Surgical Overview
In adults, the maxillary sinuses are most commonly affected with acute and chronic sinusitis. Most of these cases can be managed with medications alone. When medical management fails, surgery may be needed to treat chronic maxillary sinusitis. Pertinent sinus anatomy is seen in the image below.
 Endoscopic view right nasal cavity; lacrimal bone (L), uncinate process (U), ethmoid bulla (B), middle turbinate (MT), nasal septum (S).
Endoscopic view right nasal cavity; lacrimal bone (L), uncinate process (U), ethmoid bulla (B), middle turbinate (MT), nasal septum (S).
History of surgical therapy for chronic maxillary sinusitis
Open approaches to the maxillary sinus were first described in the early 1700s. The well-known Caldwell-Luc operation was first described in the United States by George Walter Caldwell in 1893 and then by Henri Luc of France in 1897. Subsequent advances in the understanding of the physiologic drainage pattern of the maxillary sinus led to intranasal middle meatus antrostomy in the late 1960s and the early 1970s.
Functional endoscopic sinus surgery (FESS) is based on the surgical approach performed by Messerklinger and Wigand in Europe via the ostiomeatal complex. [1, 2] FESS has become the standard surgical treatment for chronic maxillary sinusitis, with external approaches being used as an adjunct in more complicated cases or in tumor management.
Go to Functional Endoscopic Sinus Surgery for more complete information on this topic.
Indications for Surgery
Surgery for chronic sinusitis is reserved for patients who have not responded to medical therapy. Medical treatment should include 3-6 weeks of antibiotics, nasal steroids, and nasal saline irrigations.
Contraindications for surgery
No absolute contraindications to endoscopic surgical treatment of chronic maxillary sinusitis exist.
Confirmatory CT Scans
Computed tomography (CT) scanning should be obtained to confirm clinical suspicion of chronic sinusitis. Findings may include significant mucosal thickening, air-fluid levels, ostiomeatal complex obstruction, polyposis, or calcification suggestive of fungal sinusitis.
A thorough review of preoperative CT scanning is required to check for the following:
-
Position of the lamina papyracea in relation to the uncinate process
-
Position of the skull base and the nasolacrimal duct
-
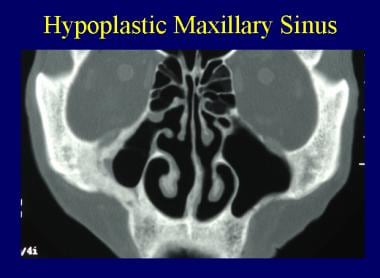
Presence of a hypoplastic maxillary sinus with or without an atelectatic uncinate process (see image below)
-
Dehiscence of the lamina papyracea or the skull base
A study by Joshua et al suggested that the severity of chronic maxillary sinusitis can be determined by CT-scan evaluation of sinus wall thickness. The study, which included 38 patients with unilateral chronic maxillary sinusitis, found that the degree of inflammation corresponded to wall thickness, although not to wall density. [3]
Anatomy of the Maxillary Sinus
Embryology
The maxillary sinus is present at birth, undergoing further expansion with age. The sinus undergoes 2 main periods of rapid growth, from birth until age 3 years and from age 7 years through early adolescence; it then continues to grow slowly until it reaches adult size by age 18 years. Later in adult life, the sinus continues to pneumatize inferiorly and may expand to contain tooth roots. The average size of the maxillary sinus is 34 mm ´ 33 mm ´ 23 mm, with an average volume of 14.75 mL. In an adult, the floor of the maxillary sinus is below the level of the nasal floor.
Anatomy of the lateral nasal wall
An understanding of the lateral nasal wall anatomy is critical to performing safe and effective endoscopic sinus surgery.
The maxillary sinus is housed in the body of the maxilla, with the inferior orbital wall as the superior border, the lateral nasal wall as the medial boundary, the alveolar process of the maxilla as its inferior border, and the canine fossa as the anterior border.
The main functional component of the maxillary sinus outflow tract is the ostiomeatal complex, which is collectively constituted by the uncinate process, the maxillary ostium, the infundibulum, and the ethmoid bulla. These structures form a functional complex through which the maxillary sinus contents egress. Obstruction of the ostiomeatal complex and its relief with surgery form the basis for FESS.
