Overview
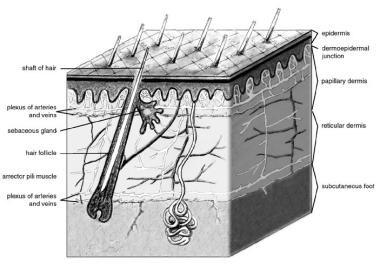
Wound closure techniques have evolved from the earliest development of suturing materials to comprise resources that include synthetic sutures, absorbables, staples, tapes, and adhesive compounds. The engineering of sutures in synthetic material along with standardization of traditional materials (eg, catgut, silk) has made for superior aesthetic results. Similarly, the creation of topical skin adhesives (the monomer 2-octyl cyanoacrylate), surgical staples, and tapes to substitute for sutures has supplemented the armamentarium of wound closure techniques. Aesthetic closure of a wound, whether traumatic or surgically induced, is based on knowledge of healing mechanisms and skin anatomy (see the image below), as well as an appreciation of suture material and closure technique. Choosing the proper materials and wound closure technique ensures optimal healing. [1]
Four phases of wound healing have been identified and studied on the cellular and molecular level. As the field of molecular biology and genetics continues to broaden, the understanding of how wounds heal continues to improve dramatically. These four distinct phases are (1) hemostasis, (2) inflammatory phase, (3) proliferative ("rebuilding") phase, and (4) maturation phase. By understanding the phases of wound healing, the provider becomes more knowledgeable about the initial and subsequent care of wounds as well as how better to care for poorly healing wounds.
The initial injury leads to blood vessel disruption. Assuming normal thrombotic ability (ie, the patient is not taking medications that inhibit the clotting cascade, or has a preexisting genetic coagulopathy), once the collagen lining the vessels is exposed to blood, hemostasis ensues. This step involves the very complex intrinsic and extrinsic coagulation pathways (discussed elsewhere). Clot formation occurs in minutes. Chemoattractants released by cells within the clot and injured vessel cause neutrophils and macrophages to be drawn to the site of injury. The inflammatory response in the wound happens within minutes to hours of development of the wound, and, as with all of the phases of wound healing, this phase overlaps with the next phase. Migration of epithelial cells has been shown to occur within the first 12-24 hours, but further new tissue formation occurs over the next 10-14 days.
The importance of the inflammatory cells (neutrophils and macrophages) and the local tissue mediators cannot be overstated. In order to preserve these cells and mediators, a wound should be minimally manipulated. Vigorous scrubbing and/or the use of cytotoxic fluids to irrigate a wound can impair and lengthen healing time. Products such as sodium hypochlorite (bleach, diluted or otherwise), hydrogen peroxide, betadine, and alcohol should not be placed directly into a wound. These are all cytotoxic and will destroy inflammatory cells. Simple wound care with sterile water or saline should be used. If necessary, a syringe and intravenous catheter can be used to pressure wash contaminants from dirty wounds.
Epithelialization and neovascularization (occurring within the overlap of proliferation and maturation phases) result from the increase in cellular activity. Stromal elements in the form of extracellular matrix materials are secreted and organized. This new tissue, called granulation tissue, depends on specific growth factors for further organization to occur in the completion of the healing process. This physiologic process occurs over several weeks to months in a healthy individual.
Finally, tissue remodeling, in which wound contraction and tensile strength is achieved, occurs in the next 6-12 months. Systemic illness and local factors can affect wound healing. Traditionally, two types of wound healing have been described—primary intention and secondary intention.
In the primary intention method, surgical wound closure facilitates the biological event of healing by joining the wound edges. Surgical wound closure directly apposes the tissue layers, which serves to minimize new tissue formation within the wound. However, remodeling of the wound does occur, and tensile strength is achieved between the newly apposed edges. Closure can serve both functional and aesthetic purposes. These purposes include elimination of dead space by approximating the subcutaneous tissues, minimization of scar formation by careful epidermal and dermal alignment, and avoidance of a depressed scar by precise eversion of skin edges. If dead space is limited with opposed wound edges, then new tissue has limited room for growth. Correspondingly, atraumatic handling of tissues combined with avoidance of tight closures and undue tension contribute to a better result.
