Overview
The eustachian tube (pharyngotympanic tube) connects the middle ear cavity with the nasopharynx. It aerates the middle ear system and clears mucus from the middle ear into the nasopharynx. Opening and closing functions of the eustachian tube are physiologically and pathologically important. Normal opening of the eustachian tube equalizes atmospheric pressure in the middle ear; closing of the eustachian tube protects the middle ear from unwanted pressure fluctuations and loud sounds. Mucociliary clearance drains mucus away from the middle ear into the nasopharynx, thus preventing infection from ascending to the middle ear.
Abnormal or impaired eustachian tube functions (ie, impaired opening or closing, defective mucociliary clearance) may cause pathological changes in the middle ear. This in turn can lead to hearing loss and other complications of otitis media. These pathological changes include recurrent acute otitis media and otitis media with effusion. Chronic retraction of the tympanic membrane may also lead to middle ear atelectasis and subsequent adhesive otitis media. A retraction pocket of the tympanic membrane secondary to chronic eustachian tube dysfunction may eventually evolve into cholesteatoma and potentially serious complications.
Embryology of the Eustachian Tube
The eustachian tube lumen develops in the embryo by the lateral extension of the endoderm of the first pharyngeal pouch as it touches the inner surface of the ectoderm of the first branchial cleft. During this process, the distal portion of the pouch expands, forming the tubotympanic recess, which will later evolve into the middle ear cavity. The proximal portion narrows to form the eustachian tube. This process takes place during the first 10 weeks of gestation.
The cartilage and muscles of the eustachian tube develop from the surrounding mesoderm during the ensuing weeks. The levator veli palatini and the tensor veli palatini muscles seem to develop earlier than the cartilage and glandular tissue.
The cartilaginous portion of the tube elongates during the middle and third trimester until it reaches approximately 13 mm in length at term. Other morphologic changes also occur during that time with further development of the glandular structures and folding of the epithelium.
As the skull base grows down, the angle of the eustachian tube changes gradually from horizontal to oblique. This process continues after birth and well into adulthood.
Anatomy of the Eustachian Tube
Cartilaginous and bony framework
The eustachian tube in the adult is approximately 36 mm long and is directed downward, forward, and medially from the middle ear. It consists of 2 portions, a lateral third (12 mm), which is a bony portion arising from the anterior wall of the tympanic cavity, and a medial two thirds (24 mm), which is a fibrocartilaginous portion entering the nasopharynx. The tube opens about 1.25 cm behind and slightly below the posterior end of the inferior turbinate.
The bony portion is widest at its tympanic end. It passes through the squamous and petrous portions of the temporal bone but narrows gradually to the isthmus, which is the narrowest part of the eustachian tube.
The cartilaginous portion consists of a plate of cartilage posteromedially. The cartilage bends forward to form a short flange. The rest of the anterolateral wall is formed by fibrous tissue. The apex or lateral end of the cartilaginous part joins the bony portion at the isthmus; the wider medial end lies under the mucosa of the nasopharynx and raises the mucosa to form the tubal elevation (torus tubarius). Just behind this elevation is a recess called the fossa of Rosenmüller, which is a common site of origin for nasopharyngeal carcinoma and occult primary tumors.
The cartilaginous eustachian tube is attached to the skull base in a groove between the petrous part of the temporal bone and the greater wing of the sphenoid.
The lumen of the eustachian tube is roughly triangular, measuring 2-3 mm vertically and 3-4 mm horizontally. The bony portion is always open; the fibrocartilaginous portion is closed at rest and opens only on swallowing, yawning, or forceful inflation.
The eustachian tube in infants measures approximately 18 mm in length. It is about half the size of the adult eustachian tube and is generally more horizontal and less angulated. The bony portion is relatively longer and wider in diameter, the nasopharyngeal end of the cartilaginous portion lies more inferiorly.
At its nasopharyngeal opening, the eustachian tube is lined by respiratory epithelium that includes columnar ciliated cells, goblet cells, and mucous glands. The respiratory epithelium blends with the middle ear mucosa in the bony portion of the tube.
