Overview
The primary purpose of impedance audiometry is to determine the status of the tympanic membrane and middle ear via tympanometry. The secondary purpose of this test is to evaluate acoustic reflex pathways, which include cranial nerves (CN) VII and VIII and the auditory brainstem. This test cannot be used to directly assess auditory sensitivity, although results are interpreted in conjunction with other threshold measures.
Acoustic immittance is a measurement of energy or air pressure flow, which involves the ear canal, eardrum, ossicular chain, tensor tympani, stapedius muscle, cochlea, CNs VII and VIII, and the brainstem. Mass, mobility, and resistance of the outer and middle ear systems affect this test. The reciprocal of acoustic immittance is acoustic impedance. Particularly in earlier years, these measurements were performed in impedance rather than immittance measures; thus, the term impedance audiometry is sometimes used.
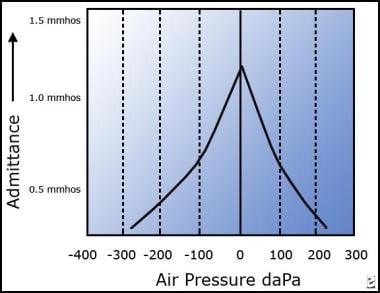
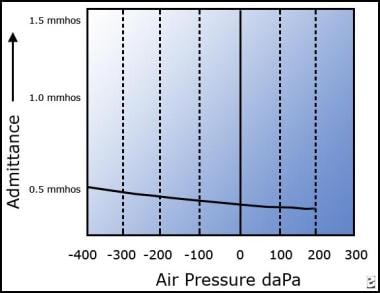
The image below depicts a type A tympanogram, suggesting normal function.
Acoustic immittance tests
The following tests are included in the category acoustic immittance tests:
-
Tympanometry (most commonly used)
-
Perilymphatic fistula test (efficacy questionable)
-
Acoustic reflex thresholds
-
Acoustic reflex decay
Acoustic reflex thresholds
An acoustic reflex threshold is a middle ear measurement of stapedius muscle response to higher intensity and adequate duration sounds for individual frequencies. Consider the softest sound that elicits a reflex contraction of the stapedius muscle as the acoustic reflex threshold. When the stapedius muscle contracts in response to a loud sound, that contraction changes the middle ear immittance. This change in immittance can be detected as a deflection in the recording.
Tympanometry records changes in middle ear immittance, while air pressure is varied in the ear canal and acoustic reflexes are recorded at a single air pressure setting (ie, the pressure setting that provided the peak immittance reading for that particular ear on the tympanogram). Ear canal pressure is maintained at that specific setting, while tones of various intensities are presented into the ear canal and immittance is recorded. A significant change in middle ear immittance immediately after the stimulus is considered an acoustic reflex.
A stapedial muscle contraction in response to an intense signal occurs bilaterally in normal ears with either unilateral or bilateral stimulation. This reaction occurs because the stapedial reflex pathway has both ipsilateral and contralateral projections. Acoustic reflex thresholds generally are determined in response to stimuli of 500, 1000, 2000, and 4000 Hz. For screening purposes, or for a general check of the pathway's integrity, usually test at 1000 Hz.
Types of acoustic reflex
For the ipsilateral or uncrossed acoustic reflex, stimulate the ear that is monitored for response. The assessed pathway involves the cochlea, ventral cochlear nucleus, CN VIII, CN VII and its motor nucleus, and the stapedius muscle—all on the side ipsilateral to the stimulus.
For the contralateral or crossed acoustic reflex, present the stimulus to the ear opposite the ear that is monitored for response. The assessed pathway involves the ipsilateral cochlea, ventral cochlear nucleus, and CN VIII; the pathway crosses the trapezoid body and then involves the contralateral medial superior olive, CN VII and its motor nucleus, and the stapedius muscle.
Variability of acoustic reflex thresholds
Thresholds vary according to individual hearing sensitivity and retrocochlear function. The range for acoustic reflexes in individuals with normal hearing averages 70-100 decibel (dB) sound pressure level (SPL). The greater the hearing loss, the higher the acoustic reflex threshold for conductive hearing loss. For sensorineural hearing loss, acoustic reflex thresholds may be within the normal range, particularly for mild-to-moderate hearing losses with recruitment.