The secondary intention method (spontaneous healing) is ancient and well established. It can be used in lieu of complicated reconstruction for certain surgical defects. This method also depends on the four stages of wound healing to achieve the ultimate result.
Indications
Many wounds heal best with surgical closure. However, as noted in Contraindications, some wounds should be left open and allowed to either heal by secondary intention or by delayed primary intention.
Contraindications
Certain concave surfaces of the face may heal best by healing by secondary intention. Examples of such surfaces include the nasal alar crease, the temple, the preauricular sulcus, and the conchal bowl.
When there is tissue loss, as in an avulsion injury, wound closure may be delayed to allow for control of locally necrotic tissue and environmental dirt/debris.
Immediate closure of human bites and certain animal bites may induce wound infections, so delayed closure may be indicated.
Anesthesia
Lidocaine 1% with 1:100,000 epinephrine is most commonly used and probably most preferred. One part sodium bicarbonate to 10 parts local anesthesia with epinephrine may be added into premixed bottles of lidocaine with epinephrine to lessen the local burning during infiltration when the procedure is performed under local anesthesia (without the use of general anesthesia).
Bupivacaine, 0.25% or 0.5%, with or without epinephrine is a long-lasting local anesthetic that may be used for procedures of longer duration, where a longer half-life is desired.
The addition of epinephrine into the local anesthetic serves two main functions. First, the local vasoconstriction afforded by the epinephrine helps keep the anesthetic at the wound site longer, allowing for a protracted anesthetic effect. Second, the vasoconstriction improves hemostasis by the effect of the epinephrine on the surrounding blood vessels. An added benefit of the epinephrine is that the delay in absorption of the anesthetic (lower plasma levels) allows for a higher dose to be used if needed to achieve complete anesthesia or to lengthen the procedural time needed to close the wound.
However, there are several body sites where the use of epinephrine in the anesthetic solution should be avoided; these include the ears, tip of the nose, distal phalanges, and the penis. Because of the sometimes tenuous blood supply to these areas, the vasoconstrictive effect of the epinephrine may cause local tissue necrosis, owing to profound, local tissue ischemia. In these cases, the anesthetic should be of the plain variety.
It is imperative that the provider know the correct dosing for any anesthetic used. For this, one must know the approximate weight, in kilograms, of the patient. Additionally, the provider must know the concentration of the anesthetic in the supplied vial to correctly calculate the volume and milligram dose that can be administered to a given patient.
Toxicity from local anesthetics can result in seizures. Both CNS and cardiovascular toxicity can be fatal. Inadvertent intravascular administration of bupivacaine may cause significant cardiac effects. Bupivacaine is the longest-lasting local anesthetic used commonly in the United States.
Dosing of lidocaine and bupivacaine (assuming normal hepatic and renal function) is as follows:
-
Lidocaine without epinephrine (ie, plain lidocaine or "lidocaine without"): 4.5 mg/kg
-
Lidocaine with epinephrine (ie, "lidocaine with"): 7 mg/kg
-
Bupivacaine with or without epinephrine (adults only): 175 mg single dose or maximum of 400 mg per 24 hours
Also see Local and Regional Anesthesia.