A study by Ozturk et al found that the length of the mucosal surface of the posterior wall of the eustachian tube is longer than the anterior wall and, in pediatric specimens, that the posterior wall has more mucosal folds (microturbinates) than adult specimens. They concluded that these microturbinates may provide important protection and clearance functions for children and play a role in the pathogenesis of eustachian tube dysfunction (see Eustachian Tube Dysfunction). [1]
A study by Janzen-Senn et al found the eustachian tube to typically be longer in males than females, possibly because of differences in body size. The investigators also found the length of the right bony eustachian tube to be significantly greater than that of the left one. In addition, the eustachian tube was seen to grow shorter with age, with increases in the open length of the cartilaginous portion and the distance of the pharyngeal orifice from the conchae, particularly in persons aged 70 years or older. The investigators attributed this to atrophic gland tissue in elderly individuals. [2]
Ostmann fat pad
This fat pad is located in the inferolateral aspect of the eustachian tube and is thought to be an important contributing factor in closing the tube. It is also quite likely to contribute in the protection of the eustachian tube and the middle ear from retrograde flow of nasopharyngeal secretions.
Relations of the Eustachian Tube
Muscles
The muscles of the eustachian tube system help open and close the tube, thus allowing it to perform its function. These muscles are the (1) tensor veli palatini, (2) levator veli palatini, (3) salpingopharyngeus, and (4) tensor tympani.
The tensor veli palatini muscle originates from the bony wall of the scaphoid fossa and from the whole length of the short cartilaginous flange that forms the upper portion of the front wall of the cartilaginous tube. The muscle runs downward, converging into a short tendon that turns medially around the pterygoid hamulus. It then fans out within the soft palate and mingles with the fibers from the opposite side in the midline raphe. The tensor veli palatini separates the eustachian tube from the otic ganglion, the mandibular nerve and its branches, the chorda tympani, and the middle meningeal artery.
The salpingopharyngeus is a delicate muscle that is attached to the pharyngeal end of the eustachian tube and blends with the palatopharyngeus muscle downward.
The levator veli palatini has 2 origins: the lower surface of the cartilaginous tube and the lower surface of the petrous bone. At first, the levator is inferior to the tube; it then crosses to the medial side and merges into the soft palate.
Blood vessels
The arterial supply of the eustachian tube is derived from the ascending pharyngeal and middle meningeal arteries. The venous drainage is carried to the pharyngeal and pterygoid plexus of veins. The lymphatics drain into the retropharyngeal lymph nodes.
Ozturk et al (2012) studied the anatomical relation between the eustachian tube and petrous portion of the internal carotid artery (ICA). [3] They found that the junctional part of the eustachian tube may be a safe landmark to identify and protect the ICA. Knowledge of the anatomical relationships of the eustachian tube with other surgical and radiological landmarks is definitely useful during endoscopic endonasal procedures and cranial base surgery.
Nerves
The pharyngeal branch of the sphenopalatine ganglion derived from the maxillary nerve (V2) supplies the ostium. The nervus spinosus derived from the mandibular nerve (V3) supplies the cartilaginous part, and the tympanic plexus derived from the glossopharyngeal nerve supplies the bony portion of the eustachian tube.
Three Physiologic Functions of the Eustachian Tube
The physiologic functions of the eustachian are as follows:
-
Ventilation or pressure regulation of the middle ear
-
Protection of the middle ear from nasopharyngeal secretions and sound pressures
-
Clearance or drainage of middle ear secretions into the nasopharynx
Ventilation or pressure regulation
The normal eustachian tube at rest is collapsed, with perhaps slight negative middle ear pressure. Repeated opening of the eustachian tube actively maintains normal atmospheric pressure.
The eustachian tube opens upon swallowing or yawning by contraction of the tensor veli palatini muscle. Defective tensor veli palatini muscle function in cleft palate results in eustachian tube dysfunction. The role of the levator veli palatini muscle is unclear. Its contribution in opening the eustachian tube has been questioned.
Eustachian tube ventilatory function is less efficient in children than in adults. In addition, repeated upper respiratory tract infections and enlarged adenoids in children further contribute to the increased incidence of middle ear disease in children. However, as children grow, eustachian tube function improves as evidenced by the reduced frequency of otitis media from infancy to maturity.
Normally, the eustachian tube opens frequently, stably maintaining the middle ear pressure between +50 mm and -50 mm H2 O. However, pressures above and below this range do not necessarily indicate middle ear disease.
About 1 mL of air or gas may be absorbed from the middle ear in 24 hours. The mastoid cell system is thought to function as a gas reservoir for the middle ear.
Protection
The eustachian tube is closed at rest. Sudden loud sounds are thus dampened before reaching the middle ear through the nasopharynx.