Elevated or absent acoustic reflex thresholds (ie, >100 dB SPL) for any given frequency may suggest sensorineural or conductive hearing loss, facial nerve disorder, or middle ear disorder. Reflexes usually are absent or cannot be recorded if the patient has type B tympanograms; therefore, acoustic reflexes generally are not tested in these ears.
For example, if the ear canal is occluded with cerumen, a type B tympanogram with low volume will be recorded. In this case, acoustic reflexes cannot be measured because middle ear immittance is not being measured. (Cerumen blocks the signal.)
For a type B tympanogram with normal volume (as in otitis media) no pressure peak for immittance is obtained. The pressure between the ear canal and middle ear are not equilibrated, and acoustic reflexes cannot be recorded.
For a type B tympanogram with high volume (as in the presence of patent pressure equalization tubes or perforated tympanic membranes), an open exchange of air occurs between the ear canal and middle ear; thus, any contraction of the stapedius muscle cannot be measured.
Relevant Anatomy
The tympanic membrane is an oval, thin, semi-transparent membrane that separates the external and middle ear (tympanic cavity). The tympanic membrane is divided into 2 parts: the pars flaccida and the pars tensa. The manubrium of the malleus is firmly attached to the medial tympanic membrane; where the manubrium draws the tympanic membrane medially, a concavity is formed. The apex of this concavity is called the umbo. The area of the tympanic membrane superior to the umbo is termed the pars flaccida; the remainder of the tympanic membrane is the pars tensa (see the image below).
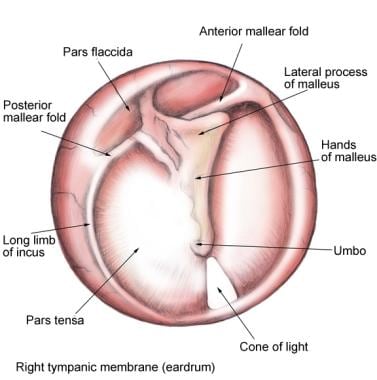 Tympanic membrane (TM): pars flaccida (superior to insertion manubrium) and pars tensa (remainder of TM).
Tympanic membrane (TM): pars flaccida (superior to insertion manubrium) and pars tensa (remainder of TM).
The eighth cranial nerve (CN VIII) or vestibulocochlear nerve is composed of 2 different sets of fibers: (1) the cochlear nerve and (2) the vestibular nerve. These 2 nerves are anatomically and physiologically different. The peripheral segments of the cochlear and vestibular nerves join at the lateral part of the internal auditory canal (IAC) to form the vestibulocochlear nerve. They are also joined by the facial nerve in the IAC. The length of the vestibulocochlear nerve, from the glial-Schwann junction to the brainstem, is 10-13 mm in the human male and 7-10 mm in females.
For more information about the relevant anatomy, see Ear Anatomy and Auditory System Anatomy.
Indications
Acoustic immittance tests can assist in identifying the following pathologies of the peripheral or central auditory systems:
-
Middle ear effusion
-
Perforation of the tympanic membrane, including patency of pressure equalization tubes
-
Tympanosclerosis
-
Hypermobility of the tympanic membrane
-
Eustachian tube dysfunction
-
Glue ear
-
Otosclerosis
-
Ossicular discontinuity
-
Acoustic neuroma or other CN VIII disorder
-
CN VII disorder
-
Hearing loss (a correlative, but not a direct measure)
-
Certain brainstem disorders
Contraindications
Low-frequency tympanometry is not recommended for infants younger than 7 months because their ear canal cartilage is so soft that misleading tympanometric results can occur.
For example, using a typical 226 Hz probe frequency, a normal-appearing, or type-A, tympanogram result may be obtained even in the presence of middle ear fluid because the soft ear canal yields to the pressure changes. Using a probe frequency of 1000 Hz appears more promising, based on recent data. However, the sensitivity and specificity of immittance audiometry in using a 1000 Hz probe to detect otitis media has not yet been determined. [1]
Research to develop accurate immittance audiometry protocols for infants younger than 7 months is ongoing. Some of this research involves using different probe frequencies in this age group, such as 1000 Hz, but no standardized clinical guidelines are currently available. The changes in tympanometric measures in infants continues to be an active area of research. [2, 3]
Technique
Tympanometry
Tympanometry measures sound reflection from the tympanic membrane, while the operator varies air pressure in the ear canal. Tympanometry aids assessment of the outer and middle ear system, including the eustachian tube.