Equipment
History
The history of sutures begins more than 2,000 years ago with the first records of eyed needles. A plastic surgeon from India, Susruta (CE c380-c450), described suture material made from flax, hemp, and hair. At that time, the jaws of the black ant were used as surgical clips in bowel surgery. In 30 CE, the Roman Celsus again described the use of sutures and clips, and Galen further described the use of silk and catgut in 150 CE. Before the end of the first millennium, Avicenna described monofilament with his use of pig bristles in infected wounds. Surgical and suture technique evolved in the late 1800s with the development of sterilization procedures. Finally, modern methods created uniformly sized sutures. [4]
Catgut and silk are natural materials that were the mainstay of suturing products, and they remain in use today. The first synthetics were developed in the 1950s, and further advancements have led to the creation of various forms. The different types of sutures offer different qualities in terms of handling, knot security, and strength for different purposes. No single suture offers all of the ideal characteristics that one would wish for. Often the trade-off is in tissue handling versus longevity versus healing properties.
Sutures
General classification of sutures includes natural and synthetic, absorbable and nonabsorbable, and monofilament and multifilament (ie, braided). Natural materials are more traditional and are still used in suturing today. Synthetic materials cause less reaction, and the resultant inflammatory reaction around the suture material is minimized. [5]
Absorbable sutures are applicable to a wound that heals quickly and needs minimal temporary support. Their purpose is to alleviate tension on wound edges. The newer synthetic absorbable sutures retain their strength until the absorption process starts. Nonabsorbable sutures offer longer mechanical support.
Monofilaments have less drag through the tissues but are susceptible to instrumentation damage. Infection is less likely with the monofilament, unlike the braided multifilament, which can potentially sustain bacterial inocula. Natural materials include gut, silk, and even cotton. Gut is absorbable, but cotton and silk are not. Gut is considered a monofilament, whereas silk and cotton are braided multifilaments. Gut, silk, and cotton have very limited use in routine wound care. These are used more commonly in the surgical suite when operating on the GI tract. One exception to this is the use of gut when closing intraoral wounds.
Various synthetic materials are available for suturing. The absorbable sutures include the monofilamentous Monocryl (poliglecaprone), Maxon (polyglycolide-trimethylene carbonate), and PDS (polydioxanone). Braided absorbable sutures include Vicryl (polyglactin) and Dexon (polyglycolic acid). Nonabsorbable sutures comprise nylon, Prolene (polypropylene), Novafil (polybutester), PTFE (polytetrafluoroethylene), steel, and polyester. Nylon and steel sutures can be monofilaments or multifilaments. Prolene, Novafil, and PTFE are monofilaments. Polyester suture is braided.
Absorbable suture materials lose their tensile strength before complete absorption. Gut can last 4-5 days in terms of tensile strength. In the chromic form (ie, treated in chromic acid salts), gut can last up to 3 weeks. Vicryl and Dexon maintain tensile strength for 7-14 days, although complete absorption takes several months. Maxon and PDS are considered long-term absorbable sutures, lasting several weeks and likewise requiring several months for complete absorption.
Nonabsorbable sutures have varying tensile strengths and may be subject to some degree of degradation. Silk has the lowest strength and nylon has the highest, although Prolene is comparable. Both nylon and Prolene require extra throws to secure knots in place, owing to the "memory" of the monofilament. Polyester has a high degree of tensile strength, and Novafil is appreciated for its elastic properties.
New to the market, within the past few years, are sutures that are either impregnated or coated with antimicrobials. Their role in routine wound care has not yet been established. These products increase the cost of wound care without significant benefit. A robust meta-analysis published in 2017 found no evidence to support routine use of these sutures. [6] Indeed, most surgeons would agree that proper wound handling, sterile technique, and after care are the most important aspects when it comes to prevention of wound infection.
