Sleep-Disordered Breathing
Sleep-disordered breathing (SDB) is characterized by repetitive upper airway obstruction and consequent oxyhemoglobin desaturation during the deeper stages of sleep. [1] The proposed etiology is a combination of both abnormal upper airway anatomy and a yet-to-be determined aberrant afferent/efferent somatosensory loop.
The health-related consequences of SDB are well documented by large prospective cohort studies and chiefly include hypertension, myocardial infarction, stroke, diabetes, depression, excessive daytime fatigue, and a greater risk of motor vehicle accidents. These associated medical problems place an enormous financial burden on society. Because of the high prevalence of this condition, cost-effective management is essential.
Fortunately, a number of viable management options are available. The most common initial treatment for SDB is a continuous positive airway pressure (CPAP) device. [2, 3] However, CPAP devices can prove annoying and discomforting to many patients, and, for some patients, may be entirely intolerable.
Thus, CPAP is effective only for patients who can tolerate the device and, unfortunately, affords no permanent cure.
Surgical intervention is an alternative form of treatment and involves anatomic reconstruction of the airway. [4] Although more expensive from the outset, it has long-lasting effects, because surgical intervention results in a permanent alteration of the airway. However, the prospect of surgery may not appeal to all patients. As a result, prosthetic devices are available as effective and low-cost treatment options for those patients that cannot tolerate CPAP and do not wish to undergo surgery. [5, 6]
See also Sleep-Disordered Breathing and CPAP and Surgical Approach to Snoring and Sleep Apnea.
Relevant anatomy, etiology, and pathophysiology
Although primary hypoventilation may be an underlying cause of SDB, the most important factor is the anatomy of the upper airway. In general, obstruction of the airway may be found at three primary sites (ie, nose, velopharynx, hypopharynx). During normal awake respiration, the obstructive tendency of the negative inspiratory pressure within the upper airway is balanced by the outward force of pharyngeal dilator muscle activity under central nervous system (CNS) control. Reduction of tone in this musculature and loss of compensatory reflex dilator mechanisms during deep sleep result in the airway obstruction. [7, 8, 9]
Snoring, a common symptom of SDB, is a repetitive sound caused by vibration of upper airway structures during sleep. Snoring is a good indicator of increased upper airway resistance.
Patients who have obstructive sleep apnea (OSA) generally have smaller upper airways than normal individuals. Increased parapharyngeal fat, a large tongue, an elongated palate, thickened lateral pharyngeal walls, as well as maxillofacial skeletal deficiencies may all play a role in OSA. Lateral pharyngeal wall encroachment by the peritonsillar pillars and tonsillar tissue is also an important etiology of OSA. This tissue bulk may direct the airway anteroposteriorly, as opposed to the normal lateral orientation, forcing the pharyngeal muscles to act at a disadvantage. Greater pharyngeal length increases collapsibility, which may explain why men are more susceptible to OSA than women.
See also Upper Airway Evaluation in Snoring and Obstructive Sleep Apnea and Physiologic Approach in Snoring and Obstructive Sleep Apnea.
SDB evaluation
The symptom and physical findings in patients with SDB, as well as tests used to diagnose this disorder, are briefly discussed below.
Symptoms
Patients with SDB generally present with symptoms of loud snoring or with struggling efforts to breathe, often reported by their sleep partner; choking episodes during sleep; awakening with early morning headaches [10] ; chronic fatigue, feeling of drowsiness, or needing frequent napping during the day; depressed mood; falls or automobile accidents, in serious cases; bedwetting in children; and/or nocturia (rare). [11]
Physical findings
Affected patients typically exhibit increases in body mass index (BMI) (about 75% of patients), blood pressure, and neck circumference and waist-hip ratio.
The upper airway should be examined to evaluate for a low hanging, bulky soft palate; large tonsils; large tongue; dental malocclusion; low hyoid position; or maxillomandibular deficiency.
Diagnostic tests/studies
The Epworth Sleepiness Scale (ESS) is a questionnaire used to screen for sleep apnea that relies on the patient's description of symptoms.
Polysomnography (testing in a sleep laboratory) is the gold standard test used to establish the diagnosis of SDB.
The multiple sleep latency test (MSLT) is used to establish how rapidly the patient falls asleep, to distinguish from narcolepsy.
