Overview of OSA
For patients in whom obstructive sleep apnea (OSA) is suspected or is diagnosed, examination of the upper airway is essential for determining an optimal treatment, as many variables are involved in the pathogenesis of the disease, making the choice of the correct treatment a complex one. [1]
An example of an upper airway examination is provided below.
 Oropharyngeal examination in a 35-year-old man reveals Mallampati grade I presentation of the palate's velum.
Oropharyngeal examination in a 35-year-old man reveals Mallampati grade I presentation of the palate's velum.
For more information, see the following:
Relevant Upper Airway Anatomy
The upper airway begins at the entrance of the nose and continues to the hypopharynx. The structures forming the upper airway are the nose and the pharynx with its 3 divisions (ie, nasopharynx, oropharynx, hypopharynx). Each of these areas has different pathologies that can produce stenosis of the airway and/or cause obstruction; sometimes, obstruction is found in several areas in varying degrees. [1] The lower airway begins in the trachea and continues to the bronchial tree.
Structures of special concern
Structures of the nose that are areas of special concern are the internal nasal valve, the septum, and the choana.
The nasopharynx is particularly important in children, because the adenoids are commonly hypertrophied, producing obstruction. Hypertrophied adenoids are the most common cause of obstructive sleep apnea (OSA) in children. [2]
In the oropharynx, the soft palate, tonsils, palatoglossal and palatopharyngeal arches, and the tongue are structures of concern. [3] In addition, the cross-sectional diameter of the pharynx can be smaller in many patients, playing an important role in the pathogenesis of OSA.
In the hypopharynx, the base of the tongue is the most influential structure.
Pathologic Conditions Associated With OSA
A prospective study by Magliulo et al found that of 50 patients with obstructive sleep apnea (OSA), 70% had nasal obstruction, 80% had at least one rhinosinusal pathology, and 18% and 26% had, respectively, allergic or nonallergic rhinitis. [4]
Nasal conditions that are associated with OSA include the following:
-
Deviated septum
-
Polyposis
-
Septal hematoma
-
Septal dislocation
-
Rhinitis
-
Turbinate hypertrophy
The following are conditions of the nasopharynx associated with OSA:
-
Carcinoma
-
Adenoidal hypertrophy
-
Lymphoma
-
Stenosis
-
Pharyngeal flap
-
Papillomatosis
Oral and oropharyngeal conditions associated with OSA include the following:
-
Hypertrophied tonsils
-
Elongated and/or thickened palate and uvula
-
Lymphoma of tonsils [5]
-
Lingual cyst
-
Lingual tonsillar hypertrophy
-
Macroglossia – Acromegaly
-
Micrognathia – Congenital or acquired
-
Lipoma of the neck
-
Hunter syndrome
-
Hurler syndrome
-
Head and neck burns
-
Papillomatosis
The following laryngeal conditions are associated with OSA:
-
Edema of epiglottis
-
Vocal cord paralysis
-
Laryngomalacia [6]
-
Collapse of aryepiglottic folds
Pediatric Upper Airway Abnormalities and Airway Obstruction
The following nasal conditions in children can cause upper airway obstruction:
-
Choanal atresia
-
Polyposis
-
Dermoid cyst
-
Tumors – Gliomas, teratomas, fibrous histiocytomas, encephaloceles
Nasopharyngeal conditions in children that can obstruct the upper airway include the following:
-
Adenoidal hypertrophy
-
Stenosis
-
Pharyngeal flap for cleft palate
-
Tumors
Pediatric oral and oropharyngeal conditions than can cause upper airway obstruction include the following:
-
Hypertrophied tonsils
-
Macroglossia due to lingual hemangioma
-
Macroglossia due to lingual lymphangioma
-
Micrognathia
-
Epignathus
-
Temporomandibular joint ankylosis
The following laryngeal conditions in children can cause upper airway obstruction:
-
Tracheal atresia
-
Intrinsic tracheal lesions
-
Extrinsic compression (goiter)
-
Laryngeal and tracheal webs
-
Kimura disease [7]
Charcot-Marie-Tooth disease has also been described in upper airway dysfunction. [8]
Overview of Physical Features and Evaluation
A systematic approach to the physical examination is recommended to avoid confusion. Briefly discussed are the general appearance and facial and cervical features. Examination of the nasal and nasopharyngeal and oral and oropharyngeal regions are discussed in separate sections.