The uncinate process is a sickle- or L-shaped bone that starts anterosuperiorly and then slopes posteroinferiorly, running horizontally from anterior to posterior. It has a free edge along its superior surface, which is taken down during uncinectomy. Superiorly, the uncinate process may attach to the lamina papyracea (most common configuration), the middle turbinate, or the skull base. At its most posterior point, it attaches to the inferior turbinate at the ethmoidal process.
Once the uncinate process is taken down, the natural maxillary sinus ostium can be visualized. The cilia of the maxillary sinus beat uphill toward the natural maxillary sinus ostium. Therefore, the natural ostium of the maxillary sinus must be included with maxillary antrostomy for maximal functional benefit.
If the natural ostium is missed, mucus recirculation may be a problem. The ethmoid bulla lies just posterior to the uncinate process and may be visible along with the uncinate process on routine nasal endoscopy. The ethmoid bulla, which is one of the features depicted in the image below, is the most constant anterior ethmoid air cell.
Surgical Options
Surgery is reserved for patients with confirmed chronic sinusitis—as documented by findings on history, physical examination, and CT scan—who have not responded to medical therapy.
Three main surgical options are available: (1) endoscopic uncinectomy with or without maxillary antrostomy, (2) the Caldwell-Luc procedure, and (3) inferior antrostomy (nasoantral window).
Today, endoscopic maxillary antrostomy and uncinectomy are the standard for treatment for refractory chronic maxillary sinusitis. The Caldwell-Luc and inferior antrostomy approaches are reserved for rare circumstances, such as a case of severe allergic fungal sinusitis in which standard antrostomy alone does not allow complete extirpation of fungal concretions or complete drainage.
Additionally, further FESS with mucosal-sparing techniques may be performed if additional disease is present within the ethmoid, sphenoid, and frontal sinuses.
Preoperative Steps
Consent should be obtained prior to any surgical procedure. This should include a thorough discussion of possible risks, such as orbital injury, blindness, nasolacrimal duct injury, epiphora, epistaxis, cerebrospinal fluid leak, meningitis and brain abscess, and, of course, persistent rhinosinusitis.
A preoperative antibiotic course may be administered in the weeks prior to surgery if an active infection is present. A preoperative steroid course may be administered if significant edema or polyps are observed on examination.
Endoscopic Maxillary Antrostomy
Before entering the operating room, the surgeon should select, inspect, and prepare all instrumentation, including image-guidance devices. In the preoperative holding area, nasal decongestion is begun with the patient receiving sprays of oxymetazoline. Following the commencement of general endotracheal anesthesia, the eyes are protected with eye ointment and thin strips of tape. The nasal passages are decongested with appropriate vasoconstrictors such as topical cocaine if not medically contraindicated.
If septoplasty is to be performed, the septum should be infiltrated with 1% lidocaine with 1:100,000 epinephrine in the submucochondrial plane. Then, the patient is draped and prepared for surgery. A 4-mm 0- or 30-degree endoscope may be used, depending on the surgeon's preference. If septoplasty is to be performed, it may be done either before or after sinus surgery. Place the septoplasty incision in the unobstructed nasal passage to allow better visualization of the more obstructed side.
Under endoscopic guidance, the middle turbinate may gently be moved medially, with care to avoid fracturing the turbinate–skull base junction. At this point, the uncinate process should be within view, and it is injected with 1% lidocaine with 1:100,000 epinephrine. Local injections can be made using a 10-mL control syringe with a Luer lock 27-gauge needle attached.
First, the root of the uncinate process is injected. Next, the inferior portion of the uncinate process is injected. The root of the middle turbinate is infiltrated as well. Finally, an injection is placed at the inferior junction of the basal lamella with the lateral nasal wall. This serves to vasoconstrict the sphenopalatine artery. Approximately 1-2 mL of local anesthetic is used at each injection site, with the bevel down (toward mucosa). An appreciable blanch of the mucosa should be observed with each injection.