Lateral cephalometric radiographs reveal the dimensions of the airway column, the position of the hyoid bone, and the craniofacial skeleton for any maxillomandibular deficiencies.
Flexible fiberoptic nasopharyngoscopy examines in real-time the three-dimensional (3-D) structure of the airway revealing any anatomic sites of obstruction.
See also Obstructive Sleep Apnea, Childhood Sleep Apnea, and Obstructive Sleep Apnea and Home Sleep Monitoring.
Sleep positioning and nasal airway obstruction
The patient’s position during sleep can affect simple snoring in patients with significant SDB. In patients whose snoring is primarily due to nasal airway obstruction, surgical or prosthetic intervention may be of benefit.
Nonsupine position
Positioning of the patient during sleep is a useful method to control simple snoring. In mild cases, snoring is often resolved when the patient assumes a nonsupine position, which may relieve the obstruction. The physiology is intuitively simple: the soft palate and tongue fall posteriorly due to gravity and relaxation of the genioglossus. When the mouth opens, the tongue is even more retrodisplaced. Airway obstruction may result in oxyhemoglobin desaturation if apnea occurs. The effect of positioning is demonstrated by polysomnography, which often shows more frequent and severe disordered breathing events when the patient is supine.
The classic remedy of attaching a tennis ball to the back of the individual's pajamas may help some patients with mild cases. However, most patients with significant SDB show apnea in all positions. Thus, this technique is seldom useful for patients with more than simple snoring.
A snoring pillow may help some patients with snoring problems. Used appropriately, the pillow positions the head so that the mouth is closed and the jaw is held forward. Unfortunately, movement during sleep minimizes the pillow's effectiveness.
Nasal airway obstruction
In the normal airway, the limen nasi is the site of the highest resistance to airflow. Collapsed alae, a severely deviated septum, or hypertrophied turbinates may affect airflow substantially. Nasal valve surgery has been demonstrated to improve snoring for many patients whose primary problem is nasal airway obstruction.
Although surgical therapy is effective for treating nasal valve obstruction, devices that splay the alae (externally or internally) have also demonstrated success in improving nasal airflow and decreasing snoring. [12, 13] However, studies disagree on whether significant improvement occurs. Although anecdotal reports describe patients whose sleep apnea may have been controlled by alar splaying devices, no statistical difference in patients using the devices compared with controls has been demonstrated. These devices are benign, inexpensive, and available at any pharmacy. For patients with minimal problems and noticeable nasal airway obstruction, devices that splay the alae are easy to obtain for an at-home trial.
Nasal trumpets may be useful for short-term management in select patients. Trumpets are commonly used in postanesthesia airway management. These devices bypass any nasal, soft-palate, and, often, tongue-base obstructions. However, few patients are willing to use the trumpets nightly to control SDB.
Products
There are numerous patented oral appliances that treat sleep-disordered breathing (SDB) problems, such as snoring and obstructive sleep apnea (OSA). These devices and appliances address a range of processes that result in SDB. This article discusses the general principles involved in controlling SDB and the most effective prosthetic devices for alleviating the condition.
See also Sleep-Disordered Breathing and CPAP and Surgical Approach to Snoring and Sleep Apnea.
Category
Oral appliances
Device details
Fixed devices
-
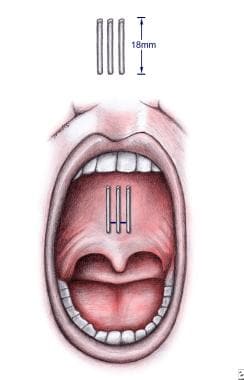
Pillar palatal implants (see the image below)
Adjustable devices
-
Thornton anterior positioner (TAP)
-
Dynamax mandibular device
Design Features
Patients with significant sleep-disordered breathing (SDB) almost always have some component of soft-palate or tongue-base obstruction (typically both). To date, more than 40 different oral appliances have been patented to treat snoring and obstructive sleep apnea (OSA). These devices can be divided into two basic categories, fixed devices and adjustable devices. Each group can be subdivided into noncustom devices (ie, mass produced/one-size-fits-all) and custom devices (ie, fabricated from specific patient impressions). Although most appliances appear similar superficially, because they share the same physiologic principles, they are actually quite different due to basic design features.