General appearance
Many adult patients with obstructive sleep apnea syndrome (OSAS) are overweight or obese, and Pickwick syndrome in patients with obesity is associated with hypersomnolence and sleep apnea. Many obese patients also have a narrow pharynx, and patients with a wide and short neck are prone to develop OSA. [9] Waist and neck circumferences have a strong correlation with the severity of sleep apnea. However, children with OSA are not necessarily obese; rather, they are lacking in development and are generally underweight.
Elevated levels of interleukin-6 (IL-6), tumor necrosis factor-a (TNF-a), and insulin have been found in patients with excessive daytime sleepiness (EDS). Vgontzas et al proposed that these cytokines are mediators of daytime sleepiness. [10] Visceral fat was found to be a primary parameter linked to OSAS.
Facial and cervical characteristics
Anatomic characteristics commonly associated with OSAS include micrognathia, retrognathia, a short and thick neck, and abnormal positioning of the hyoid. Chronic nasal obstruction generally produces a long face. Certain craniofacial relationships have a greater potential to produce apnea than others. Lowe reported that a high apnea index was found in patients who had a large volume of the tongue and soft palate, a retrognathic mandible, an open-bite tendency between the incisors, and an anteroposterior discrepancy between the maxilla and mandible, and who were obese. [11]
Nasal and Nasopharyngeal Examination
Obstruction of the nasal passage can begin at the entrance. Rhinoscopy can reveal nasal septum deviations and problems at the valvular area.
Nose and nasal cavity
The area of highest resistance in the nose is the nasal valve; therefore, a small deviation in that area can produce a higher degree of obstruction than a larger deviation in any other part of the nose. External nasal valve collapse can be produced by weakening of the alar rim or by an extremely wide columella. The internal nasal valve is also a common source of obstruction. A small deflection of the nasal septum in this area produces more obstruction than in any other part of the nose. Deviations of the nasal septum can produce obstruction of the nasal passage. When the deviation is big enough, the contralateral inferior turbinate develops hypertrophy to compensate for the excessive widening of the nasal fossa. This hypertrophic turbinate sometimes produces obstruction by itself.
Allergic rhinitis or sinusitis may cause rhinorrhea. Rhinitis, caused by allergies or some other etiology, can produce constant obstruction of the nose. This problem is frequently aggravated at night when the patient is lying in bed because of the redistribution of fluids in the body. Nasal polyposis can be particularly troublesome. Many craniofacial syndromes cause midfacial hypoplasia that produces nasal obstruction. In many cases, visualizing the rhinopharynx is possible, although applying a topical vasoconstrictor beforehand is sometimes necessary. Less common pathologies, such as choanal stenosis or atresia, can produce obstruction of the airway. [12]
Nasopharynx
The nasopharynx can be better examined with a rigid or flexible endoscope, because the nasopharynx is located at the bottom of the nasal cavity. The most common problem in this area is adenoid hypertrophy, which can be large enough to produce nasal obstruction. Adenoid hypertrophy is normal in children aged 6 months to 5-6 years; absence of hypertrophy is abnormal at this age. Adenoid hypertrophy in adults is uncommon [13] ; however, several studies report this pathology in patients as old as 52 years. This author has found adenoid hypertrophy confirmed by histopathologic examination in patients as old as 63 years.
Nasal obstruction due to new onset of adenoid and/or tonsil hypertrophy in adults can be an initial sign of human immunodeficiency virus (HIV) infection. [14, 15] Tumors are an uncommon finding.
Oral and Oropharyngeal Examination
Dental anomalies, such as open-bite deformity or micrognathia class II occlusion, are easy to detect. A high arched palate is common in patients with chronic nasal obstruction. Gum size is important, because hypertrophic gums are generally associated with chronic oral respiration.
Palate
The velum of the palate is particularly important for the pathology of airway obstruction. A long or flaccid velum can produce obstruction. The soft palate is frequently elongated, increasing the possibility of snoring. Many patients have pharyngeal and palatal edema after sleep because of the snoring-induced trauma. Upon examination, the patient is asked to open the mouth and extend the tongue to assess the length of the soft palate.
The Mallampati classification is used to describe the size of the palate and its relationship to the rest of the pharyngeal structures (see the images below). This classification helps to predict the difficulty of orotracheal intubation. The uvula in patients with obstructive sleep apnea (OSA) is generally larger than that of the normal population, due to edema and thickening of the covering epithelium. [16] In addition, the uvula of snorers and OSA patients contains less muscle than that of nonsnorers and can sometimes produce obstruction because of the edema.