If using an image-guided system, it can be calibrated at this time (thereby giving time for vasoconstriction from the injections to take effect). Alternatively, the system may be calibrated prior to beginning the case. When using an image-guided system, checking the position of the guidance tracking in a few different known points and confirming the accuracy in 3 dimensions is important. Typically, for isolated chronic maxillary sinus disease, image-guided surgery is not necessary.
After decongestion, uncinectomy is the next step. Uncinectomy can be performed in numerous ways. The following is the authors' preference. Under endoscopic guidance, a maxillary ostium seeker is insinuated just behind the uncinate process and used carefully to displace the free edge of the uncinate outwardly and anteriorly. To prevent lamina papyracea injury, care is taken to very gently manipulate only the uncinate process and not to penetrate deeply.
Next, 90-degree upbiting forceps are used to grasp the free edge of the uncinate process. In a controlled push-and-pull fashion, staying parallel to the lacrimal duct, the uncinate process is then removed. Care is taken to engage the uncinate process parallel to the lateral nasal wall to prevent injury to the lamina papyracea. Any remaining uncinate process may be removed using a combination of microdebrider powered instrumentation and pediatric forceps. All portions of the uncinate should be taken down completely to permit visualization of the natural maxillary sinus ostium, roughly parallel to the inferior portion of the middle turbinate.
Once the natural ostium is identified, an ostium seeker can be placed through the ostium and then carefully pushed posteriorly to widen the ostium. Using a through-cutting forceps, the ostium is enlarged, thereby completing a maxillary antrostomy. The maxillary sinus should be inspected with a 30- or 70-degree scope to ensure that no further disease is present within the sinus and that the natural ostium was included in the antrostomy. [4]
If either a microlith or a polyp is present, it may be removed using curved giraffe forceps or a curved suction. Further endoscopic work can be performed if disease is present in other sinuses.
If lateralization of the middle turbinate is a concern and to allow easier postoperative examination of the maxillary antrostomy in the office, the controlled synechiae technique, as described by Bolger et al, may be used. [5] Briefly, this involves abrading the opposing areas of mucosa from the medial middle turbinate and septum. With healing, the two roughened areas appose, thus medializing the turbinate for improved postoperative visualization of the maxillary sinus antrostomy.
The middle meatus may be packed with various products if either postoperative bleeding or lateralization of the middle turbinate is a concern. Many packing materials have been described, ranging from rolled Gelfilm to Merocel packing. The authors' preference is for a latex-free, glove-covered, trimmed Merocel in the middle meatus. This should be removed at the first postoperative visit (3-5 d).
A study by Costa et al indicated that endoscopic maxillary mega-antrostomy (EMMA) is an effective revision procedure in cases of chronic maxillary sinusitis that prove refractory to medical therapy and endoscopic antrostomy. The study included 28 patients who were followed up for a mean period of 6.9 years after EMMA; 72.4% of individuals reported complete or significant improvement in their condition, and the rest reported partial improvement. [6]
Balloon catheters in endoscopic sinus surgery
Balloon catheter technology has been used to dilate the maxillary sinus natural ostia without bone or soft-tissue removal. Early reports show sustained patient symptom improvement and sinus ostia patency. Further study and long-term outcomes with this technology will determine its role in endoscopic sinus surgery. [7]
A study by Soler et al indicated that balloon sinus dilation is safe and effective in children aged 2 years or older with chronic rhinosinusitis. The study, which looked at 157 sinus dilations, including 98 of the maxillary sinuses, found that for 92% of the patients, the Sinus and Nasal Quality of Life Survey score showed moderate to large improvement. The study’s subjects were aged 2 to 21 years, with 30 of the 50 patients undergoing procedures performed concomitantly with dilation. [8]
Similarly, a study by Zalzal et al indicated that balloon catheter sinuplasty offers long-term benefit in the treatment of pediatric chronic maxillary sinusitis. The report, which involved children under age 12 years who had previously undergone failed treatment with adenoidectomy and had a preoperative Lund-Mackay score of 5 or greater, found that 79% of patients had not experienced recurrent or persistent sinus infections by 3-year postprocedure follow-up, while 87% of them needed no further surgical intervention by 5-year follow-up. [9]
A clinical consensus statement from an expert panel of otolaryngologists included the following with regard to balloon dilation of the paranasal sinuses [10] :
-
Balloon dilation should not be performed in patients who do not have both sinonasal symptoms and positive computed tomography (CT) scan findings
-
Prior to balloon dilation, sinus CT scanning must be performed
-
Balloon dilation can serve as an adjunct to functional endoscopic sinus surgery (FESS) in chronic sinusitis patients without nasal polyps
-
Patients with limited chronic rhinosinusitis without polyposis can experience improved short-term quality-of-life outcomes via balloon dilation
FESS in patients with normal CT scans
A controversy as to whether FESS is useful for patients with history and physical examination findings that are consistent with recurrent or chronic sinusitis but who have relatively normal findings on CT scanning.
