Overview
The primary function of the middle ear is to offset the decrease in acoustic energy that would occur if the low impedance ear canal air directly contacted the high-impedance cochlear fluid. [1] When a sound wave is transferred from a low-impedance medium (eg, air) to one of high impedance (eg, water), a considerable amount of its energy is reflected and fails to enter the liquid. If no middle ear were present, only 0.1% of the acoustic wave energy traveling through air would enter the fluid of the cochlea and 99.9% would be reflected. [2]
For physiologic hearing to occur, a precochlear amplification system must be present to address the impedance mismatch that exists between air and water. Proper impedance matching requires the normal anatomy and functioning of an external ear and a middle ear with an intact tympanic membrane, a normal ossicular chain, and a well-ventilated tympanic cavity. Any dysfunction or disease of these components results in a conductive hearing loss, and clinically, an individual’s inability to properly hear sound.
What is Sound?
Sound represents a combination of waves that are generated by a vibrating sound source (or sources) and propagated through the air until they reach the ear. The most elementary sound wave is a sine wave that is produced by the regular to-and-fro vibration of the sound source. The sine wave can be characterized by several properties to include frequency and amplitude.
The image below illustrates a sine wave generated by a tuning fork. Starting from the neutral position, the wave moves to one extreme position then reverses direction, passes back through the neutral position, reaches the maximum opposite extreme position, and returns again to neutral position. This pattern of vibration is termed a cycle, and it is repeated as long as the tuning fork continues to vibrate. The period of the wave is the amount of time the wave takes to complete 1 cycle. The frequency of the wave is the number of cycles it completes in 1 second and is reported in units of cycles per second, or hertz (Hz). The amplitude of the wave is the distance between the wave's neutral position and its position of maximal displacement.
These wave characteristics have practical implications. Wave frequency corresponds to what we perceive as pitch, whereas amplitude corresponds to the loudness or intensity of the sound. The sounds we typically encounter in our environment are complex, consisting of a mixture of sine waves of various frequencies and intensities. These complex sounds may be described mathematically by a Fourier transformation. This process breaks down complex sounds into their composite sine waves. The ear performs the same type of analysis when it is stimulated by sound.
Sound intensity
The study of hearing is often concerned with measuring the minimum intensity of sound that can be detected by the ear. This is defined as the auditory threshold. Such measurements are routinely made in both the clinic and basic science laboratory; however, the broad range of sound intensities that can be detected by the ear complicates these measurements. Therefore, hearing science uses a measure of sound intensity that compresses the units of measurement into a practical range. This intensity scale uses the decibel (dB), which is defined as follows:
-
Number of decibels = 10 log10 (sound intensity/reference intensity)
-
Number of decibels = 20 log10 (sound pressure/reference pressure)
Note the following characteristics of the decibel scale:
-
It is a relative scale, based on a ratio that compares sound intensity or pressure with a standard reference level. The reference level used is the lowest sound pressure commonly detected by people and is equal to 20 uPa (2 X 10-5 N/m2), thus, the intensity level in decibel sound pressure level (SPL) = 20 log10 (sound pressure/20 uPa).
-
It is a logarithmic, not a linear, scale. Doubling sound pressure results in a 6-dB increase in measured sound pressure, while a 10-fold change in sound pressure is reflected by a 20-dB change in measured sound pressure.
-
The log of 1 is 0. Thus, 0 dB SPL does not correspond to the absence of sound but rather indicates that the sound pressure of the measured wave is equal to the reference sound pressure.
When the reference sound pressure level discussed above is used, sound pressure is described in units of dB SPL. Other reference values exist. The ear's ability to detect sound waves differs for different frequencies, with the human ear being maximally sensitive from 1-5 kHz. The average hearing thresholds for each hearing frequency serve as the reference values when determining auditory threshold in humans. When these reference values are used, thresholds are reported as dB hearing level (HL), with a value of 0 dB HL indicating that, at the frequency being tested, the measured auditory threshold is equal to that of the average human hearing level.
External Ear
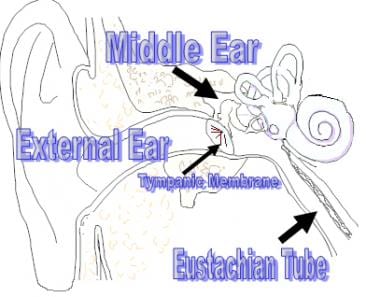
Although not anatomically part of the middle ear, the external ear plays a role in the function of the middle ear. See the image below.