 Oropharyngeal examination in a 35-year-old man reveals Mallampati grade I presentation of the palate's velum.
Oropharyngeal examination in a 35-year-old man reveals Mallampati grade I presentation of the palate's velum.
 Oropharyngeal examination in 45-year-old man reveals Mallampati II presentation of the palate's velum.
Oropharyngeal examination in 45-year-old man reveals Mallampati II presentation of the palate's velum.
 Mallampati III presentation in a 24-year-old woman. Notice how the palatal arches cannot be visualized.
Mallampati III presentation in a 24-year-old woman. Notice how the palatal arches cannot be visualized.
Tongue
The tongue plays a major role in the pathogenesis of snoring and apnea. The lingual tonsils can be hypertrophied, and tumors may be present, such as those developed from a lingual thyroid. The epiglottis can prolapse during inspiration, producing airway obstruction. Catalfumo reported this problem in 11.5% of patients in whom a uvulopalatopharyngoplasty (UPPP) was unsuccessful. [17] These patients were treated with a partial epiglottidectomy with laser. Another factor is the degree of redundancy of the mucosa in the arytenoid-aryepiglottic fold area, which is correlated with an increase of the apnea index when the mucosa is markedly redundant. [18]
Macroglossia, an enlarged tongue, can be found in many patients with obesity and is commonly found in patients with Down syndrome. The tongue can be so large that it produces airway obstruction and has to be reduced with surgery. The base of the tongue is more commonly involved in the pathogenesis of obstruction. No direct correlation between tongue size and the apnea-hypopnea index (AHI) has been discovered. [19]
Oropharynx
The overall width of the pharynx is particularly important. The hypopharynx is affected by reduction in the width of the pharynx because of obesity, and drainage along the posterior wall of the pharynx is commonly correlated with adenoid hypertrophy. Tonsillar hypertrophy can produce airway obstruction (see the image below), a pathology that is more common in children but that has also been described in adults. Tonsillar hypertrophy occurs most commonly in pedunculated tonsils that rotate toward the pharynx when the patient lies down. [20] The tonsils do not have to be very large; however, a statistically significant correlation between tonsil size and respiratory disturbance index has been found. [21]
 Oropharyngeal examination in a 29-year-old man reveals airway obstruction due to tonsillar hypertrophy.
Oropharyngeal examination in a 29-year-old man reveals airway obstruction due to tonsillar hypertrophy.
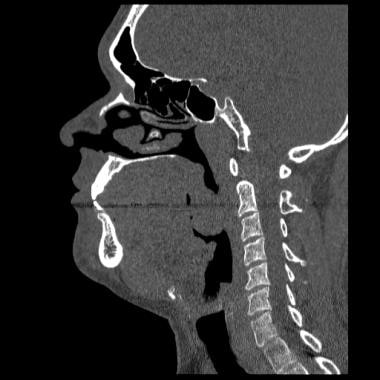 Tonsillar hypertrophy in a 34-year-old male, shown on a sagittal computed tomography (CT) scan. Polysomnography demonstrated an apnea-hypopnea index (AHI) of 80/h.
Tonsillar hypertrophy in a 34-year-old male, shown on a sagittal computed tomography (CT) scan. Polysomnography demonstrated an apnea-hypopnea index (AHI) of 80/h.
Perhaps the most important factor in OSA is the collapsibility of the pharynx. Most persons with OSA have a decreased tone of the pharyngeal muscles. This allows the pharynx to collapse even with small levels of intrapharyngeal negative pressure (see Flexible Nasopharyngoscopy). Micrognathia can be a life-threatening pathology in some patients, such as those who have Pierre-Robin syndrome. In certain circumstances, temporary glossopexy may need to be performed to avoid asphyxia until a secure airway is obtained.