Little information exists in the literature regarding the optimal management of these patients with no abnormality detected on CT scanning, but one study with a very limited number of subjects demonstrated preliminary improvement in a very select group of patients without significant disease based on CT scan findings. [11]
At present, this subset of patients is thought to be a very small minority of patients with chronic rhinosinusitis, and every effort should be made to confirm the diagnosis of chronic sinusitis and to prescribe a comprehensive course of medical treatment, including allergy treatment and saline, before resorting to surgical treatment.
Caldwell-Luc Procedure
For patient comfort, this procedure typically is performed under general anesthesia. However, if medical comorbidities preclude general anesthesia, the procedure may be performed with local anesthetic and sedation. It may be performed in conjunction with nasoantral window (inferior antrostomy) to facilitate postoperative surveillance.
Lidocaine, 1% with 1:100,000 epinephrine, is injected in the incision site, and time is allowed for vasoconstriction. Make a 3-cm incision centered over the canine tooth and first premolar while leaving about 0.5-1 cm of gingiva intact above the dentition to facilitate closure.
Using electrocautery, dissection is carried down through the soft tissue and periosteum to bone. Next, a periosteal elevator is used to widely elevate periosteum from the anterior wall of the maxilla. Care is taken to identify and avoid injury to the infraorbital nerve, which is vertical and inferior to the midpupillary line. In the canine fossa, with mallet and osteotome, the maxillary sinus is entered through its anterior thin bone. Thereafter, rongeurs are used to enlarge the opening. Any pus from the maxillary cavity may be sent for culture. The disease within the sinus can be addressed appropriately. Next, the sinus is irrigated. The incision is then closed using 3-0 or 4-0 absorbable suture.
Inferior Antrostomy
Vasoconstriction is begun with topical oxymetazoline on pledgets. Next, 1% lidocaine with 1:100,000 epinephrine is injected under endoscopic guidance along the lateral nasal wall underneath the inferior turbinate. A 3-mL syringe with a 27-gauge needle facilitates the injection. Because the nasolacrimal duct lies approximately 1 cm anterior to the natural maxillary ostium, the injection and surgical antrostomy site is about one to two thirds of the distance back along the inferior turbinate.
Next, the maxillary sinus is punctured in this region using a curved suction or trocar. This antrostomy should then be enlarged with through-cutting forceps. The maxillary sinus disease should then be extirpated as appropriate.
Postoperative Steps
The stomach and nasopharynx should be suctioned prior to extubation. The surgeon should confirm with the anesthesiologist that an appropriate antiemetic was administered during surgery.
After extubation, the patient is taken to the postoperative care unit for recovery. Once the patient is awake, he or she is examined to check extraocular motility and to look for evidence of excessive bleeding or proptosis. If the patient is doing well, the individual may be discharged home after all postanesthesia protocol parameters have been satisfied.
Postoperative Follow-up
Postoperative care of the patient with chronic sinusitis is essential for long-term success. The patient is sent home with appropriate pain medications and instructions for nasal saline irrigations.
The patient returns for the first postoperative visit 3-5 days after surgery. At this time, the middle meatus packing is removed and all crusts and dried blood clots are carefully débrided. Weekly follow-up may be needed for the first month; biweekly follow-up with débridements may be indicated for the second month. After the second month, the patient is usually monitored quarterly for the first year. Further follow-up is then determined by the severity of the patient's disease, healing, and symptoms.
