Background
Tracheostomy is an operative procedure that creates a surgical airway in the cervical trachea. [1, 2] It is most often performed in patients who have had difficulty weaning off a ventilator, followed by those who have suffered trauma or a catastrophic neurologic insult. [3] Infectious and neoplastic processes are less common in diseases that require a surgical airway.
Tracheostomy is a utilitarian surgical procedure of access; therefore, it should be discussed in light of the problem it addresses: access to the tracheobronchial tree. The trachea is a conduit between the upper airway and the lungs that delivers moist warm air and expels carbon dioxide and sputum. Failure or blockage at any point along that conduit can be most readily corrected with the provision of access for mechanical ventilators and suction equipment. In the case of upper airway obstruction, tracheostomy provides a path of low resistance for air exchange.
The traditional semantic difference between tracheostomy and tracheotomy is now blurred because the hole is variably permanent. If a cannula is in place, an unsutured opening heals into a patent stoma within a week. If decannulation is performed (ie, the tracheostomy cannula is removed), the hole usually closes in a similar amount of time. The cut edges of the tracheal opening can be sutured to the skin with a few absorbable sutures to facilitate cannulation and, if necessary, recannulation can be performed. Alternatively, a permanent stoma can be created with circumferential sutures. The term tracheostomy is used, by convention, for all these procedures and is considered to be synonymous with tracheotomy.
The trachea is nearly but not quite cylindrical but is flattened posteriorly. In cross-section, it is D-shaped, with incomplete cartilaginous rings anteriorly and laterally, and a straight membranous wall posteriorly. The trachea measures about 11 cm in length and is chondromembranous. This structure starts from the inferior part of the larynx (cricoid cartilage) in the neck, opposite the 6th cervical vertebra, to the intervertebral disc between T4-5 vertebrae in the thorax, where it divides at the carina into the right and left main stem bronchi. For more information about the relevant anatomy, see Trachea Anatomy.
Indications
The advent of the antibiotic era and advances in anesthesia have made tracheostomy a commonly performed elective procedure. Important to note, however, is that there are situations when tracheostomy is quite urgent or emergent. This typically involves patient who is immediate need of a surgical airway because of impending airway obstruction.
General indications include the following:
-
Congenital anomaly (eg, laryngeal hypoplasia, vascular web)
-
Upper airway foreign body that cannot be dislodged with Heimlich and basic cardiac life support maneuvers
-
Supraglottic or glottic pathologic condition (eg, infection, neoplasm, bilateral vocal cord paralysis)
-
Neck trauma that results in severe injury to the thyroid or cricoid cartilages, hyoid bone, or great vessels
-
Subcutaneous emphysema
-
Facial fractures that may lead to upper airway obstruction (eg, comminuted fractures of the mid face and mandible)
-
Upper airway edema from trauma, burns, infection, or anaphylaxis
-
Prophylaxis (as in preparation for extensive head and neck procedures and the convalescent period)
-
Severe sleep apnea not amendable to continuous positive airway pressure devices or other less invasive surgery
Tracheostomy may also be performed to provide a long-term route for mechanical ventilation in cases of respiratory failure or to provide pulmonary toilet in the following cases:
-
Inadequate cough due to chronic pain or weakness
-
Aspiration and the inability to handle secretions
The cuffed tube allows the trachea to be sealed off from the esophagus and its refluxing contents. Thus, this intervention can prevent aspiration and provide for the removal of any aspirated substances. However, some investigators argue that the risk of aspiration is not actually lessened, as secretions can leak around the cuffed tube and reach the lower airway.
The Council on Critical Care of the American College of Chest Physicians recommends tracheostomy in patients who are expected to require mechanical ventilation for longer than 7 days. [4] However, the final decision is made on an individual basis based on comorbidities and the patient’s current condition.
A retrospective population-based study from Taiwan compared the long-term mortality between patients on prolonged mechanical ventilation with tracheostomy with those without tracheostomy and found no differences in long-term mortality between the two groups. [5]
It is also important to outline what tracheostomy does not or will not do for the patient. Specifically, tracheostomy does not prevent aspiration of airway or other secretions.
Additional diagnoses for which tracheostomy is often considered early in the course include botulism, amyotrophic lateral sclerosis, and cervical spine injury, among others.
Contraindications
No absolute contraindications exist for tracheostomy. A strong relative contraindication to discrete surgical access to the airway is the anticipation that the blockage is a laryngeal carcinoma. The definitive procedure (usually a laryngectomy) is planned, and prior manipulation of the tumor is avoided because it may lead to increased incidence of stomal recurrence. Temporary tracheostomy may be performed just under the first tracheal ring in anticipation of a laryngectomy at a later time.
End-of-life issues may also come to bear on the decision to perform a tracheostomy because it may represent further mechanization of the patient's care to family members. In fact, the performance of a tracheostomy does not affect the decision to extend or to withdraw care. Hygiene is improved, quality of life (speaking and eating, if relevant) is improved, and placement in long-term care is facilitated in some cases; however, dependence on mechanical ventilation may not be changed.
Technical Considerations
Procedure planning
Tracheostomies can be performed through with an open or percutaneous technique. Open tracheostomy is one of the oldest procedures described in the literature and is still the procedure of choice for some trauma centers. However, the use of percutaneous tracheostomy has been increasing since its introduction in the 1980s.
Studies have supported percutaneous over open tracheostomies. However, the final technique depends on the surgeon’s experience and comfort, in addition to guidelines of the facility where this procedure is to be performed.
Patient selection - Percutaneous versus open tracheostomy
In 1969, Toy and Weinstein described a technique of tracheostomy performed percutaneously at the bedside using essentially a Seldinger technique modified with progressive dilation. [6]
Its main advantage is that it can be performed at the bedside; therefore, the expense and logistics of transportation and operating room usage are eliminated. These advantages are mitigated because bedside anesthesia is required and bronchoscopic visualization adds to the expense and personnel required. Moreover, preparation for the possibility of an emergent open tracheostomy is important.
