Overview
Skin transplanted from one location to another on the same individual is termed an autogenous graft, or autograft. Autografts consist of the entire epidermis and a dermal component of variable thickness. If the dermis is included in its entirety, the appropriate term is full-thickness skin graft. Because the complete dermal component is preserved in full-thickness grafts, more of the characteristics of normal skin are maintained following grafting. This is due to the greater collagen content, dermal vascular plexus, and epithelial appendages contained within full-thickness grafts when compared with split-thickness grafts. However, full-thickness grafts require more optimal conditions for survival because of the greater amount of tissue requiring revascularization. [1, 2]
Skin, also known as the integument, covers the entire external surface of the human body. The integumentary system is the body's principle interface with the surrounding world, and as such, it performs a multitude of specialized functions. It serves as a protective barrier preventing internal tissues from being exposed to trauma, radiation, temperature changes, and infection. Other important functions include thermoregulation through sweating and vasoconstriction or vasodilatation and control of insensible fluid loss. Restoration of an intact barrier is of critical importance following wounding and may be achieved in numerous ways, including grafting.
Skin grafting was performed in India 2000 years ago, but widespread interest did not develop until the 19th century. During the last 200 years, skin grafting has evolved into an essential component of the reconstructive surgeon's armamentarium. Grafting may be used to accelerate healing and reduce insensible fluid loss from burns and other wounds, reduce scar contraction, and enhance cosmesis.
Images depicting skin grafts can be seen below.
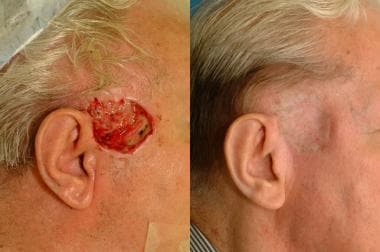 Patient is status post excision of a recurrent basal cell carcinoma. The skin defect was repaired with a split-thickness skin graft.
Patient is status post excision of a recurrent basal cell carcinoma. The skin defect was repaired with a split-thickness skin graft.
As with any procedure, before performing skin grafting, a thorough understanding of the pertinent anatomy is needed. The skin consists of 2 layers, the epidermis and dermis. The epidermis, the more external of the 2 layers, is stratified squamous epithelium consisting primarily of keratinocytes in progressive stages of differentiation from deeper to more superficial layers. The epidermis has no blood vessels, so it must receive nutrients by diffusion from the underlying dermis through the basement membrane, which separates the layers.
The dermis is a more complex structure and is composed of 2 layers, the more superficial papillary dermis and the deeper reticular dermis. The papillary dermis is thinner, consisting of loose connective tissue containing capillaries, elastic fibers, reticular fibers, and some collagen. The reticular dermis consists of a thicker layer of dense connective tissue containing larger blood vessels, closely interlaced elastic fibers, and coarse branching collagen fibers arranged in layers parallel to the surface. The reticular layer also contains fibroblasts, mast cells, nerve endings, lymphatics, and epidermal appendages. Surrounding the components of the dermis is the gel-like ground substance, composed of mucopolysaccharides (primarily hyaluronic acid), chondroitin sulfates, and glycoproteins.
Epidermal appendages serve an important role as a source of epithelial cells, which accomplish re-epithelialization when the overlying epithelium is removed or destroyed in cases such as partial-thickness burns, abrasions, or split-thickness skin graft harvesting. These intradermal epithelial structures, such as sebaceous glands, sweat glands, and hair follicles, are lined with epithelial cells with the potential for division and differentiation. They are often found deep within the dermis, and in the face may even lie in the subcutaneous fat beneath the dermis. This accounts for the remarkable ability of the face to re-epithelialize even the deepest cutaneous wounds.
Sebaceous glands, or holocrine glands, secrete sebum, which serves to lubricate the skin and make it more impervious to moisture. They are found over the entire surface of the body, except the palms, soles, and dorsum of the feet. They are largest and most concentrated in the face and scalp, where they are the site of origin of acne. Sweat glands, or eccrine glands, are found over the entire surface of the body, except the lips, external ear canal, and labia minora. They are most concentrated in the palms and soles of the feet. The normal function of these glands is to produce sweat, which cools the body via evaporation.