Under normal circumstances, hearing is binaural. If a sound originates directly in front of an individual's head it is expected to reach both ears simultaneously. Conversely, a sound originating directly to an individual's right arrives at the right ear slightly before it reaches the left ear. Not only does the sound wave arrive somewhat later in the left ear, but its intensity is slightly attenuated by the shadowing effect of the head. These interaural differences in time and intensity, which are dependent on the sound wave's angle of incidence on the head, are more pronounced for sound differences above 1 kHz and serve as important clues for sound localization.
The collection of sound on the pinnae provides a spectral shape to the sound allowing the determination of both the elevation of the sound source and its origination in front of or behind the head. The ability of the pinnae to accurately localize sound in this manner is severely attenuated if one pinna is covered and absent if both pinnae are covered. Covering the pinnae does not, however, affect the ability to perceive the lateral origins of sound that are determined by time and intensity differences of binaural hearing. [3]
The external ear acts as a filter to reduce low frequencies, a resonator/amplifier to enhance mid frequencies, and a direction-dependent filter at high frequencies to augment spatial perception. [4] The pinna, conchal bowl, and external ear canal each contribute to the amplification of the sound wave. If a sound wave has an angle of incidence on the head of 45°, the peak amplification attributable to the pinna is 3 dB at 4 kHz. The concha provides a maximum gain of 10 dB at 4-5 kHz, while the ear canal provides a similar gain, peaking at 2.5 kHz. When taken together, the components of the external ear maximally amplify sound at frequencies from 2-5 kHz, with the maximal gain being 20 dB at 2.5 Hz. [5]
Middle Ear
Although the external ear does amplify and modify the spectrum of the sound wave, the middle ear makes the most significant contribution to this process. The tympanic membrane (TM) separates the external ear from the middle ear and plays an important role in transforming sound waves into mechanical vibrations that stimulate the inner ear. The tympanic membrane is an irregularly round 0.08 mm thick viscoelastic material that has a diameter about 10 mm. [6] The total surface area of the TM is 85 mm2 with a physiologically effective area of 55 mm2. [7] The tympanic membrane is attached at the umbo to the ossicular chain made up of the malleus, incus, and stapes that creates a mechanical advantage, ultimately eliciting a fluid wave through the round window into the fluid-filled cochlea of the inner ear. [8, 9, 10, 11]
Traditional teaching holds that the human middle ear acts as a pure transformer. The middle ear pressure gain resulting from this transformer action is usually specified at 27-30 dB. This is derived from the product of 2 structurally related factors: the area ratio (TM area divided by the stapes footplate area [22:1]) and the ossicular lever (the length of the manubrium of the malleus divided by the length of the long process of the incus [1.3:1]). Implied in a transformer analogy is the expectation that this gain is independent of frequency. Conventional teaching also holds that a phase difference must exist between the oval and round windows for optimal hearing.
Modifications of this theory have developed because of better understandings of TM motion/velocity, increased laxity of the malleal-incudal joint system above 1 KHz, ossicular coupling and acoustic coupling. The pressure gain provided by the normal middle ear (via ossicular coupling) is frequency-dependent. [12] The mean middle ear gain is about 20 dB between 250 and 500 Hz, reaching a maximum of about 26.6 dB around 1KHz and then decreasing at about 8.6 dB per octave at frequencies to near zero gain at 7 KHz and above. Sound pressure gain averages 23 dB. [1] Less amplification is required at higher frequencies to correct for the impedance of the cochlear fluids. Also, the stapes footplate movement is not entirely pistonlike but has an anterior-posterior rocking motion with rising frequency. [13]
Eustachian Tube
The proper function of the middle ear depends on the presence of a mobile tympanic membrane capable of vibrating in response to a sound wave. For the tympanic membrane to have maximal mobility, the air pressure within the middle ear must equal that of the external environment. The eustachian tube acts as a pressure release valve to adjust the middle ear pressure. Increasing positive pressure within the middle ear or negative pressure in the nasopharynx promotes the flow of air or secretions from the middle ear through the eustachian tube to the nasopharynx.