A retrospective, multicenter cohort study by Huyett et al indicated that in patients with OSA, detection via drug-induced sleep endoscopy (DISE) of complete tongue-related obstruction was associated with a higher rate of response to treatment with hypoglossal nerve stimulation (HNS) than was partial or complete lack of tongue obstruction (78% vs 68%, respectively). The investigators also reported that a finding on DISE of complete oropharyngeal lateral wall–related obstruction was linked to a lower response rate than that found in cases of partial or absent wall-associated obstruction (58% vs 74%, respectively). Patients were considered to have responded to HNS if there was a reduction in the AHI of at least 50%, to less than 15 events/hour. [22]
Hypopharynx
Examination of the hypopharynx requires the use of a laryngeal mirror, flexible endoscope, or a magnifying laryngoscope. A gag reflex that is very intense is a common problem in some patients and can make performing the examination of the hypopharynx difficult or impossible. Flexible nasopharyngoscopy is the method of choice in these patients (see Flexible Nasopharyngoscopy). The size of the hypopharynx can be decreased because of alterations at the base of the tongue, and the diameter of the hypopharynx is decreased in obese patients.
Friedman Staging System for OSA
The Friedman classification is intended to identify prognostic indicators that will lead to stratification of patients likely to have successful uvulopalatopharyngoplasty (UPPP) versus those who are destined to failure of this treatment. [23] This classification considers the individual’s palate position, tonsil size and body mass index (BMI).
The Friedman palate position type as follows:
-
Allows visualization of the entire uvula and tonsils/pillars
-
Allows visualization of the uvula but not the tonsils
-
Allows visualization of the soft palate but not the uvula
-
Allows visualization of the hard palate only
Tonsil size is determined as follows:
-
The tonsils are hidden within the pillars.
-
The tonsils are extended to the pillars.
-
The tonsils are extended beyond the pillars but not to the midline.
-
The tonsils are extended to the midline.
The BMI is determined to be less than or greater than 40 kg/m2.
The table below uses the palate position, tonsil size, and BMI to determine the patient’s clinical OSA stage. [23] In a study with 134 patients, Friedman et al found that patients in stage I have the better chance to improve the apnea-hypopnea index (AHI) and the minimum arterial oxygen saturation (SpO2) after UPPP. [23] Patients in stage II have a low probability to improve AHI but have an improvement in minimum SpO2. Patients in Stage III didn’t have any improvement in AHI or minimum SpO2 after surgery.
Table. Friedman Staging System for Obstructive Sleep Apnea (Open Table in a new window)
|
Friedman Palate Position |
Tonsil Size |
Body Mass Index (kg/m2) |
Stage I |
1 |
3,4 |
< 40 |
2 |
3,4 |
< 40 |
|
Stage II |
1,2 |
0,1,2 |
< 40 |
3,4 |
3,4 |
< 40 |
|
Stage III |
3 |
0,1,2 |
Any |
4 |
0,1,2 |
Any |
|
Any |
Any |
Any |
Diagnostic Considerations
Most of the characteristics discussed in Physical Evaluation are suggestive of sleep apnea; however, none is considered pathognomonic of the disease. Radiologic examination and polysomnography are necessary to complement the study and are of particular importance in choosing the best treatment for the patient.
A study by Woodson and Nagnuma found no correlation between Mallampati presentation and Müller maneuver and the apnea-hypopnea index (AHI), [24] but the same study established a correlation between AHI and body mass index (BMI), posterior wall redundancy, and endoscopic retropalatal size. However, the sensitivity (50-60%) and specificity (63-70%) of the clinical impression are low.
In search of a decision rule for obstructive sleep apnea (OSA), Tsai et al found that patients with a cricomental distance of 1.5 cm or less, a pharyngeal grade II, and an overbite had a positive predictive value of 95% for OSA and a negative predictive value of 49%. A cricomental space of more than 1.5 cm excluded OSA. [25]
A magnetic resonance imaging (MRI) study by Savoldi et al indicated that in children and adolescents, the degree of OSA and severity of upper airway obstruction, during induced sleep, are negatively correlated with the maxillary basal bone width. The study also determined that in these patients, the severity of OSA and airway obstruction, during induced sleep, is most significantly predicted by “[s]tatic measurement of the nasopharyngeal and retropalatal laterolateral width of the airway in awake patients.” In addition, the investigators reported that in awake patients, static and dynamic airway evaluations differed with regard to the level of collapse, indicating that diagnosis and treatment planning could be improved with complementary dynamic assessment. [26]
Airway Resistance Measurement and Manometry
Superior airway resistance measurement and manometry were developed to evaluate the difference in pressure in the areas with high possibility of collapse (ie, hypopharynx, oropharynx, the region of the velum of the palate). The relative pressures in these areas are compared with the pleural pressure measured through the esophagus. Although this test may be performed during polysomnography, it is not commonly used because of its complexity.