See also Obstructive Sleep Apnea; Childhood Sleep Apnea; Surgical Approach to Snoring and Sleep Apnea; Obstructive Sleep Apnea and Home Sleep Monitoring; Upper Airway Evaluation in Snoring and Obstructive Sleep Apnea; Sleep-Disordered Breathing and CPAP; and Physiologic Approach in Snoring and Obstructive Sleep Apnea.
Advantages of oral appliances
Compared with other treatment modalities, oral appliance therapy has several advantages, including simplicity, reversibility, cost-effectiveness, and broad applicability for varying degrees of SDB. An oral appliance can be used to treat simple snoring, upper airway resistance syndrome (UARS), and OSA. In addition, this type of therapy can also be used in conjunction with other forms of treatment.
The advantages of oral appliances include relatively low cost, good success rates (their efficacy is comparable to uvulopalatopharyngoplasty [UPPP]), increased rates of compliance (range, 50-100%), being preferred more than CPAP, [14, 15, 16, 17, 18] a benign adverse-effect profile, rapid effectiveness, and easy termination without sequelae. Additionally, insertion of oral appliances can be performed as a single-stage procedure in an outpatient setting. Oral appliances are recommended for mild to moderate OSA and in patients with body mass indexes (BMIs) of 30 kg/m2 or less in whom CPAP treatment fails or cannot be tolerated. These advantages make oral devices an attractive form of treatment for SDB. Unfortunately, these oral appliances and devices are typically less effective than CPAP. [19]
A literature review by AlRumaih et al indicated that in patients with OSA, oral-appliance use can enhance many patients’ quality of life. The study also reported that owing to their convenience, patients tend to prefer oral appliances over other OSA treatments, including CPAP therapy. [20]
Features that affect prosthetic success
Three primary features determine whether therapy with oral appliances will be successful in patients with SDB: retention, adjustability, and adaptability. Other factors that influence a positive outcome with these devices include younger patient age, lower BMI, smaller neck size, positional OSA-hypopnea syndrome (OSAHS), and a lower apnea-hypopnea index (AHI).
Retention
Oral appliances must fit accurately, comfortably, and remain in position all night. Some devices are made of hard acrylics that wedge against the height of contour of each tooth. Rigid oral appliances periodically require realigning, which is a labor-intensive process. If the patient neglects realigning and continues to wear the device, movement and misalignment of teeth can occur.
Some appliances use orthodontic retentive mechanisms (ie, ball clasps, Adams clasps) that use undercuts on a select number of teeth. Because only a few areas, usually interproximal, are involved (typically four in each arch), movement of teeth frequently occurs.
Heat-sensitive elastomeric materials have also been used. These materials have proven to be the most effective in retention of oral appliances. They allow contact with more dental surface area, including undercuts and portions of interproximal areas, resulting in a more uniform fit and higher rates of appliance retention.
Most noncustom oral appliances are made of soft boil-and-bite elastometrics that usually fail to maintain adequate retention for long when expected to attach to both maxillary and mandibular dentition.
Although Pillar palatal implants are a relatively newer modality, short-term studies have shown good retention. One long term study demonstrated a 17.8% partial extrusion rate.
Adjustability
Oral appliances should be able to variably adjust mandibular position. Many methods are available, such as interchangeable shims, incremental slots, and rotational mechanisms. Both shim and slot methods can be limiting due to the distance required of the mandible (seldom < 1 mm and often 2 mm), which may initiate muscular and/or joint sensitivity. Increments this large may jeopardize the clinicians' ability to optimize treatment.
Increased efficacy can be achieved with a rotational mechanism that allows for more precise positioning of the mandible. Pillar palatal implants are not adjustable, and once inserted remain in place.
Adaptability
Oral appliances must be adaptable to dentition changes (ie, fillings, crowns). Pillar palatal implants are placed into the soft palate, near the junction of the hard palate (see the following image). Consequently, they are adaptable to all patients without palate clefts or fistulas.
Conditions and situations that affect long-term oral appliance success
As a patient’s weight increases, SDB symptoms usually intensify. With weight loss, SDB symptoms typically diminish. With age, muscles in the pharyngeal area atrophy, thus increasing obstruction. Congestion and sinus drainage contribute to nasal and pharyngeal inflammation, constricting the airway and aggravating SDB. Central nervous system (CNS) depressants and muscle relaxants may have a counterproductive sedative or relaxant effect.