Apocrine glands are similar in structure but not identical to eccrine glands. They are concentrated in the axillae and anogenital regions. They probably serve a vestigial sexual function because they produce odor and do not function prior to puberty. The hair follicle is another important source of epithelial cells, and many of the other dermal appendages actually open into the hair follicle rather than directly onto the skin.
The skin varies in thickness based on its anatomic location and the sex and age of an individual. Skin is thickest on the palms and soles of the feet, while the thinnest skin is found on the eyelids and in the postauricular region. Male skin is characteristically thicker than female skin in all anatomic locations. Children have relatively thin skin that progressively thickens until the fourth or fifth decade of life, when it begins to thin. This thinning is primarily a dermal change, with loss of elastic fibers, epithelial appendages, and ground substance.
Graft Selection
Full-thickness skin grafts are ideal for visible areas of the face that are inaccessible by local flaps or for when local flaps are contraindicated. They retain more of the characteristics of normal skin, including color, texture, and thickness, when compared with split-thickness grafts. Full-thickness grafts also undergo less contraction while healing. This is important on the face, as well as on the hands and over joints. Additionally, full-thickness grafts in children are more likely to grow with the individual. (A study by Oh et al indicated that rapid growth in pediatric patients who undergo full-thickness skin grafts for palmar hand burns can be accommodated with a secondary full-thickness graft. This may be particularly necessary when the primary graft is located in the proximal digital crease and palmar web regions. [3] )
However, full-thickness skin grafts are limited to relatively small, uncontaminated, well-vascularized wounds and thus do not have as wide a range of applications as split-thickness grafts. Donor sites must be closed primarily or, more rarely, resurfaced with a split-thickness graft.
A retrospective study by Zlatarova et al reported that full-thickness skin grafts can be effectively used for eyelid reconstruction following carcinoma excision. The grafts, donor sites for which included the upper eyelid, preauricular area, and inner brachial area, proved viable in 95% of cases (37 of 39 patients), as evaluated 1 week postsurgically. Patients demonstrated normal lid function and, as assessed via graft color and lid position 6 months postoperatively, good to excellent cosmetic results. The few early complications that occurred, including graft hypertrophy, graft contraction, and partial graft failure, were addressed nonsurgically. [4]
A literature review by Saleki et al indicated that in repairing the donor site for radial forearm free flaps used in oral cavity reconstruction, full-thickness skin grafts offer better aesthetic outcomes than split-thickness grafts while producing comparable results with regard to infection, scarring, tendon exposure, skin graft loss, and donor site pain. [5]
In contrast, a literature review by Zhang et al reported that in repairing the donor site for radial forearm flaps, full-thickness grafts are more likely to fail than are split-thickness grafts, while providing no significant aesthetic advantages. Similar to the Saleki study, however, this one did report that the degree of pain and the rate of infection and tendon exposure did not significantly differ between the two types of graft. [6]
Donor Site Selection
Donor site selection is an important component of skin grafting and should take into account the characteristics of the recipient site. This is more important in full-thickness grafts than in split-thickness grafts because the graft in its new location retains more of the characteristics of the donor site skin. Match thickness, texture, pigmentation, and presence or absence of hair as closely as possible.
As the most common indication for full-thickness skin grafting is reconstruction of a cutaneous defect following neoplasia excision, one must be aware of the possibility of a cancerous lesion at the donor site. Meticulous inspection of the donor site is therefore warranted in order to minimize the possibility of transplantation of the carcinoma. These patients are typically at a higher risk for development of skin cancers, so this is not a trivial concern.
When grafting in children, be aware that donor skin that may grow hair later in life (eg, groin, axillae, thigh, chest) may develop undesirable hair growth in its new location. Donor sites chosen for full-thickness grafts should also be inconspicuous and easily closed primarily.
Full-thickness grafts may be harvested from the upper eyelid, nasolabial fold, preauricular and postauricular regions, and the supraclavicular fossa. These donor sites are most often used to close a wound on the face or neck. When harvesting from the face, harvesting bilaterally to maintain facial symmetry is often aesthetically preferable, even if it results in removing more skin than is necessary to cover the defect. Less common donor sites include hairless groin skin, dorsum of the foot, wrist flexion crease, and elbow crease.