Anterior rhinomanometry has been found to have a high sensitivity (91%) and specificity (96%) to detect sleep apnea in children with adenotonsillar hypertrophy and a nasal resistance of 0.59 Pa/cm3/s. [27]
OSA Imaging Considerations
Different imaging methods for the evaluation of patients with obstructive sleep apnea (OSA) have been tried. Radiologic evaluation should aid in making a correct diagnosis and in planning the appropriate treatment. [28] This, however, is not always the case. The anatomy of the pharyngeal walls should be correctly evaluated using the various diagnostic tools available. The airway was previously evaluated using measurements of electromyographic activity during sleep and intrapharyngeal pressure. However, these methods did not accurately represent the behavior of the pharyngeal structures surrounding the airway. Currently, different methods are used to provide a better understanding of the airway, such as acoustic reflection, fluoroscopy, cephalometry, computed tomography scanning, and magnetic resonance imaging. The advantage of these methods is that they are not invasive, although some of them involve exposure to x-ray radiation.
Nasopharyngoscopy provides an image of the upper airway, and dynamic tests can be performed. The only drawback is that nasopharyngoscopy is invasive, although the discomfort produced by the instrument has been reduced considerably with the new slimmer models.
Flexible Nasopharyngoscopy
Flexible nasopharyngoscopy is popular for obstructive sleep apnea (OSA) examination. This modality allows examination of the nose, all portions of the pharynx, and the larynx—in one procedure. In addition, when performing the nasopharyngoscopy, dynamic tests are possible.
Beginning in the rhinopharynx, the Passavant sphincter is evaluated during the closure of the velum of the palate. Afterward, the patient is asked to perform Müller maneuver, which is useful to assess the collapsibility of the pharynx. The Müller maneuver is performed with the nasopharyngoscope in the pharynx. The patient is asked to breathe while the lips are closed and the physician closes the nasal valves with his/her fingers. In this way, a negative pressure is created in the pharyngeal area, allowing evaluation of the retropalatal, retroglossal, and retroepiglottic spaces. [29] Endoscopy can also be performed with the patient under sedation to simulate sleeping conditions. Some authors doubt that these studies improve the treatment outcome. [30] However, if the area of obstruction is unclear, nasopharyngoscopy under sedation can be a useful tool. [31, 32]
The base of the tongue and the glossoepiglottic recesses are examined by asking the patient to extend his/her tongue. Evaluating the diameter of the pharynx and the characteristics of the epiglottis is also possible.
Advantages of nasopharyngoscopy include the following:
-
It does not involve radiation exposure.
-
Performance of dynamic tests is possible.
-
It is useful to evaluate the obstruction at the retropalatal and retroglossal levels.
-
It is easily reproducible preoperatively and postoperatively.
-
The test may be performed with the patient in sitting or supine position.
-
The test may be performed with the patient awake or sleeping.
-
The test is widely available and relatively inexpensive.
Disadvantages of nasopharyngoscopy include the following:
-
It is an invasive technique, and it can produce some discomfort when introducing the nasopharyngoscope into the nose.
-
It gives an approximate idea of the pharynx, because it is not possible to make any measurements.
-
The evaluation depends on the experience of the examiner.
A prospective study by Huo et al indicated that fiberoptic nasopharyngoscopy during Müller maneuver (FNMM) and fiberoptic nasopharyngoscopy with simulation of snoring (FNSS) are both effective means of upper airway assessment in patients with OSA and hypopnea syndrome. In the study, which included 92 patients, daytime FNMM and FNSS detected retropalatal obstruction in all cases. The two techniques also agreed diagnostically regarding retroglossal obstruction in 72 patients but were found to provide differing information with respect to collapse patterns. [33]
Fluoroscopy
Fluoroscopy has the advantage of producing dynamic images with the patient seated or reclining, awake or sleeping. This technique is useful to evaluate the areas of obstruction in the supine position. However, fluoroscopy is not sensitive enough to measure changes in the cross-sectional size of the airway. Other drawbacks of the technique are that the patient has great exposure to x-ray irradiation and that performing sectional cuts of the area is not possible. This situation has made fluoroscopy impractical and has limited its use.