Use of topical skin adhesives can simplify skin closure in that certain problems inherent to suture use can be avoided. Problems (eg, reactivity, premature reabsorption) can occur with sutures and lead to an undesirable result, both cosmetically and functionally. Several adhesives have been developed to alleviate this problem and to facilitate wound closure. One substance, cyanoacrylate, has been used for 25 years and easily forms a strong flexible bond. In some forms, it can induce a substantial inflammatory reaction if implanted subcutaneously. If used superficially on the epidermal surface, few problems with inflammation occur. In a study on the use of adhesives in the emergency department, adhesives were more likely to be used in facial lacerations and in children and less likely to be used in longer wounds. [10] The concomitant use of either a topical anesthetic or no anesthetic, as opposed to an injectable, was cited as an advantage in the use of adhesives. [10]
Octyl-2-cyanoacrylate (Dermabond, Ethicon, Somerville, NJ) is the only cyanoacrylate tissue adhesive approved by the U.S. Food and Drug Administration (FDA) for superficial skin closure. Octyl-2-cyanoacrylate should only be used for superficial skin closure and should not be implanted subcutaneously. Subcutaneous sutures are used to take the tension off the skin edges prior to applying the octyl-2-cyanoacrylate. Subcutaneous suture placement aids in everting the skin edges and minimizing the chances of deposition of cyanoacrylate into the subcutaneous tissues.
In addition to its surgical adhesive indication, the FDA granted approval in January 2001 for Dermabond to be used as a barrier against common bacterial microbes including certain staphylococci, pseudomonads, and Escherichia coli.
Fibrin-based tissue adhesives can be created from autologous sources or pooled blood. They are typically used for hemostasis and can seal tissues. Although they do not have adequate tensile strength to close skin, fibrin tissue adhesives can be used to fixate skin grafts or seal cerebrospinal fluid leaks. Commercial preparations such as Tisseel (Baxter) and Hemaseel (Haemacure) are FDA-approved fibrin tissue adhesives made from pooled blood sources. These fibrin tissue adhesives are relatively strong and can be used to fixate tissues. Autologous forms of fibrin tissue adhesives can be made from patient's plasma. The concentration of fibrinogen in the autologous preparations is less than the pooled forms; therefore, these forms have a lower tensile strength.
Other materials
Staples provide a fast method for wound closure and have been associated with decreased wound infection rates. Staples are composed of stainless steel, which has been shown to be less reactive than traditional suturing material. The act of stapling requires minimal skin penetration, and, thus, fewer microorganisms are carried into the deeper skin layers. However, staples are more expensive than traditional sutures and also require great care in placement, especially in ensuring the eversion of wound edges. With proper placement though, resultant scar formation is cosmetically equivalent to that of other techniques.
Closure using adhesive tapes or strips was first described in France in the 1500s, when Pare devised strips of sticking plaster that were sewn together for facial wounds. This method allowed the wound edges to be joined and splinted. The porous paper tapes (eg, Steri-Strips) in use today are reminiscent of these earlier splints and are used to ensure proper wound apposition and to provide additional suture reinforcement. These tapes can be used either with sutures or alone. Often, skin adhesives (eg, Mastisol, tincture of Benzoin) aid in tape adherence.
Newer products such as the ClozeX (Wellesley, Mass) adhesive strip allows for rapid and effective wound closure that results in adequate cosmesis. [11] Additionally, wound closure with adhesive strips can be significantly cheaper than suturing or using a tissue adhesive. However, adhesive strips are not appropriate for many types of lacerations.
Technique
Closure by secondary intention [12]
Closure by secondary intention is a viable alternative to other wound closure techniques, especially on concave areas of the head and neck and in wounds prone to infection (human and animal bites and grossly contaminated wounds that cannot be adequately cleansed). The results achieved are aesthetic and functional and can spare the patient more complex procedures such as flap or skin graft reconstruction.
Concave surfaces, such as those presented by the auricle, occiput, medial canthus, nasal alar crease, nasolabial fold, and temple, heal well by secondary intention with minimal scarring. This approach is useful, especially in defects (either superficial or deep) resulting from dermatological surgery. The final scar is less noticeable in older patients with skin laxity and in lighter-skinned patients. This method is appropriate in conjunction with other reconstructive techniques.