A retrospective study by Kim et al indicated that the groin is a good donor site for full-thickness skin grafts with regard to the size of the graft, donor site morbidity, and graft survival. In the study, 50 patients underwent full-thickness skin grafts, taken from the groin, primarily for the repair of oral mucosal defects or donor-site wounds made from the harvesting of radial forearm free flaps; graft width and length ranged from 2-8 cm and 3-13 cm, respectively. The investigators found that in 47 patients (94%), the donor site healed well, with two patients suffering minor wound dehiscence and a third having severe wound impairment. Only two patients (4%) experienced delayed healing at the recipient site. [7]
Skin grafts harvested from the wrist flexion crease may give the unwanted appearance of a previous suicide attempt and probably should be avoided. Darker pigmented grafts may be obtained from the prepuce, scrotum, and labia minora. An often overlooked potential donor site for full- or split-thickness grafts is avulsed or surgically-removed skin.
When excising lesions from the face, and the majority of an aesthetic unit has been lost, the best results are often obtained by excising the remainder of that aesthetic unit and replacing it with a skin graft, even if this increases the amount of skin removed when compared with what is required to achieve an adequate margin around the lesion.
Wound Preparation
The most critical component of successful skin grafting is proper wound preparation. Failure to establish optimal physiologic conditions to accept and nourish the graft is the source of most graft failures. Skin grafts will not survive on tissue with a limited blood supply, such as bone, cartilage, tendon, or nerve. Skin grafts will survive on periosteum, perichondrium, peritenon, perineurium, dermis, fascia, muscle, and granulation tissue. Wounds secondary to radiation are also unlikely to support a graft. Treat the underlying conditions of wounds resulting from venous stasis or arterial insufficiency prior to grafting to increase the likelihood of graft survival.
The wound must also be free of necrotic tissue and relatively uncontaminated by bacteria. Bacterial counts greater than 100,000 per square centimeter are associated with a high likelihood of graft failure. To achieve an adequate wound bed, debridement, dressing changes, and topical or systemic antibiotics may be indicated prior to grafting.
Operative Technique
Careful operative technique is necessary to maximize graft survival. After initiation of appropriate anesthesia, the wound is first prepared for grafting. This includes cleansing of the wound with normal saline or diluted Betadine, judicious debridement, and meticulous hemostasis. Hemostasis may be achieved through ligation, gentle pressure, application of a topical vasoconstrictor (eg, epinephrine), or electrocautery. Minimize the use of electrocautery, as it creates devitalized tissue. The use of epinephrine at the donor or recipient site does not compromise graft survival.
Full-thickness skin grafts are harvested with a scalpel. The wound pattern is initially outlined over the donor region and is enlarged by 3-5% to compensate for primary contracture, which occurs because of the elastic fiber content of the graft dermis. The donor site may then be infiltrated with local anesthetic with or without epinephrine. Perform infiltration after the outline of the graft has been drawn on the skin to avoid distortion caused by the infiltrated volume.
After incising the pattern, the skin is elevated with a skin hook, keeping a finger of the nonoperating hand on the epidermal side of the graft. This provides tension and a sense of graft thickness while the operating hand dissects the graft off of the underlying subcutaneous fat. Any residual adipose tissue must be trimmed from the underside of the graft because this fat is poorly vascularized and will prevent direct contact between the graft dermis and the wound bed. Trimming of residual fat is best accomplished with sharp curved scissors with the graft stretched over the nonoperating hand until only the white glistening dermis remains. The donor site is then closed primarily with excision of dog-ears, as required.
Full-thickness grafts may be pie-crusted to allow egress of wound fluid from beneath the graft. These small stab wounds allow wound fluid to escape through the graft rather than it accumulating beneath the graft and preventing adherence. However, these openings do not prevent graft loss from an underlying hematoma. This technique is performed by making multiple stab wounds through the graft with a number 15 scalpel blade. Unlike meshing of split-thickness grafts, this does not serve to expand the surface area of the graft.
Once the graft has been harvested, reinspect the recipient site for hemostasis. Once this is achieved, the graft may be placed over the wound bed. Place the graft with the dermal side down. Although this sounds simple and obvious, dermis and epidermis can appear very similar without close inspection in lighter-skinned individuals. Also take care to prevent wrinkling or excessive stretching of the graft. The graft must then be secured in place to provide stability during initial adherence and healing. This most often is accomplished by suturing or stapling the graft to the surrounding wound bed. Avoid using staples, as they are painful to remove and may disrupt adherence of the graft to the wound when removed at approximately 7 days postoperatively. Absorbable sutures are preferable because they do not require removal.