Proper sleep hygiene is desirable, with 8 hours total sleep time considered optimal. Maintenance of a consistent sleep schedule also mitigates problems. Obstruction is more prevalent in a supine position. Environmental factors (eg, temperature, lighting, noise, comfort) affect quality and length of sleep.
Soft-palate, tongue, mandibular devices
Oral appliances can advance the soft palate, tongue, or mandible, thus opening the airway. However, devices that advance the soft palate are seldom employed, most likely because of stimulation of the gag reflex and discomfort. Devices that advance the tongue alone are also rarely used, probably for similar reasons and because of the success of adjustable oral appliances.
During obstructive apneas, the collapsed pharynx prevents airflow, which leads to continued negative pressure generated by respiratory efforts. The cycle continues, until the patient is aroused. Traditional devices work by downwardly rotating, and in some cases advancing, the mandible. By altering the position of upper airway structures, these devices serve to enlarge the airway and/or reduce collapsibility. Oral appliances that fixate and/or alter the relative position of the mandible to the maxilla affect the pharyngeal soft tissues by increasing the airway space, stabilizing the mandible in an anterior and closed position, advancing the tongue, and increasing genioglossus muscle activity.
Variations in design include restricted elastic bands, clasps, or tubes for opening the mouth. These modifications act to relieve pressure and produce posterior extension of the maxillary component so as to modify the position of the soft palate or tongue. Dental impressions are generally required for mandibular advancing devices and anterior tongue retainers. However, prefabricated models can now be purchased. Proper fitting and alignment as well as regular patient follow-up are important components of therapy.
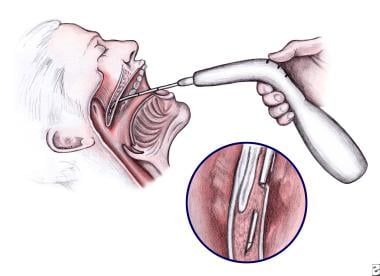
Palatal implants
A newer treatment option is the Pillar palatal implant, which was originally developed for the treatment of snoring. However, studies have demonstrated it has some efficacy in treating mild to moderate sleep apnea. [21, 22, 23, 24, 25] This system involves the placement of three mesh, polyethylene terephthalate implants, 18 mm × 2 mm each, within the soft palate muscles under local anesthesia (see the images below). These permanent implants improve snoring by stiffening the palate and decreasing its vibratory movement during inspiration.
Indications
Millions of Americans are affected by sleep-disordered breathing (SDB). Various treatments are available, depending on disease severity, patient anatomy, and natural inclination regarding treatment options. Some patients are claustrophobic and cannot use continuous positive airway pressure (CPAP) but can tolerate oral appliances. Others may fear surgery or simply want surgery as the last option.
Oral appliances are simple, effective, and inexpensive and should be considered as potential treatment by any otolaryngologist who treats patients with snoring or sleep apnea. Treatment with oral appliances begins with an initial consultation and examination.
Close collaboration with a dentist is recommended when oral appliance therapy is being considered. The patient’s available dental records should be acquired.
Indications for oral appliance therapy
These prosthetic devices are indicated for patients with the following:
-
Simple snoring problems
-
Upper airway resistance syndrome (UARS)
-
Mild, moderate, or severe obstructive sleep apnea (OSA)
Contraindications for oral appliance therapy
Patients with the following conditions should not receive oral appliance therapy:
-
No dentition
-
Limited dentition (highly dependent on number, placement, and condition of remaining teeth to anchor the device)
-
Active dental disease
-
Minimal protrusive range
-
Children
-
Acute temporomandibular joint dysfunction (TMJD) symptoms (case-by-case basis)
-
TMJD arthritis
-
Obvious psychologic aversion to structures in the oral cavity
-
Moderately limited dexterity
-
Limited mental capacity
Although tongue position and tonsil size can influence the success of the Pillar implants (see Design Features), no other contraindications have been identified to date.
Research Evidence
Studies related to the use of prosthetic devices, such as oral appliances and Pillar palatal implants, are briefly discussed.