Patulous eustachian tube is an abnormal but not uncommon condition in which the tube is abnormally patent. The patient often complains about echoing when he or she talks (autophony), as well as ear fullness. Rapid weight loss may lead to decreased size of the Ostmann fat pad, which is thought to contribute to this condition.
The eustachian tube drains normal secretions of the middle ear by the mucociliary transport system and by repeated active tubal opening and closing, which allows secretions to drain into the nasopharynx.
A derangement in the closed middle ear system, such as tympanic membrane perforation or after mastoid surgery, sometimes results in reflux of nasopharyngeal secretions into the tube and can cause otorrhea.
Similarly, forceful nose blowing creates high nasopharyngeal pressure and may force nasopharyngeal secretions into the middle ear. Laryngopharyngeal reflux (LPR) was recently implicated in the etiology of otitis media with effusion (OME). Al-Saab et al (2008) demonstrated the presence of pepsinogen in 84% of middle ear effusions (MEEs) at concentrations 1.86 to 12.5 times higher than that of serum. [4]
Conversely, a relative negative middle ear pressure, as occurs in aircraft or scuba diving descent, may lock the eustachian tube. This leads to stagnation of secretions, and effusion collects in the middle ear as otitic barotrauma evolves. Inflation of the eustachian tube by the Valsalva maneuver or by politzerization can break the negative pressure in the middle ear and clears the effusion.
The middle ear is also protected by the local immunologic defense of the respiratory epithelium of the eustachian tube, as well as its mucociliary defense (clearance). A pulmonary immunoreactive surfactant protein has been isolated from the middle ears of animals and humans. It is thought to have the same protective function in the middle ear.
Clearance or drainage
Drainage of secretions and occasional foreign material from the middle ear is achieved by the mucociliary system of the eustachian tube and the middle-ear mucosa and muscular clearance of the eustachian tube, as well as surface tension within the tube lumen.
The flask model proposed by Bluestone and his colleagues helps to better explain the role of the anatomic configuration of the eustachian tube in the protection and drainage of the middle ear. [5] In this model, the eustachian tube and middle ear system is likened to a flask with a long narrow neck. The mouth of the flask represents the nasopharyngeal end, the narrow neck represents the isthmus, and the middle ear and mastoid gas cell system represents the body of the flask.
Fluid flow through the neck depends on the pressure at either end, the radius and length of the neck, and the viscosity of the liquid. When a small amount of liquid is instilled into the mouth of the flask, the liquid flow stops somewhere in the narrow neck due to the narrow diameter of the neck and the relative positive air pressure in the chamber of the flask. However, this does not take into consideration the dynamic role of the tensor veli palatini muscle in actively opening the nasopharyngeal orifice of the eustachian tube.
Eustachian Tube Function Tests
A functional and patent eustachian tube is necessary for ideal middle ear sound mechanics. A fully patent eustachian tube may not necessarily have perfect functioning, as is the case with the patulous eustachian tube or with mucociliary abnormalities. Testing of both eustachian tube patency and function are therefore important.
Pneumatic otoscopy
Permeatal examination of the tympanic membrane assesses the patency and perhaps the function of the tube. A normal appearing tympanic membrane usually indicates a normally functioning eustachian tube, although this does not preclude the possibility of a patulous tube.
Otoscopic evidence of tympanic membrane retraction or fluid in the middle ear indicates eustachian tube dysfunction but cannot be used to differentiate between functional impairment and mechanical obstruction of the tube. Normal tympanic membrane mobility on pneumatic otoscopy (siegalization) indicates good patency of the eustachian tube.
Nasopharyngoscopy
Nasopharyngoscopy by posterior rhinoscopic mirror examination or more accurately by fiberoptic endoscope helps visualization of any mass (eg, adenoids, soft tissue growth in the nasopharynx) that may be obstructing the pharyngeal end of the eustachian tube.
Attempts have been made to assess eustachian tube function with the help of nasopharyngoscopy. Yagi and colleagues evaluated the patency of the eustachian tube using a fiberoptic endoscope and a photoelectric device (phototubometry). [6] Using videoendoscopy of the ear, Poe and colleagues assessed tubal function in adults and observed various disease processes such as inflammation of the tube and patulous dysfunction. This method has been gaining popularity in the assessment of patients suspected to have eustachian tube dysfunction.
Tympanometry
Measuring middle ear pressure with an electroacoustic impedance meter helps to assess eustachian tube function.