Usually, 4 corner sutures are placed to hold the graft in the proper orientation. Then, a running suture is placed around the periphery. Passing the needle first through the graft and then through the surrounding wound margin is helpful to prevent lifting of the graft from the wound bed. Perfect epidermal-to-epidermal approximation ensures optimal cosmetic results, and the sutures should approximate, not strangulate, the skin edges. Occasionally, central sutures may be indicated to ensure adherence of the graft over a concave portion of the wound, but these are not required routinely.
A retrospective study by Gostian et al indicated that in reconstruction of the inner nasal lining, a full-thickness skin graft can be effectively secured to the underside of a forehead flap using multiple quilting sutures. The investigators reported that the technique did not increase the risk of serious complications, including flap necrosis. [8]
Dressings, casts, and splints
After a graft has been sutured, a dressing is chosen to provide uniform pressure over the entire grafted area through a nonadherent, semi-occlusive, absorbent material. [9] These dressings are meant to immobilize the graft, avoid shearing, and prevent seroma or hematoma formation beneath the graft. Tie-over bolster dressings are useful over joints or other areas where motion is difficult to avoid, in wounds with irregular contours, and in wounds located in places difficult to secure a dressing (eg, oral and nasal cavities, nasal tip).
These bolsters may be constructed from foam rubber, N-terface, Adaptic, or Xeroform folded over moistened cotton balls. When sewn into place, these provide a constant light pressure that is molded to the contour of the wound. These dressings are then secured by placing nonabsorbable sutures radially around the wound and tying them to each other over the bolster dressing. Alternatively, the sutures used to hold the graft in place may be nonabsorbable and left long enough to subsequently tie over the bolster.
A literature review by Steele et al, however, indicated that in full-thickness skin grafts, tie-over dressings are not superior to other fixation methods. Although the downward pressure from tie-over dressings has been considered advantageous in terms of promoting revascularization and discouraging the formation of hematomas and seromas, the pressure may not be greater than the capillary pressure and therefore may fail to reduce complications. The investigators cautioned, however, that their conclusions were drawn from a limited evidence base. [10]
Another dressing choice for an irregularly contoured wound or wound with high levels of exudate is the vacuum-assisted closure (VAC) sponge. This dressing conforms to the wound surface by suction and promotes skin graft adherence while removing exudate and edema from surrounding tissues. A nonadherent surface (eg, Adaptic) must be placed as an interface between the skin graft and the sponge to prevent peeling the graft off when removing the sponge. Grafts placed on the extremities may be managed with elevation and compression dressing for the entire extremity distal to the graft to avoid edema that can prevent graft adherence.
Casts or splints may also be useful in patients who are poorly compliant and in cases of grafting over a mobile surface to prevent motion and shearing forces that disrupt graft adherence. Burn netting may also be useful for securing dressings in difficult locations (eg, pelvic and shoulder regions). Finally, the graft may be treated open by placing no dressing except a layer of ointment to prevent desiccation. This technique is susceptible to hematoma or seroma formation beneath the graft because no pressure is applied. This technique is used only occasionally in facial grafting.
Graft adherence is maximal during the first 8 hours postgrafting, but the initial dressing should be left in place for 3-7 days unless pain, odor, discharge, or other signs of complication occur. When removing dressings, moisten them with normal saline to reduce adherence to the graft. The dressing is then carefully removed to prevent lifting the graft off of the underlying wound bed. Treat a hematoma or seroma encountered at dressing change by making a small incision over the collection and expressing the underlying contents. Rolling the fluid out under the edge of the graft is not recommended because it disrupts adherence of the entire graft, not just the area of hematoma or seroma formation.
The donor site must also be dressed appropriately at the conclusion of the operation. Full-thickness donor sites closed primarily are dressed in standard fashion.