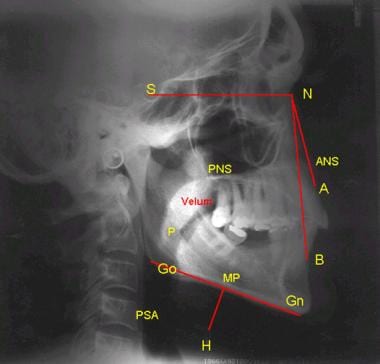
Cephalometry
This plain radiographic study is the most commonly used technique in patients with obstructive sleep apnea (OSA) (see the following image). Cephalometry is used to examine both the soft tissue and the osseous structures related to the airway. This modality is widely available, easy to perform, and has a low cost. One of the main advantages is that it is standardized. The exposure should be taken at the end of the expiration.
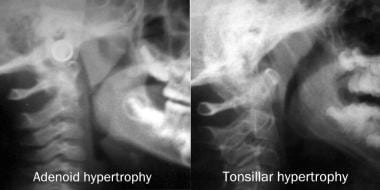 Plain radiographs of patients with adenoid hypertrophy (left) and another with tonsillar hypertrophy (right). Notice the reduction in the airway in the pharynx at the level of the base of the tongue cause by the tonsils. The adenoids cause obstruction in the rhinopharynx.
Plain radiographs of patients with adenoid hypertrophy (left) and another with tonsillar hypertrophy (right). Notice the reduction in the airway in the pharynx at the level of the base of the tongue cause by the tonsils. The adenoids cause obstruction in the rhinopharynx.
The main utility of cephalometry is to evaluate craniofacial abnormalities (eg, retrognathia, micrognathia). The most common cephalometric findings in patients with OSA are retrognathia, narrowing of the posterior airway space (PAS), elongation of the soft palate, increased volume of the base of the tongue, and a low position of the hyoid bone. A limitation of the study is that it produces a bidimensional representation of the airway, showing only the anteroposterior dimensions. Cephalometry does not provide any information on lateral structures. Researchers have found a statistically significant correlation between an increase of the apnea index (AI), a PAS-epipharynx distance less than 7 mm, and an MP-H distance (the distance from the mandibular plane to the most anterior and superior point on the body of the hyoid bone) greater than 27.4 mm. [18]
Several authors have found that the narrowing of the airway in patients with OSA takes place mainly in the laterolateral direction. This limits the utility of the study, but it still has a place in the evaluation of the patient and especially in those individuals in whom involvement of the mandible or maxilla is suspected to produce obstruction.
Special notice should be given to the adenoids, which can be evaluated more accurately in cephalometry because of the better alignment of the head. This avoids the distortion produced by rotation of the head, which can suggest a false hypertrophy of adenoids. Several classifications of adenoid hypertrophy exist. However, because of the variation of the pharyngeal size at different ages and the variation between different children, establishing a normal size of the retropalatal space is difficult. Viewing the tonsils in patients with tonsillar hypertrophy is also possible.
The following are reference points used in cephalometric analysis (see the image below):
-
S – This point is taken from the center of the sella turcica.
-
N – The nasion is the most anterior point of the frontonasal suture.
-
A – The subspinal point is the most depressed part of the superior incisive fossa.
-
B – The supramental point is the most depressed part of the inferior incisive fossa.
-
Gn – The gnathion is the most inferior point of the mandibular symphysis.
-
Go – The gonion is the most posterior and inferior point of the angle of the mandible.
-
H – The hyoid is the most anterior and superior point of the hyoid body.
-
MP – The mandibular plane is a plane joining the gonion with the gnathion.
-
PSP – This is the posterior nasal spine.
-
P – This is the most inferior and posterior point of the soft palate.
The following are angles and spaces measured in cephalometry:
-
The SNA angle measures the projection, anterior or posterior, of the maxilla. The reference range value is 82 ± 2°.
-
The SNB angle measures the position of the mandible. The reference range value is 80 ± 2°. Less than this is considered retrognathia.
-
The ANB angle measures the position of the maxilla with the mandible. The reference range value is 2°. This measures prognathism.
-
MP-H is the distance between the mandibular plane (MP) and the hyoid bone (H). The reference range is 11-19 mm. The longer the distance, the higher the possibility of the patient having OSA.
-
PSN-P is the length of the velum of the palate. The reference range value is 37 ± 3 mm.
-
G is the width of the velum of the palate. The reference range is 6-10 mm.
-
PAS is the posterior airway space or retroglossal space; the reference range is 10-16 mm.
-
The retropalatal space is the narrowest measurement between the posterior surface of the velum of the palate and the posterior pharyngeal wall.