Oral appliances in sleep-disordered breathing
Oral appliances find their greatest success when utilized for simple snoring, upper airway resistance syndrome (UARS), and mild to moderate obstructive sleep apnea (OSA). [26, 27, 28, 29] Improvement of snoring occurs in a high proportion of patients, with complete resolution in a smaller subset. In fact, subjective improvements in snoring are reported in most case series with oral appliances. Approximately 50% achieve an apnea-hypopnea index (AHI) of less than 10, and patient-reported compliance rates are 75-90%. A large literature review by Lowe et al indicated that, as a group, oral appliances were effective in mild to moderate OSA with a 75% compliance rate. [14]
A study by Pancer et al of the Thornton anterior positioner (TAP) demonstrated effectiveness of the adjustable device in patients with mild to moderate sleep-disordered breathing (SDB). [30] Of 75 patients evaluated by polysomnography, with and without the appliance, 38 patients achieved resolution of their OSA with the device alone. In an additional 31 patients, the AHI was reduced from 54 ± 31 to 20 ± 12. [30] Univariate regression analysis demonstrated an inverse correlation between the percentage improvement of AHI and both baseline AHI and body mass index (BMI). No correlation with age was noted.
In addition, although baseline low-oxygen saturations were similar, patients who experienced a treatment response also had an improvement in their oxygen saturations, whereas nonresponders had no significant change. [30] In this study, 86% of patients continued to use the appliance after a mean follow-up of 350 days. These patients were very satisfied (60%) or moderately satisfied (27%) with the device. Complications occurred in 26% of patients but were minor and not unexpected (eg, tooth and/or jaw discomfort, excess salivation). [30]
A study by Okuno et al found that in patients with OSA who underwent treatment with oral appliances, the mean AHI decreased from 22.6/hour at diagnosis to 10.0/hour at follow-up. Greater severity of OSA, a higher body mass index (obesity), and older age correlated with reduced effectiveness of oral appliance use. [31]
A study by Knowles et al of military patients with obstructive sleep apnea (OSA) who underwent treatment with oral appliance therapy found that the condition was successfully controlled in 85.5% of these individuals. According to the investigators, there is a moderate correlation between a less severe (ie, higher) baseline O2 nadir on diagnostic polysomnography and the likelihood that oral appliance therapy will succeed. [32]
A cohort study of 35 patients evaluated the efficacy of the Dynamax oral appliance in mild to moderate OSA. [33] An overall compliance rate of 60% was reported, with bed partners describing "improved snoring" in 70% of the participants. Ten patients had tried continuous positive airway pressure (CPAP) before the prosthesis; 80% of these patients cited easier tolerance of the oral appliance. [33] Epworth scores were improved, as were overnight oximetry measurements. Polysomnography was not used to evaluate changes in OSA parameters such as AHI.
White and Shafazand compared the effectiveness of mandibular advancement devices and CPAP in a randomized trial of 126 adults, concluding that in adults with moderate to severe OSA, the devices yielded similar results to CPAP in the short-term. [34] (Although research indicates that in general, CPAP is more effective than oral appliances against OSA. [19] )
A literature review by Zhang et al indicated that oral appliances can significantly increase the percentage of time spent in rapid eye movement (REM) sleep in patients with severe OSA. In addition, severe OSA patients with adjustable oral appliances showed significant improvement in their Epworth Sleepiness Scale (ESS) scores. However, similar to the statement above, CPAP devices were found to provide better overall reductions in OSA severity, producing significantly greater improvements in the AHI and ESS and in minimum oxygen saturation. [35]
A literature review by Serra-Torres et al indicated that mandibular advancement devices are effective in treating mild to moderate OSA/hypopnea syndrome, demonstrating success in the prevention of snoring and excessive daytime sleepiness, the reduction of the AHI, and the introduction of beneficial upper airway changes. The greatest improvements were seen with adjustable and custom-made mandibular advancement devices, as opposed to fixed and prefabricated appliances. [36]
Pillar palatal implants in snoring and OSA
One study assessed the efficacy of Pillar palatal implants in patients with socially significant snoring, without a history of OSA and found improvements in snoring, as rated by bed partners, following the procedure. [25] The outcome was assessed by the change in snoring severity measured by the bed partner using a 10-cm visual analogue scale, with 10 representing snoring that was unbearable. Snoring, rated by the bed partner, had a baseline mean value of 8.5, which decreased to 5 at 30 days and to 4.4 at 90 days posttreatment. [25] All patients tolerated the procedure well. At 90 days, 75% of patients and 90% of their bed partners advocated the procedure.