Graft Survival
After graft placement, an initial adherence to the wound bed via a thin fibrin network temporarily anchors the graft until definitive circulation and connective-tissue connections are established. This adherence begins immediately and is probably maximized by 8 hours postgrafting. The period of time between grafting and revascularization of the graft is referred to as the phase of plasmatic imbibition. The graft imbibes wound exudate by capillary action through the spongelike structure of the graft dermis and through the dermal blood vessels. This prevents graft desiccation, maintains graft vessel patency, and provides nourishment for the graft. This process is entirely responsible for graft survival for 2-3 days until circulation is reestablished. During this time, the graft typically becomes edematous and increases in weight by 30-50%.
Revascularization of the graft begins at 2-3 days postgrafting by a mechanism that is not completely understood. Several theories exist, although the true mechanism may be a combination of these theories. Inosculation is the establishment of direct anastomoses between graft and recipient blood vessels. Several investigators have demonstrated vascular ingrowth of recipient bed vessels into the graft along the channels of previous graft vessels, a similar but not identical theory to inosculation. Still, others propose that random new vascular ingrowth of recipient bed vessels into the graft occurs without regard for previous graft vessels. Regardless of the true mechanism or mechanisms, full circulation to the graft is restored by 6 or 7 days postgrafting. Without initial adherence, plasmatic imbibition, and revascularization, the graft will not survive.
Several important aspects of skin-graft healing deserve further discussion. Wound contraction may present serious functional and cosmetic concerns, depending on location and severity. On the face, it may produce ectropion, retraction of the nasal ala, or distortion of the vermilion border. Over joints, it may limit functional range of motion. Contraction probably begins shortly following initial wounding, progressing slowly over 6-18 months following grafting. The myofibroblast is believed to be responsible for this contraction. In general, full-thickness grafts contract less than do split-thickness grafts. The deep dermal component is able to suppress myofibroblast function by an unknown mechanism. Contraction can be ameliorated by splinting or compression devices, such as facial masks or Jobst garments. These devices should be worn as much as tolerated each day for at least the first 6 months postgrafting and often even longer.
Epithelial appendages must be regenerated following grafting. Hair is more likely to grow from full-thickness grafts than from split-thickness grafts, but this is more likely to be a nuisance rather than desirable. Carefully select donor sites for full-thickness grafting regarding patterns of hair growth at the time of surgery and in the future of the individual. When deliberately grafting hair follicles, as in hair restoration or eyebrow or eyelash reconstructions, carefully angle the scalpel blade to incise the skin parallel to the orientation of the hair follicles. These structures are usually not oriented parallel to the skin surface and are transected if the incision is not oriented properly.
Sweat glands and sebaceous glands initially degenerate following grafting. Once again, they are more likely to regenerate in full-thickness grafts because they are transferred as an entire functional unit. Sweat gland regeneration is dependent on reinnervation of the skin graft with recipient bed sympathetic nerve fibers. Once this ingrowth has occurred, the skin graft assumes the sweating characteristics of the recipient site, rather than retaining the characteristics of the donor site.
Sebaceous gland regeneration is independent of graft reinnervation and retains the characteristics of the donor site. Prior to regeneration, the skin graft is lacking the normal lubrication of sebum produced by these glands. This makes the grafts more susceptible to injury. The grafts may appear dry and undergo scaling during this period. Patients frequently report pruritus. Recommend bland creams such as lanolin or cocoa butter to moisturize the graft and reduce itching. Full-thickness grafts become more soft and pliable with time as sebaceous gland regeneration occurs. These glands may also regenerate on the deep surface of skin grafts and present as milia. When encountered, unroof them with a needle.
Reinnervation of the graft occurs from the recipient bed and from the periphery along the empty neurolemma sheaths of the graft. Sensation returns to the periphery of the graft and proceeds centrally. This process usually begins during the first month but is not complete for several years following grafting. Full-thickness grafts reinnervate more completely than do split-thickness grafts. Reinnervation is always incomplete, and some degree of permanent derangement persists. Usually, the patient develops protective sensation but not normal perception. Pain is usually the first perceived sensation, followed later by touch, heat, and cold.
Pigmentation returns gradually to full-thickness skin grafts, and these grafts maintain pigment match to the donor site much more predictably than do split-thickness grafts. Generally, the recommendation is that the graft be protected from direct sunlight for at least 6 months postgrafting or even longer. Hyperpigmentation has been treated with dermabrasion and laser resurfacing.