High negative middle ear pressure (>-100 daPa) indicates eustachian tube dysfunction. High negative pressures may be seen in individuals with normal hearing; however, a nearly normal middle ear pressure may be associated with hearing loss.
In the presence of tympanic membrane perforation, the air passes into the middle ear resulting in a large canal volume on tympanometry.
Imaging
With the recent development of advanced imaging technology, studies have been used to better define the anatomy and pathology of the eustachian tube. Magnetic resonance imaging (MRI) has been used to visualize the eustachian tube and to assess its anatomy and pathology in patients with nasopharyngeal carcinoma. Moreover, MRI has been used in experimental animal models to evaluate middle ear inflammation. It has more accurately been also used to assess the effect of experimentally induced functional obstruction of the eustachian tube by botulinum toxin A on the middle ear.
Computed tomography (CT) scanning has also been used to assess the tube in normal individuals, in patients with patulous eustachian tube, and in otitis media, and it has been used in studying eustachian tube clearance. Fluoroscopy with contrast provides dynamic evaluation of mucociliary clearance. Yoshioka et al (2013) studied the movement of the eustachian tube during sniffing in patients with patulous tube using a 320-Row Area Detector CT scanner. [7] They demonstrated various patterns of eustachian tube closure during sniffing in these patients. This method may be useful for evaluating different types of eustachian tube dysfunction.
A prospective study by Tarabichi and Najmi indicated that in most persons with healthy ears, temporal bone CT scans performed during the Valsalva maneuver can visualize the distal third of the eustachian tube lumen, suggesting that this imaging strategy could help to localize disorders in patients with symptoms of eustachian tube obstruction. The study was performed on 38 patients (76 ears), with the distal third of the lumen visualized in 71 ears (93%) and the entire lumen visualized in 27 ears (36%). [8]
However, a study by Kourtidis et al indicated that in the detection of Eustachian tube dysfunction, CT scans have low sensitivity (52.5%; specificity, 97.5%) and are therefore not an appropriate screening tool for such dysfunction in routine clinical practice. Patients in the study were aged over 16 years and had unilateral Eustachian tube dysfunction, with the Valsalva maneuver performed during temporal bone CT scanning to improve visualization of the tube’s lumen. [9]
Eustachian tube catheterization
Catheterization of the eustachian tube with a curved metal cannula via the transnasal approach has been used to assess tubal function for more than 100 years. It can be done blindly, with the help of a nasopharyngoscope, or transorally with a 90° telescope.
The catheter is passed along the floor of the nose until it touches the posterior wall of the nasopharynx. The catheter is then rotated 90° medially and pulled forward until it impinges on the posterior free part of the nasal septum. The catheter is then rotated 180° laterally, so that its tip lies at the nasopharyngeal opening of the eustachian tube. A Politzer bag is attached to the outer end of the catheter, and an auscultation tube with 2 ear tips is used with one tip in the patient's ear and the other in the examiner's ear. Air is pushed into the catheter by means of the Politzer bag. The examiner hears the rush of air as it passes through the catheter into the eustachian tube and then into the middle ear.
Successful transferring of applied positive pressure from the proximal end of the cannula into the middle ear suggests tubal patency. Normal blowing sounds mean a patent eustachian tube and bubbling indicates middle ear fluid. Whistling suggests partial eustachian tube obstruction while absence of sounds indicates complete obstruction or failed catheterization.
Valsalva and Politzer tests
In the Valsalva test, the eustachian tube and middle ear are inflated by a forced expiration with the mouth closed and the nose pinched by the thumb and forefinger. The effect of high positive nasopharyngeal pressures at the proximal end of the eustachian tube system can be evaluated qualitatively. When the tympanic membrane is intact, the overpressure in the middle ear can be observed by otoscopy as a bulging tympanic membrane. When the tympanic membrane is perforated, the sound of the air escaping from the middle ear can be heard with a stethoscope or with the Toynbee tube.
The Politzer test is similar to the Valsalva test, but instead of positive nasopharyngeal pressure being generated by the patient, the nasopharynx is passively inflated. This is achieved by compressing one nostril into which the end of a rubber tube attached to an air bag has been inserted while compressing the opposite nostril by finger pressure. The subject is asked to swallow or to elevate the soft palate by repeating the letter "k."