Another clinical trial that evaluated the efficacy of Pillar palatal implants in mild to moderate OSA demonstrated that 80% of patients achieved reductions in AHI values. [21] Nearly 60% of these patients achieved resolution of apnea.
Two randomized control trials compared Pillar palatal implants to sham procedures and placebo in treating mild to moderate sleep apnea and demonstrated a statistically significant change in AHI, quality-of-life–questionnaire scores and subjective snoring scores. [22, 23] However, the clinical significance of Pillar palatal implants efficacy alone in treating mild to moderate OSA remains questionable, as very few patients in these trials had a reduction of their sleep parameters to the often accepted definition of surgical "cure" (AHI decrease by ≥ 50% to presurgery as well as AHI < 20). Further studies regarding the efficacy of Pillar palatal implants in OSA are required.
Follow-up/Monitoring
Thoroughly instruct the patient in the use and care of the oral appliance, and follow up in 2-4 weeks. An objective analysis of progress includes pulse oximetry findings and polysomnography. It is recommended to follow up with the patient at 6-month intervals for as long as the prosthetic is used to check the status of the patient, the patient’s dentition, and the device itself.
Complications
Expected sequelae or problems and possible adverse effects with the use of oral appliances are briefly discussed below.
Expected sequelae or problems
Some patients may be unable to tolerate oral appliances. Many develop temporary adverse sensitivities of teeth, mastication muscles, and temporomandibular joint dysfunction (TMJD). Consider these problems a normal part of insertion, adjustment, and removal transition phases that should improve with time. Temporary bite changes after removal of the device last 5-60 minutes. Such changes should always resolve in a reasonable time with no discomfort. Some patients experience increased salivary production. Individuals who breathe through their mouths often experience dry mouth.
Pillar palatal implants may extrude over time, although the frequency of this occurrence is low (< 1% according to the manufacturer). The inflammatory reaction that ensues after insertion usually binds the three implants together and stabilizes their positions permanently.
Possible adverse effects
Many unusual problems may develop with the fitting or use of an oral appliance. Complications are often prevented from becoming significant issues by simple recognition of their possibility and appropriate response to initial complaints. Possible adverse effects include the following [37] :
-
Excessive salivation
-
Temporary discomfort with initial use (typically subsiding with regular use and adjustment of fit)
-
Temporomandibular joint (TMJ) discomfort
-
Broken and/or loosened teeth
-
Dislodgment of existing dental restorations
-
Tooth movement
-
Mouth sores
-
Periodontal complications
-
Root resorption
-
Muscle spasms
-
Otalgia
-
Permanent change in bite (anterior migration of mandible)
-
Ingestion or aspiration of broken pieces of the prosthetic
-
Changes in occlusive alignment
-
Xerostomia
Furthermore, the risk of worsening upper airway function (ie, worse apnea-hypopnea frequency), although rare, should be considered. Long-term consequences of oral appliance use are not well studied, but it is suggested that permanent tooth movement causing change in mandibular posture is common. [18, 38]
A study by Baldini et al found that in patients who had been using a mandibular advancement device for a median 4.6 years, long-term dentoskeletal side effects primarily took the form of moderate dental side effects. These included reductions in overbite (-0.5 mm), overjet (-0.7 mm), and maxillary incisor inclination (-2.5°), with mandibular incisor inclination increased 2.2°. The risk of overjet changes was higher in current smokers, while the decrease in overbite tended to be greater in patients with a preexisting anterior open bite. Mandibular incisor proclination tended to be more pronounced in association with the duration of treatment, and maxillary incisor retroclination was negatively correlated with propulsion. [39]
Adverse effects specific to soft-palate implants include difficulty speaking or swallowing and ear or jaw pain, all secondary to initial postprocedural swelling. A foreign-body sensation may also occur over time. These implants may also be extruded, thereby requiring replacement.
-
Illustration of the intraoral placement of 3 pillar implants in the soft palate.
-
Illustration of the technique of placing Pillar implants into the soft palate.