Graft Failure
Skin grafting may be unsuccessful for numerous reasons. The most common reason for skin graft failure is hematoma beneath the graft. Similarly, seroma formation may prevent graft adherence to the underlying wound bed, preventing the graft from receiving the necessary nourishment. Movement of the graft, or shear forces, may also lead to graft failure through disruption of the fragile attachment of the graft to the wound bed.
Another common source of failure is a poor recipient site. The wound may have poor vascularity, or the surface contamination may have been too great to allow graft survival. Bacteria and the response to bacteria through the cellular and humoral immune responses lead to the release of enzymes and other harmful substances at the wound interface that disrupts the fibrin adherence of the graft.
Technical error may also yield graft failure. Applying the graft upside down results in complete graft loss. Applying excess pressure, stretching the graft too tightly, or handling of the graft in other traumatic ways can lead to partial or complete graft failure.
Biologic Skin Substitutes
No discussion of skin grafting would be complete without mention of alternative substances now available. [11] These biologic skin substitutes may be intended for permanent replacement or as a temporary biologic dressing until a permanent solution is available or normal skin regeneration and healing occur. These serve multiple functions. They decrease bacterial counts and promote a sterile wound. They also slow the loss of water, protein, and electrolytes. They reduce pain and fever, help restore function, and facilitate early motion. They provide coverage of vessels, tendons, and nerves to prevent desiccation. The ideal skin substitute is one with little or no antigenicity, lack of toxicity, tissue compatibility, and lack of disease transmission.
Cadaveric grafts and pig skin grafts are the historical skin substitutes with which most surgeons are familiar. Cadaveric grafts are termed allografts, or homografts, because they are transplanted from one organism to another within the same species. Pig skin grafts are termed xenografts, or heterografts, because they are transplanted from one organism to another of a different species. These may be prepared for use in several ways. They may be treated with glycerol and rapidly frozen with liquid nitrogen, or they may be lyophilized and freeze-dried.
Although cell viability is not ensured by the processing of these grafts, the structural details, proteins, and enzymes remain intact. Eventually rejected by the body, these grafts may be used as temporary biologic dressings, especially in extensive burns where skin graft donor sites are limited. In normal patients, these must be changed every 3 days to prevent a rejection response, but grafts in patients who are burned and relatively immunosuppressed may require removal only every 5 days. The theoretical risk of disease transmission with cadaveric grafts also exists.
Cultured epithelial cells have also been developed, both as autografts and as allografts. Cultured epithelial autografts require biopsies of the patient, followed by growth of these cells in culture. For this reason, they are not available for several weeks until they have grown to confluent sheets. This culturing process is currently quite costly and yields an extremely fragile sheet of cells that are very sensitive to infection. Allograft sheets are available immediately but share the structural weaknesses of the autografts, as well as the theoretical risk of disease transmission. These allografts are eventually rejected as well, but, in the interim, they can serve as a biologic dressing.
Allograft dermis has also been developed. This structure is not actually rejected by the body because it is rendered immunologically inert during processing. The body instead remodels and replaces it with a native dermal substitute. Cultured epithelial sheets or thin split-thickness grafts may be placed over this dermal substitute once it has become incorporated.
Bilayer collagen matrices are the latest development in this explosive field. These consist of a porous spongelike lattice of bovine collagen, chondroitin-6-sulfate, and glycosaminoglycans that serve as the dermal substitute. The dermal substitute layer serves as a scaffold that facilitates ingrowth of native fibroblasts and blood vessels with its eventual replacement. An overlying silastic membrane simulates the epidermis and serves to seal the surface to reduce insensible fluid loss. This membrane is transparent, allowing wound inspection, and progressively adheres less to the dermal layer as it is incorporated into the body. At about 3 weeks, the silastic layer may be peeled off and replaced with cultured epithelial cells or thin split-thickness skin grafts.
Current research in molecular biology, wound healing, and immunology is likely to yield even better skin substitutes with which to treat patients in the future. A time can be envisioned when a synthetic bilayer membrane of equal quality to that of skin will be available off of the shelf for application that is no more difficult than a dressing change.
-
Full-thickness skin graft to nasal dorsum.
-
Full-thickness skin graft to temple following excision of skin neoplasm.
-
Patient is status post excision of a recurrent basal cell carcinoma. The skin defect was repaired with a split-thickness skin graft.