Both the Valsalva and Politzer tests are outdated and rarely used clinically for assessment of eustachian tube function. These maneuvers may be more beneficial in the management of some patients. Nevertheless, the efficacy of these procedures for treatment of middle ear effusion is controversial, and they are not without potential risks. The author has encountered a case of meningitis following Politzerization for the treatment of otitis media with effusion in an otherwise healthy elderly man.
Toynbee test
This test is considered more reliable than the previous 2 in the assessment of eustachian tube function. On closed nose swallowing, negative middle ear pressure develops in healthy persons. In an intact tympanic membrane, pneumatic otoscopy or tympanography can be used to measure changes in middle ear compliance. In a perforated tympanic membrane, the manometer of the impedance bridge can be used to measure middle ear pressure changes.
Other Tests of Eustachian Tube Function
Other tests have been developed for assessment of eustachian tube function. A 9-step inflation-deflation tympanometric test is used to assess changes in resting middle ear pressure after applying positive and negative ear canal pressures while the patient is swallowing.
Other methods include microflow technique, impedance method, sonometry, forced response test, and videoendoscopy of the nasopharyngeal end of the eustachian tube.
A self-described method by patients with perforated tympanic membranes is the bitter taste of ear drops in the mouth when used topically. This indicates a patent eustachian tube.
A final testing mechanism is sonotubometery. The advantage of this diagnostic test is the ability to evaluate the eustachian tube function with or without an intact tympanic membrane under physiologic conditions.
Eustachian Tube Dysfunction
A long-lasting dysfunction of the eustachian tube seems to be the cause for development of chronic otitis media (COM) with tympanic membrane perforation, otitis media with effusion (OME), and atelectasia of the middle ear. [10] Surgical interventions generally treat the sequelae of the tube dysfunction but not the dysfunction itself. Sedlmaeir et al (2009) published a study on laser ablation of the posterior half of the tubal ostium. [11] The function of the eustachian tube was optimized in 70% of the patients, particularly if pathological findings were present (tubal tonsil, narrow orifice of the tubal ostium, adenoids).
To study the safety and efficacy of balloon dilation of the eustachian tube, Poe et al published a pilot clinical trial in 2011. They concluded that dilation of the cartilaginous eustachian tube appeared to be beneficial and without significant adverse effects in the treatment of patients with longstanding OME who were unable to autoinsufflate their eustachian tube by Valsalva, swallow, or yawn. [12]
A study by Tisch et al reported that following balloon dilation therapy, more than 80% of children with refractory chronic obstructive eustachian tube dysfunction experienced clinical symptom improvement. [13]
A retrospective study by Satmis and van der Torn found that transnasal balloon dilation may be useful in treating adults with chronic dilatory eustachian tube dysfunction, at least in the short-term. The study patients’ Eustachian Tube Dysfunction Questionnaire (ETDQ-7) score showed significant improvement at 1- and 3-month postoperative follow-up. The air-bone gap also significantly improved postoperatively. Subjective satisfaction at the two follow-up points was about 43% and 48%, respectively. [14]
A literature review by Mehta et al found that single-agent intranasal corticosteroid treatment produced symptomatic improvement in just 11-18% of patients with chronic eustachian tube dysfunction. However, one study found that symptoms resolved in 50% of chronic patients treated with a combination of intranasal corticosteroid and the Buteyko breathing technique. [15]
Kanemaru et al (2012) studied the change in function of the eustachian tube using tissue-engineered regeneration of mastoid air cells (MACs). [16] They observed that tissue-engineered regeneration of MACs improved eustachian tube function and gas exchange in the middle ear.
Using transnasal videoendoscopy in 33 adults, Alper et al found evidence that during swallowing, elevation of the soft palate (which is associated with rotation of the medial lamina and widening of the eustachian tube orifice) is decreased in persons with a healthy middle ear but with a history of middle ear disease, compared with persons with a healthy middle ear and no history of middle ear disease, perhaps indicating that such individuals have reduced eustachian tube function and a greater risk for otitis media. [17]
-
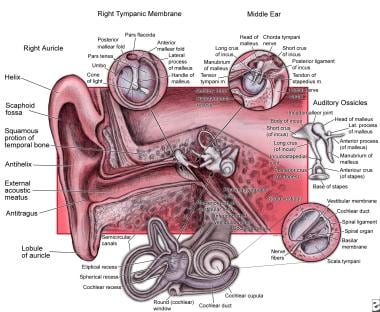
Anatomy of the ear.