Basic methodology
-
First, insert a probe with a soft plastic tip in the ear canal until an airtight seal is obtained.
-
Present a probe tone (typically 226 Hz) into the ear canal while altering air pressure of the external ear canal from +200 to -400 decapascal (daPa).
-
The maximum compliance peak occurs when ear canal and middle ear air pressures are equal, thus maximizing acoustic transmission through the middle ear. The compliance peak, therefore, indicates pressure of the middle ear and implies the efficacy of eustachian tube function. The height of the compliance peak reflects mobility, or conversely, stiffness, of the tympanic membrane and middle ear. Static compliance is the height of the tympanogram at its peak and is a measurement of system mobility.
Responses to tympanometry measurement
The Jerger system is the most commonly used classification system for tympanograms. While other systems have been proposed, none are in as widespread of clinical use.
A type A response suggests normal middle ear function, but it occurs in some otosclerotic ears, particularly in early stages. Compliance peak is -150 to +100 daPa, and immittance is 0.2-2.5 millimhos (mmhos) (see image below).
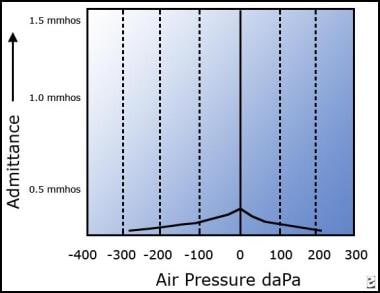
Type As (A shallow) suggests a stiffened middle ear system. Compliance peak is -150 to +100 daPa, and immittance is less than 0.2 mmhos. This type may suggest a glue ear, a thickened or scarred eardrum, or otosclerosis (see image below).
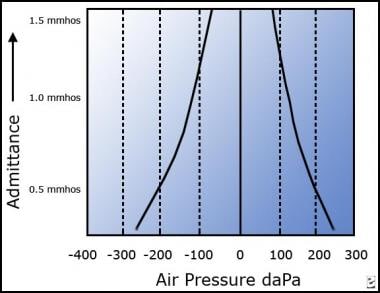
Type Ad (A deep) suggests a flaccid tympanic membrane, a middle ear system, or a disarticulation of middle ear ossicles. Usually a disarticulation of ossicles results in a compliance peak higher than the recording parameters (ie, off the chart). Compliance peak is -150 to +100 daPa, and immittance is more than 2.5 mmhos (see image below).
Type B is a flat trace with no observed compliance or immittance peak. Type B tympanograms must be interpreted in conjunction with ear canal volume readings (see image below). Average ear canal volumes for children are 0.42-0.97 mL. Average adult volumes are 0.63-1.46 mL.
 This graph depicts a type B tympanogram with no pressure peak. Type B tympanograms must be interpreted in conjunction with ear canal volume.
This graph depicts a type B tympanogram with no pressure peak. Type B tympanograms must be interpreted in conjunction with ear canal volume.
Type B (normal ear canal volume) usually suggests otitis media.
Type B (small ear canal volume) may suggest that the ear canal is occluded with wax/debris or that the immittance probe is pushed against the side of the ear canal.
Type B (large ear canal volume) suggests a patent pressure equalization tube or perforation of the tympanic membrane.
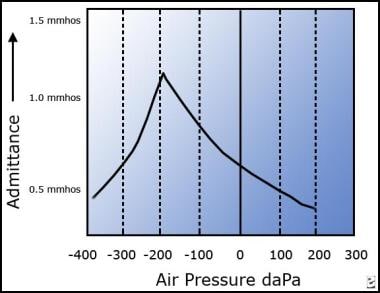
Type C suggests significant negative pressure in the middle ear system and may suggest developing or resolving otitis media. Additionally, this type indicates a malfunctioning eustachian tube. Immittance peak is measurable, but compliance peak is less than -150 daPa (see image below)
Eustachian tube function testing
Eustachian tube function testing can be implied by tympanograms. Type A tympanograms reflect normal middle ear pressure with an intact tympanic membrane. This situation only occurs if the eustachian tube is ventilating the middle ear. Similarly, type C tympanograms show significant negative middle ear pressure, implying eustachian tube dysfunction.