Basics of wound closure
Good approximation of wound edges is paramount to proper wound closure technique. This may entail the placement of deep sutures subcutaneously or in the deepest layer of disrupted tissue; however, in some situations, a single-layer closure is adequate. When placing deep sutures, absorbables (eg, gut, Dexon, Vicryl, Monocryl) are typically used. The knot is buried. All deep sutures serve to eliminate the dead space and relieve tension from the wound surface. Deep sutures also ensure proper alignment of the wound edges and contribute to their final eversion.
Before placement of the sutures, wound closure may require sharp undermining of the tissues to minimize tension on the wound. Accomplish this maneuver by scalpel or scissors in the subdermal plane. Additionally, achieve hemostasis prior to wound closure to avoid future complications such as hematoma. Use atraumatic skin-handling technique with instruments such as skin hooks and small forceps. Typically, a cutting needle is the needle of choice. Various curvatures are available depending on tissue depth.
For wound closure in the head and neck region, small 5-0 or 6-0 sutures of nonabsorbable Prolene, nylon, or absorbable catgut are appropriate. Take great care to avoid tension during closure. Likewise, avoid strangulation with the suture at the superficial skin level. Take the greatest care to ensure that wound edges are not only aligned but are also everted. Eversion of all skin edges avoids unnecessary depression of the resultant scar. With simple sutures, place knots away from the opposed edges of the wound. Normally, remove nonabsorbable suture after 4-5 days. In certain situations, nonabsorbables can be removed at 10-12 days. Short-duration nonabsorbable sutures, especially in the face, are sufficient since the skin in these areas is very well vascularized and heals relatively quickly. Further, a shorter time span should diminish the scarring effect of sutures left in longer (ie, “railroad tracks"). However, in areas of higher skin tension or mobility, sutures should be left in longer to allow increased wound strength prior to removal of the sutures.
Suturing techniques
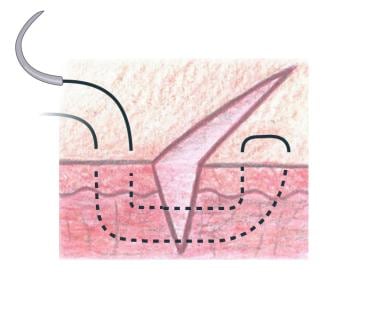
Simple suture or everting interrupted suture procedure (see the image below)
Insert the needle at a 90° angle to the skin within 1-2 mm of the wound edge and in the superficial layer. The needle should exit through the opposite side equidistant to the wound edge and directly opposite the initial insertion. For wounds of wider diameter, larger "bites" to each side may be required to allow sufficient suture tension, bring together the edges, and not compromise capillary blood flow at the sites of maximal tissue tension.
Oppose equal amounts of tissue on each side.
A surgeon's knot helps place the nonabsorbable suture because this affords a relatively higher degree of friction, thus holding the first knot until an additional knot can be placed.
Strive to evert the edges and avoid tension on the skin, while approximating the wound edges. Place all knots on the same side.
A good technique for equidistant suture placement is to place the first suture at the half-way point of the wound. Then, place additional sutures in between the first suture and the ends of the wound. Minimal gaps should be seen; however, one should strive to use as few sutures as possible to mitigate the inflammatory effects of the suture material.
Two good rules about suture placement should be remembered. (1) Approximate, do not strangulate; that is, the wound edges need only to touch to begin proper primary healing. Sutures placed too tightly may compromise blood flow and result in local tissue necrosis, worse scarring, and a less-than-appealing cosmetic effect. (2) Sutures placed and tied tightly today will be tighter tomorrow. Regardless of how much care is taken in handling tissue and placing sutures, wound edema is ubiquitous. The wound edges will swell and the tension at the site of the suture(s) will increase.
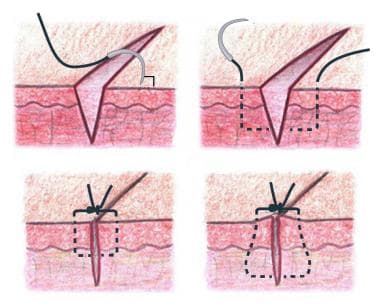 Simple interrupted suture placement. Bottom right image shows a flask-shaped stitch, which maximizes eversion.