Computed Tomography Scanning
Computed tomography (CT) scanning produces excellent resolution of images to evaluate both the soft tissue and the osseous structures of the pharynx-larynx complex. In CT studies, viewing the difference in shape of the pharynx between nonsnorers, snorers, and patients with obstructive sleep apnea (OSA) is possible, and this imaging modality has been used by many authors studying the pathogenesis of OSA. CT scanning has the advantage of producing axial and coronal cuts, as well as sagittal reconstructions. In addition, not only is taking measurements is possible, but volumetric reconstruction and 3-dimensional (3-D) imaging is also possible with the newer equipment (helical CT scanning).
The advantages of CT scanning are its wide availability and the quickness with which newer scanners can perform studies. Volumetric and 3-D reconstructions of the airway and other peripharyngeal structures are possible. The study is performed in the supine position.
Disadvantages of the study are that radiation is involved, limiting the number of studies that can be performed. (However, a study by Fleck et al determined that dynamic 3-D CT scanning of the upper airway in OSA patients can be performed with an effective radiation dose [under 0.38 mSv] comparable to or below that administered in clinical facial CT scanning. [34] ) CT scanning is also relatively expensive. The actual image is in the axial plane, so performing a reconstruction is necessary to obtain a sagittal image.
High-speed CT scanning (with electron beam) has been used for correlating the image with the different phases of snoring.
Magnetic Resonance Imaging
MRI is probably the best imaging study for patients with obstructive sleep apnea because of its excellent resolution in the supine position. This modality provides a detailed view of the fat and soft tissue of the pharyngeal walls and its relation with the airway. Obtaining sagittal, coronal, and axial images, as well as 3-dimensional reconstructions, is also possible, as are measurements of the different structures and their volume. MRI has the advantage of being radiation free, thus making performance of several studies possible.
Although the noise and the cumbersome design of the machine makes sleeping in it difficult, MRI has been used during sleep to study the effects of continuous positive airway pressure (CPAP) therapy. In addition, performing dynamic studies is possible because of faster equipment.
MRI is beginning to have a role in the evaluation of patients before and after surgeries such as uvulopalatopharyngoplasty (UPPP), resection of tongue base, or geniohyoid muscle surgery. MRI is an expensive study, especially with the newer technologies, making its price the real limit to the number of studies that can be performed.
MRI versus ultrasonography
A study by Kwan et al found that in patients with obstructive sleep apnea (OSA), as well as those without, tongue movement measurements obtained using ultrasonography were consistent with those derived via MRI. The investigators suggested that ultrasonography may be useful in evaluating dynamic airway muscle function and in determining how treatments for OSA, including CPAP and mandibular advancement splints, impact regional tongue movement. [35]
-
Oropharyngeal examination in a 35-year-old man reveals Mallampati grade I presentation of the palate's velum.
-
Oropharyngeal examination in 45-year-old man reveals Mallampati II presentation of the palate's velum.
-
Mallampati III presentation in a 24-year-old woman. Notice how the palatal arches cannot be visualized.
-
Oropharyngeal examination in a 29-year-old man reveals airway obstruction due to tonsillar hypertrophy.
-
Cephalometric analysis for obstructive sleep apnea.
-
Plain radiographs of patients with adenoid hypertrophy (left) and another with tonsillar hypertrophy (right). Notice the reduction in the airway in the pharynx at the level of the base of the tongue cause by the tonsils. The adenoids cause obstruction in the rhinopharynx.
-
Tonsillar hypertrophy in a 34-year-old male, shown on a sagittal computed tomography (CT) scan. Polysomnography demonstrated an apnea-hypopnea index (AHI) of 80/h.
Tables
What would you like to print?
- Overview of OSA
- Relevant Upper Airway Anatomy
- Pathologic Conditions Associated With OSA
- Pediatric Upper Airway Abnormalities and Airway Obstruction
- Overview of Physical Features and Evaluation
- Nasal and Nasopharyngeal Examination
- Oral and Oropharyngeal Examination
- Friedman Staging System for OSA
- Diagnostic Considerations
- Airway Resistance Measurement and Manometry
- OSA Imaging Considerations
- Flexible Nasopharyngoscopy
- Fluoroscopy
- Cephalometry
- Computed Tomography Scanning
- Magnetic Resonance Imaging
- Show All
- Media Gallery
- Tables
- References