In patients with perforated tympanic membranes, type B tympanograms disclose high-volume readings and no information on eustachian tube dysfunction. However, in these patients pressure in the ear canal can be increased via the probe in the ear canal. Instruct the patient to swallow several times or yawn to determine if the eustachian tube can clear the pressure.
Several types of eustachian tube function testing exist and can be useful in evaluating function for divers or in evaluating the efficacy of treatments to improve eustachian tube dysfunction. [4]
Perilymphatic fistula testing
Assessment involves the outer, middle, and inner ear.
Testing implies presence or absence of a fistula (ie, an abnormal opening in the inner ear labyrinthine system).
Variation of ear canal pressure by the immittance probe (from +200 to -400 daPa) elicits a response. If vertigo or nystagmus occurs (Hennebert sign), the test result is positive.
The accuracy of this test in distinguishing symptomatic patients with patent fistulas from those without is questionable.
Acoustic reflex decay test
The acoustic reflex decay test is used to assess the integrity of CN VIII.
Using a stimulus of either 500 or 1000 Hz, a contralateral continuous tone is presented for 10 seconds at a stimulus level 10 dB above the acoustic reflex threshold for that stimulus frequency in that ear.
This suprathreshold acoustic reflex then is recorded over the 10-second stimulation period.
If the amplitude of the recorded deflection on the screen decreases by 50% or more within 10 seconds, the test is considered positive. Positive findings on this test may suggest a retrocochlear lesion (eg, vestibular schwannoma, acoustic neuroma). [5]
In some cases of muscular or neuromuscular disorder, tone decay results also may be positive secondary to muscle fatigue.
Pathologies Indicated By Acoustic Reflex Patterns
Key
See the list below:
-
Normal - Within expected limits
-
Abnormal - Absent or elevated
-
Ipsilateral - Stimulus and read-out in same ear
-
Contralateral - Stimulus presented to ear opposite to recording ear
-
Ear - Designates recording ear
Normal results
A normal ipsilateral acoustic reflex threshold (ie, within the 70-100 dB SPL range) suggests that a large conductive component is not present in that ear. If reflexes are present, sensorineural hearing loss is probably no worse than moderate in degree, and the ipsilateral acoustic reflex pathway is largely intact.
A normal contralateral acoustic reflex threshold (ie, within the 70-100 dB SPL range) suggests that a large conductive component is not present in either the stimulated or recording ear. If reflexes are present, sensorineural hearing loss in the stimulated or contralateral ear probably is no worse than moderate in degree, and the contralateral acoustic reflex pathway is largely intact. The presence of a normal contralateral reflex threshold does not provide any information regarding the sensorineural hearing thresholds in the recording or nonstimulated ear.
Absence of acoustic reflexes
As discussed previously, acoustic reflexes are generally absent or cannot be recorded in the presence of type B tympanograms. In the presence of severe-to-profound sensorineural hearing loss in the stimulated ear, acoustic reflexes may be absent secondary to insufficient stimulation. Similarly, a conductive component may attenuate the signal intensity, preventing sufficient stimulation in the stimulated ear or precluding a clear response in the recording ear. In a small percentage of patients, acoustic reflexes may be absent in the presence of type A tympanograms with no apparent otologic abnormality. The absence of acoustic reflexes warrants investigation.
Typical patterns for the interpretation of acoustic reflex abnormalities are as follows:
Efferent pattern
In an efferent pattern, reflexes are always abnormal in the recording ear (in this case, the second ear), regardless of which ear is stimulated. The following pattern may suggest a middle ear disorder with mild conductive hearing loss in the second ear or CN VII abnormality on the second ear side.
-
First ear contralateral - Normal
-
Second ear contralateral - Abnormal
-
First ear ipsilateral - Normal
-
Second ear ipsilateral - Abnormal
For example, a patient has a normal acoustic reflex threshold in the right ear with ipsilateral stimulation. The acoustic reflex threshold is also normal when the left ear is stimulated and the reflex is recorded again in the right ear. However, no acoustic reflex is present when the left ear is stimulated and the recording is taken from the left ear, and no acoustic reflex is present when the right ear is stimulated and the recording is taken from the left ear.