Its disadvantages stem from the decreased exposure and thus decreased visualization and control. A study of 149 critically ill patients found a greater risk of severe (>50%) suprastomal stenosis developing as a late complication of percutaneous dilational tracheostomy versus surgical tracheostomy. [7]
The following patients are commonly recognized to be unfavorable candidates:
-
Patients with obesity
-
Patients with abnormal or poorly palpable midline neck anatomy
-
Patients who need emergency airways
-
Patients with coagulopathy
-
Pediatric patients
-
Patients with enlarged thyroids
Kost reported on the use of this procedure in 500 consecutive intubated adults in the intensive care unit. [8] When this procedure was performed in conjunction with bronchoscopy, the complication rate was acceptably low (9.2%). No serious complications (eg, pneumothorax, pneumomediastinum, death) occurred. The most common complications were oxygen desaturation in 14 patients (defined as a drop, even transient, to less than 90%) and bleeding in 12 patients (when intervention was required to control the bleeding).
Complication prevention
Potential complications are due to direct injury. Bedside ultrasound is often used to survey the tracheostomy site during the planning stage, especially for percutaneous tracheostomies. This is to identify vessels that may be under the intended incision and to help avoid injury.
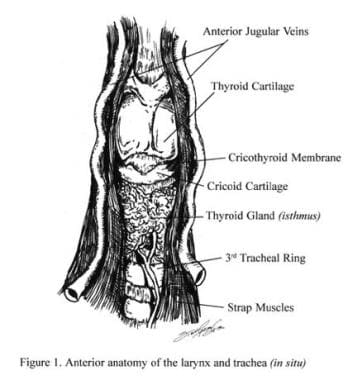
The cricothyroid muscle, vocal muscles, and the vocal cords are vulnerable to injury during tracheostomy (see the image below).
The innominate artery, or brachiocephalic trunk, crosses from left to right anterior to the trachea at the superior thoracic inlet and lies just beneath the sternum. The trachea is membranous posteriorly and is formed of semicircular cartilaginous rings anteriorly and laterally. The spaces between the rings are membranous.
The recurrent laryngeal nerves and inferior thyroid veins that travel in the tracheoesophageal groove are paratracheal structures vulnerable to injury if dissection strays from the midline (see the image below). The recurrent laryngeal nerve is also vulnerable to injury from the cuff of the tracheostomy tube, particularly if the cuff is overinflated.
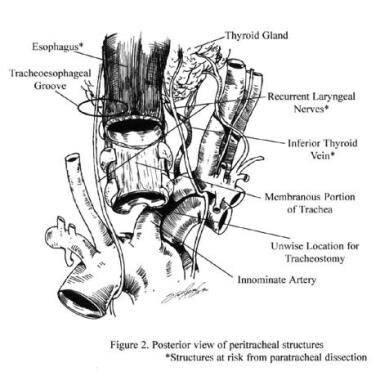 Posterior view of paratracheal structures. The asterisk indicates structures at risk from paratracheal dissection.
Posterior view of paratracheal structures. The asterisk indicates structures at risk from paratracheal dissection.
The great vessels (ie, carotid arteries, internal jugular veins) could be damaged should dissection go far afield, which is a real risk in pediatric or obese patients. The thyroid gland lies anteriorly to the trachea with a lobe on both sides and the isthmus, which crosses the trachea at approximately the level of the second and third tracheal rings. This tissue is extremely vascular and must be divided with careful hemostasis.
-
Anterior anatomy of the larynx and trachea (in situ).
-
Posterior view of paratracheal structures. The asterisk indicates structures at risk from paratracheal dissection.
-
Parasagittal view through larynx. The asterisk indicates structures at risk during cricothyrotomy.
-
Operative view of tracheostomy. The thyroid isthmus is divided with electrocautery.
-
Operative view of tracheostomy. These are options for tracheal incision.
-
Operative view of tracheostomy. These are special techniques in the patient with obesity.
-
This video demonstrates the results of rigid direct laryngoscopy and flexible tracheal endoscopy in a patient with significant tracheal stenosis.
-
This video demonstrates the 90-degree endoscopic view in 2 patients with tracheal stenosis.
-
This video of a 90-degree endoscopic tracheal view was obtained from a patient with postintubation tracheal stenosis.
-
This video demonstrates the 90-degree endoscopic view in 2 patients with tracheal stenosis.
-
Surgical technique for a tracheostomy. Video courtesy of Ravindhra G Elluru, MD, PhD.
-
Percutaneous Tracheostomy. Video courtesy of Yassir Adbulrahman, MD, Ashok Parchani, MD, and Ruben Peralta, MD, FACS, FCCM, FCCP, Hamad Medical Corporation.
-
Surgical cricothyroidotomy Seldinger. Video courtesy of Therese Canares, MD, and Jonathan Valente, MD, Rhode Island Hospital, Brown University.
-
Uncuffed (A) and cuffed (B) single-cannula tubes.
-
Double-cannula tube shown with choice of fenestrated and nonfenestrated inner cannulae. Obturator for insertion is also included at the bottom.
-
Inner cannulae shown with and without 15-mm connector, fenestrated and nonfenestrated designs.
-
Cuffed tube with pilot balloon.
-
Fenestrated cuffed and uncuffed tubes.
-
Adult swivel, neonatal, and pediatric neck flanges.
-
Bivona and Portex adjustable-neck-flange tubes.
-
Decannulation cap (top). Decannulation caps attached to inner cannulae of cuffed and uncuffed tubes.
-
Single-cannula tube made of silver with speaking valve.