Simple interrupted suture placement. Bottom right image shows a flask-shaped stitch, which maximizes eversion.
Simple running suture procedure
This suture method entails similar technique to the simple suture without a knotted completion after each throw. Precision penetration and tissue opposition is required.
The speed of this technique is its hallmark; however, it is associated with excess tension and strangulation at the suture line if too tight, which leads to compromised blood flow to the skin edges.
Another variant is the simple locked running suture, which has the same advantages and similar risks. The locked variant allows for greater accuracy in skin alignment, and, in some wounds, it can help with hemostasis. This can be particularly beneficial in patients who are on anticoagulation therapy and cannot be taken off these medications for simple surgical procedures.
Both styles are easy to remove. Additionally, the running sutures are more watertight.
Mattress suture procedure
Vertical mattress sutures can aid in everting the skin edges. Use this technique also for attachments to a fascial layer. The needle penetrates at 90° to the skin surface near the wound edge and can be placed in deeper layers, either through the dermal or subdermal layers. Exit the needle through the opposite wound edge at the same level, and then turn it to repenetrate that same edge but at a greater distance from the wound edge. The final exit is through the opposing skin edge, again at a greater distance from the wound edge than the original needle entrance site. Place the knot at the surface. A knot placed under tension risks a stitch mark. See the image below.
The horizontal mattress can be used to oppose skin of different thickness. With this stitch, the entrance and exit sites for the needle are at the same distance from the wound edge. Half-buried mattress sutures are useful at corners. On one side, an intradermal component exists, in which the surface is not penetrated. Place the knot at the skin surface on the opposing edge of the wound.
Subcuticular suture procedure
Sutures can be placed intradermally in either a simple or running fashion.
Place the needle horizontally in the dermis, 1-2 mm from the wound edge. Do not pass the needle through the skin surface.
The knot is buried in the simple suture, and the technique allows for minimization of tension on the wound edge.
In a continuous subcuticular stitch, the suture ends can be taped to the skin surface without knotting. [13]
Complications
Both immediate and delayed complications may occur with wound closure.
Immediate complications include the formation of hematoma secondary to improper hemostasis technique and the development of a wound infection. Antibiotics have a limited role in protecting against wound infection in traumatic wounds. These wounds are best managed with thorough lavage, debridement of devitalized tissue, and meticulous hemostasis prior to closure. Human bites and some animal bites (especially feline) are at significant risk for early infection. In these cases, antibiotics are imperative with or without primary closure. If closure is considered, wound decontamination must be as thorough as possible.
Late complications include scar formation, which may be due to either improper suturing with excess tension or lack of eversion of the edges. Additionally, hypertrophic scarring and keloid formation are unfortunate later complications of wound closure in some individuals. Other complications include stitch marks and wound necrosis.
Use of Antibiotics in Routine Wound Care
As resistance to antibiotics continues to rise in both the outpatient and the inpatient setting, a quick note regarding the use of antibiotics in routine wound care is appropriate.
As with any injury or disease process, there will be exceptions to this rule. However, it can otherwise be stated, with confidence, that antibiotic use in basic, routine wound care is unnecessary, exceptionally costly, and increases the rates of resistance. With proper wound care (adequate lavage, debridement of devitalized tissue, proper wound handling, dressing, and follow-up care), infectious complications should be an uncommon occurrence.
-
Anatomy of the skin.
-
Simple interrupted suture placement. Bottom right image shows a flask-shaped stitch, which maximizes eversion.
-
Closed chin laceration.
-
New chin laceration.
-
Fresh finger laceration.
-
Healed finger laceration.
-
Far-near near-far modification of vertical mattress suture, creating pulley effect.