The normal responses recorded from the right ear in response to both ipsilateral and contralateral stimulation show that acoustic reflexes can be elicited with both right ear and left ear stimulation, thus both of those afferent pathways are intact. These responses also show that the right efferent pathway is intact because a response was recorded on that side.
The problem therefore seems to be specific to the efferent pathway on the left side such as with a CN VII or middle ear abnormality.
Afferent pattern
In an afferent pattern, reflexes are always abnormal in the stimulated ear (in this case, the second ear), regardless of which ear is the recording ear. The following pattern may suggest sensorineural hearing loss or acoustic schwannoma in the first ear.
-
First ear contralateral - Normal
-
Second ear contralateral - Abnormal
-
First ear ipsilateral - Abnormal
-
Second ear ipsilateral - Normal
For example, a patient has no acoustic reflex with ipsilateral stimulation of the right ear. When the left ear is stimulated, however, the acoustic reflex threshold is normal when read on the right side. The left ipsilateral reflex threshold is normal, but no response is recorded from the left ear when the right ear is stimulated. Therefore, both efferent pathways are intact because the right ear responds with left ear stimulation as does the left ear. The absence of response only occurs when the right ear is stimulated regardless of the recording ear. The problem thus appears to be the afferent pathway of the right ear as would be consistent with an acoustic neuroma.
Central pathway (brainstem) pattern
In the central pathway pattern, crossed reflexes are abnormal; ipsilateral reflexes are normal. This pattern may suggest a brainstem disorder, collapsing ear canals (if circumaural earphones are used for contralateral stimulation), or other central disorders, such as central auditory processing disorder (frequently not a clear correlation).
-
First ear contralateral - Abnormal
-
Second ear contralateral - Abnormal
-
First ear ipsilateral - Normal
-
Second ear ipsilateral - Normal
For example, a patient has normal acoustic reflex thresholds for both the right and the left ear when the reflex is recorded on the same side as the stimulus. However, responses are absent when the signal is presented to the ear opposite to the recording ear. Because the ipsilateral responses are present for both ears, the middle ears, cochleae, and CN VII and CN VIII are functioning bilaterally. The problem seems to occur only on the crossed pathways or at the level of the brainstem.
Unilateral/ipsilateral pattern
In the unilateral/ipsilateral pattern, all reflexes are abnormal except for the ipsilateral recording in 1 ear. This pattern may suggest middle ear disorder with moderate conductive hearing loss in the first ear, or it may suggest severe brainstem disorder affecting not only the crossed pathways but also the ipsilateral pathway on the first ear side.
-
First ear contralateral - Abnormal
-
Second ear contralateral - Abnormal
-
First ear ipsilateral - Abnormal
-
Second ear ipsilateral - Normal
For example, acoustic reflexes are absent when recorded from the right ear with either right or left ear stimulation. Reflexes also are absent in the left ear with right ear stimulation, but acoustic reflexes are normal with ipsilateral left ear stimulation. A moderate conductive hearing loss on the right side that affects not only the effective stimulus level reaching the cochlea but also the middle ear reflex response on the right side could cause these findings. However, a brainstem disorder large enough to affect not only both crossed reflex pathways but also the right ipsilateral pathway could cause these findings.
Global pattern
In the global patten, all reflexes (ipsilateral and contralateral) are abnormal. This pattern may suggest severe-to-profound bilateral sensorineural hearing loss, bilateral conductive hearing loss, or auditory neuropathy or other neural disorder affecting both ipsilateral and contralateral reflex pathways.
-
First ear contralateral - Abnormal
-
Second ear contralateral - Abnormal
-
First ear ipsilateral - Abnormal
-
Second ear ipsilateral - Abnormal
-
Type A tympanogram suggesting normal function.
-
Type As (A shallow) tympanogram depicting normal middle ear pressure but low compliance.
-
Type Ad (A deep) tympanogram depicting normal middle ear pressure but high compliance.
-
This graph depicts a type B tympanogram with no pressure peak. Type B tympanograms must be interpreted in conjunction with ear canal volume.
-
Type C tympanogram depicting normal compliance but significant negative pressure.
-
Tympanic membrane (TM): pars flaccida (superior to insertion manubrium) and pars tensa (remainder of TM).