation involves excision of the level VI lymph nodes (selective neck dissection [VI]). The procedure is indicated for the treatment of cancers of the thyroid gland (see image below), hypopharynx, cervical trachea, cervical esophagus, and subglottic larynx.
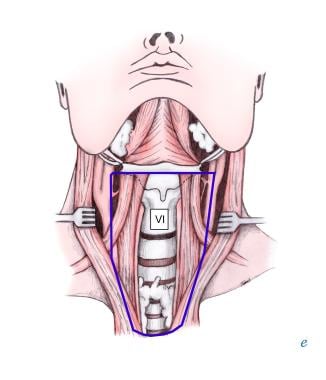 Selective neck dissection for thyroid cancer: selective neck dissection VI, or anterior neck dissection.
Selective neck dissection for thyroid cancer: selective neck dissection VI, or anterior neck dissection.
The boundaries of the dissection are the hyoid bone superiorly, the suprasternal notch inferiorly, and the carotid sheaths on both sides. Hypoparathyroidism may be a disabling complication if care is not taken to identify and preserve the parathyroid glands, and injury to the parathyroid blood supply is a risk with this procedure. Excising and reimplanting the glands into the sternomastoid or pectoralis major muscle or the anterior forearm muscles may be necessary. Alternatively, the dissection may be limited to one side if the lesion is not close to the midline, particularly if radiation therapy can be administered postoperatively.
A study by Song et al in which robotic selective neck dissection with total thyroidectomy was compared with conventional transcervical selective neck dissection with total thyroidectomy found that patients with papillary thyroid carcinoma who underwent the robotic surgery had higher postoperative cosmetic satisfaction. However, it was also found that length of surgery and degree of anterior chest pain were greater with the robotic technique. [25]
Selective neck dissection for cutaneous malignancies
Selective neck dissection (II-V, postauricular, suboccipital) was initially described as a posterolateral neck dissection by Rochlin in 1962 and later modified and popularized by Geopfert et al for use in patients with cutaneous malignancies of the scalp and postauricular and suboccipital regions as depicted below. Unlike all other neck dissections, this operation is performed with the patient in the lateral decubitus position and consists of an en bloc removal of the lymph nodes in the suboccipital; postauricular; and upper, middle, and lower jugular nodes, along with posterior triangle nodes situated superior to the accessory nerve. See the image below.
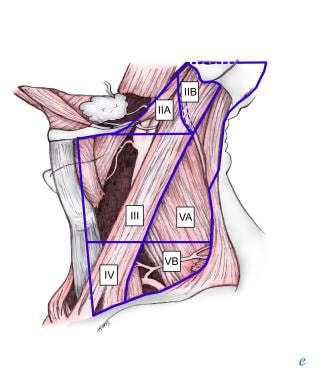 Selective neck dissection for posterior scalp and upper posterolateral neck cutaneous malignancies: selective neck dissection II-V, postauricular, suboccipital, or posterolateral neck dissection.
Selective neck dissection for posterior scalp and upper posterolateral neck cutaneous malignancies: selective neck dissection II-V, postauricular, suboccipital, or posterolateral neck dissection.
Although the original description included sacrifice of the accessory nerve, internal jugular vein, and a portion of the trapezius muscle, Diaz et al from the MD Anderson Cancer Center showed in 1996 that the preservation of these nonlymphatic structures does not increase the failure rate of this operation. [26] Any variation of this operation involves naming the level of nodes removed. In cancers that arise in the preauricular, anterior scalp, or temporal region, the elective neck dissection of choice is selective neck dissection (II, III, Va, parotid, facial, external jugular nodes).
Extended Neck Dissection
In cases of advanced neck disease, certain lymphatic or nonlymphatic structures not routinely included in the aforementioned neck dissections may have to be removed. Extended neck dissection is the term used to describe these procedures. Retropharyngeal lymph nodes, the hypoglossal nerve, portions of the prevertebral musculature, or the carotid artery are some of the structures that may occasionally have to be excised to obtain negative margins. All additional lymphatic and nonlymphatic structures removed should be identified in parentheses.
In a study of extended neck dissection in 72 patients with human papillomavirus (HPV)–related oropharyngeal squamous cell carcinoma (SCC), Zenga et al reported that advanced T classification, a pathologic node number of five or more, and no employment of adjuvant radiotherapy were associated with a reduced disease-free survival rate. [27]
Questions & Answers
Overview
What is the anatomy of the neck relative to neck dissection?
What is the anatomy of the level II group of lymph nodes in neck dissection?
What is the anatomy of the level III group of lymph nodes in neck dissection?
What is the anatomy of the level I group of lymph nodes in neck dissection?
What is the anatomy of the level IV group of lymph nodes in neck dissection?
What is the anatomy of the level V group of lymph nodes in neck dissection?
What is the anatomy of the level VI group of lymph nodes in neck dissection?
What are principles of neck dissection classification?
How is radical neck dissection defined?
How is modified radical neck dissection defined?
How is selective neck dissection defined?
What is the role of neck dissection in the treatment of oral cavity cancer?
What is the role of neck dissection in the treatment of cutaneous malignancies?
-
Selective neck dissection levels I-III.
-
Selective neck dissection levels II-IV.
-
Selective neck dissection for thyroid cancer: selective neck dissection VI, or anterior neck dissection.
-
Selective neck dissection for posterior scalp and upper posterolateral neck cutaneous malignancies: selective neck dissection II-V, postauricular, suboccipital, or posterolateral neck dissection.
-
The 6 levels of the neck with sublevels.