Conversely, positive pressure in the nasopharynx or negative pressure in the middle ear promotes air passage and/or reflux of nasopharyngeal secretion into the middle ear. If pressure equalization is not maintained, the ear drum retracts inwards if the middle ear pressure is less than that of the external environment (negative middle ear pressure). With positive middle ear pressure, when the middle ear pressure exceeds that of the external environment, the tympanic membrane balloons outward. Ear pain may occur if the middle ear is unable to equalize during acute external air pressure changes, such as when flying or scuba diving.
The eustachian tube extends from the anterior wall of the tympanic cavity to the lateral wall of the nasopharynx. In its resting state, the eustachian tube valve is closed because of the elastic forces of the tube and its supporting structures. The valve area within the nasopharynx dilates when the tensor veli palatini muscle contracts during pharyngeal swallowing and yawning. [14] Mathematical modeling of this process has shown that longer tube lumens open more easily than shorter ones, and elastic forces appear to do little to oppose this active process.
The ability of the eustachian tube to perform its functions of ventilation, protection, and drainage can be influenced by variations in its own structure and by the conditions of the middle ear and the nasopharynx. An abnormally compliant eustachian tube fails to protect the middle ear from reflux of nasopharyngeal secretions and is more prone to open with changes in air pressure in the middle ear or nasopharynx. If the valve remains open (a patulous eustachian tube), the person has autophonia, described as hearing their own breath sounds and, when speaking, the sensation of being a tunnel. This may be due to abnormal activity of the paratubal muscles, rapid weight loss due to anorexia nervosa, hormonal effects, pharyngeal tumor diseases, neuromuscular diseases, and physical or psychological stress. [15]
A partially or totally obstructed eustachian tube impedes passage of air or fluid. This may be anatomic or physiologic. Anatomic obstruction may be caused by adenoid disease, tumors, or hypertrophy of nasopharyngeal mucosa related to sinus disease, allergies, or laryngopharyngeal reflux . Physiologic obstruction is due principally to a failure of the tensor veli palatini muscle to function properly. [14] This tends to affect young children, especially those with cleft palates and craniofacial abnormalities. Eustachian tube dysfunction may cause significant middle ear disease such as otitis media, tympanic membrane atelectasis and perforations, and cholesteatoma formation. Hearing loss is often exacerbated because of both negative pressure and fluid within the middle ear attenuating the movement of the umbo. [16]
Muscles of the Middle Ear
The 2 smallest striated muscles in the body, the tensor tympani and the stapedius, are contained within the middle ear. The tensor tympani muscle attaches to the superior portion of the malleus, and the stapedius muscle emerges from the pyramidal eminence to attach to the upper portion stapes. Contraction of both muscles is primarily activated by acoustic stimulation of 70-90 dB above threshold. Reflex contraction with a latency of more than 10 ms stiffens the ossicular chain, reducing sound transmission by 5-10 dB, primarily at frequencies below 2kHz.
The stapedius is dominant in reducing sound transmission and altering acoustic impedance at the tympanic membrane. Other stimuli (eg, tactile stimulation of the auricle, change in head posture, anticipation of speech production) can also activate acoustic reflex contraction. Sensory stimuli elicit contraction via an involuntary reflex mediated by the central nervous system at the level of the superior olivary complex. The superior olivary complex sends out crossed and uncrossed fibers, allowing a unilateral sensory stimulus to elicit bilateral muscle contraction. Motor nerve fibers are carried to the tensor tympani via the fifth (trigeminal) cranial nerve and to the stapedius via the seventh (facial) cranial nerve.
Although the nature of the acoustic middle ear muscle reflex has been well established, the physiologic role of the reflex has remained unclear. A logical role for the reflex is protection of the cochlea from loud noises, but the degree of attenuation afforded by muscle contraction is minimal and concentrated in the low frequencies. In addition, the latency of the muscle contraction, which takes up to 25-35 ms, is such that it would fail to protect the ear from a sudden impulsive acoustic trauma.
Other possible functions of the middle ear muscles have been proposed, including alterations in the frequency spectrum of an acoustic stimulus, reduction in low frequency harmonics, and stabilization of the ossicular chain. These theories have led to the proposal that the stapedial reflex helps clarify high-frequency verbal recognition by modulating low-frequency sounds that might otherwise mask higher frequency sounds at elevated dB levels. Recent data have shown this not to be the case, as speech perception remains unaffected with or without a stapedial response. But another study looking at patients who had undergone argon laser stapedotomy with preservation of the stapedial tendon compared with patients without tendon preservation demonstrated that patients with tendon preservation showed a tendency to better results in the sound-noise ratio. [17]
Myoclonus of the stapedius and tensor tympani muscles may lead to objective tinnitus (ie, tinnitus heard by both the patient and the examiner). [18, 19] Some evidence suggests that the tensor tympani may be responsible for a reversed ipsilateral acoustic reflex. The reversed acoustic reflex pattern is a physiologic event, but one study suggests this reflex does not appear to be related to stapedius or tensor tympani muscle contraction. [20] The etiology of the reversed reflex is believed to be related to the system that contains the tympanic membrane, malleus, and incus and their ligaments but not the middle ear muscles.
Assessment of Middle Ear Function
Middle ear function is commonly assessed with a pure-tone audiogram and impedance testing.
Pure-tone audiogram
A pure-tone audiogram (PTA) is a test used to identify hearing threshold levels of an individual to determine the degree, type, and configuration of a hearing loss. PTA provides ear-specific thresholds and uses frequency-specific pure tones from 250-8000 Hz. The PTA uses both air and bone conduction audiometry to differentiate between a sensory-neural, conductive, or mixed hearing loss. An identifiable air-bone gap is consistent with a conductive hearing loss found in external or middle ear disease.
Tympanotomy impedance testing
This test measures changes in eardrum compliance because air pressure is varied in the external ear canal. Tympanometry indirectly assesses the middle ear system that includes the eustachian tube. Low-frequency tympanometry is not recommended for infants younger than 7 months because their ear canal cartilage is so pliable that misleading tympanometric results can occur. Using a probe frequency of 1000 Hz appears more promising, based on 2006 data. [21]
The modified Jerger classification is as follows:
-
Type A response suggests normal middle ear function with a compliance peak between -150 to + daPA with a normal immittance of 0.2-2.5 mmhos. A diminished (shallow) compliance peak with an immittance below 0.2 mmhos may be found in people with otosclerosis, a middle ear effusion, or a tympanic membrane thickening. An exaggerated (deep) compliance peak with an immittance above 2.5 mmhos demonstrates a flaccid tympanic membrane most consistent with ossicular disarticulation.
-
Type B is a flat trace with no observed compliance or immittance peak. These are interpreted in conjunction with ear canal volume readings. Average ear canal volumes for children are 0.4-1.0 mL. Average adult volumes are 0.6-1.8 mL.
Type B with a normal ear canal volume suggests otitis media.
Type B with a small ear canal volume suggests that the ear canal is occluded or that the immittance probe is pushed against the side of the ear canal.
Type B with a large ear canal volume suggests a perforation or a patent pressure equalization tube.
-
Type C suggests significant negative pressure in the middle ear consistent with eustachian tube dysfunction. An immittance peak is measurable, but the compliance is less than -150 daPa. This may be due to chronic eustachian tube dysfunction or acute early or resolving otitis media.
Acoustic reflex impedance testing
This is a middle ear measurement of the stapedius muscle’s contraction to high-intensity sounds for individual frequencies. The softest sound that elicits a reflex contraction of the stapedius muscle is the acoustic reflex threshold. When the stapedius muscle contracts in response to a loud sound, that contraction changes the middle ear immittance that can be detected as a deflection in the recording. Acoustic reflexes are recorded at a single air pressure setting determined by the peak immittance reading on the tympanogram. Ear canal pressure is maintained at that specific setting, while tones of various intensities are presented into the ear canal. A significant change in the immittance immediately after the stimulus is considered the acoustic reflex. [22]
The acoustic reflex should occur bilaterally in normal ears with either unilateral or bilateral stimulation, because the stapedial reflex pathway has both ipsilateral and contralateral projections. Elevated or absent acoustic reflex thresholds above 100dB SPL for any given frequency may suggest a hearing loss, or a facial nerve disorder. Reflexes are absent if the patient has a tympanic membrane perforation and may be absent with a middle ear effusion due no measurable immittance peak.
A study by Causon et al found that acoustic reflex threshold and growth did not correlate with lifetime noise exposure, suggesting that in audiometrically normal listeners, a routine clinical measurement of the acoustic reflex cannot provide a sensitive evaluation of the effects of noise exposure. However, the investigators did find acoustic reflex and growth to be associated with middle-ear compliance, with the thresholds and growth functions of the acoustic reflex being lower and steeper, respectively, in persons with a higher middle-ear compliance that is, nonetheless, in the clinically normal range. [22]
-
Sine wave.
-
Anatomy of the external and middle ear.