Further medical management after surgery, using antibiotics, nasal steroids, antihistamines, allergy medications, and oral steroids, is individualized based on the patient and further flares of sinusitis.
Common Causes of FESS Failure
Several studies have been conducted to elucidate the common causes of failure in FESS. These may include incomplete uncinectomy or failure to include the natural maxillary sinus ostium within the antrostomy, thereby creating recirculation between two ostia.
Lateralization of the middle turbinate or turbinate remnant and postoperative synechiae formation are also common. These pitfalls may be carefully avoided by performing a complete uncinectomy, identifying and enlarging the true maxillary sinus ostium, being gentle with medialization of the middle turbinate, and using a mucosal-sparing technique with through-cutting instrumentation to avoid excessive mucosal stripping.
Postoperative nasal endoscopic débridement is critical to decrease scarring and synechiae formation. The mucosa of the maxillary sinus should not be stripped routinely. The mucosa should be left intact because the mucosa that replaces stripped areas is devoid of proper ciliary function. This contributes to postoperative problems with mucus stasis and recurrent infection.
Occasionally, either secondary to scar band formation or in association with inferior antrostomy, recirculation may occur. This refers to the recirculation of maxillary sinus contents out of the natural ostium, along the mucosal band, and then back into the surgical antrostomy, thus creating an endless cycle of mucus build-up. To correct this, the intervening band of mucosa should be taken down to enlarge the antrostomy and to eliminate the cause of the recirculation.
Prognosis After FESS
Outcomes with properly selected patients for FESS have been outstanding. In 1989, Kamel reported a 96.8% patency rate for 94 endoscopic maxillary antrostomies (follow-up: 4-12 mo). [12] Of his 66 patients, 95.5% had subjective improvement in their symptoms. In 1993, Salam and Cable reported long-term 89% patency rate of 90 maxillary antrostomies with statistically significant improvements in headache, nasal obstruction, and pain with a 26-month mean follow-up. [13] Revision surgery is required in about 10% of cases.
Surgical Complications
Potential complications of endoscopic surgery
Complications of endoscopic surgery for chronic maxillary sinusitis may include orbital injury, blindness, orbital hematoma, nasolacrimal duct injury, epiphora, and postoperative epistaxis. Skull base injury and cerebrospinal fluid leak are very rare complications that should be discussed with patients undergoing endoscopic sinus surgery. With simple maxillary antrostomy, however, the risk of skull base injury should be negligible.
A study by Kim et al indicated that recurrent maxillary sinusitis after endoscopic sinus surgery may be associated with extensive trimming of the hypertrophied sinus mucosa. Such trimming may result in rapid shrinkage and fibrosis of the mucosa, causing stenosis at the site of middle meatal antrostomy and, consequently, the repeat development of sinusitis. [14]
In a study of children who underwent bilateral endoscopic middle meatal antrostomy, with or without partial or total ethmoidectomy, Ramadan et al found orbital injury to be the most common of the complications reviewed. The surgery was performed in 352 patients (age < 12 years), for uncomplicated chronic rhinosinusitis, with review made of such complications as skull base injury and cerebrospinal fluid (CSF) leak, orbital injuries (blindness, orbital hemorrhage, emphysema, periorbital swelling and bruising, fat exposure), and bleeding that mandated intervention. Thirty-one patients (8.8%) experienced complications, including skull base injury and CSF rhinorrhea (1 patient; 0.3%), orbital emphysema (3 patients; 0.85%), periorbital ecchymosis (5 patients; 1.4%), and violation of the lamina papyracea, with orbital fat exposure (22 patients; 6.3%). [15]
Potential complications of Caldwell-Luc procedure
The main complications associated with the Caldwell-Luc procedure include oroantral fistula, infraorbital nerve injury with associated hypesthesia, and injury to the tooth roots.
Potential complications of inferior antrostomy
The main risk associated with inferior antrostomy is nasolacrimal duct injury. Recirculation of mucus from the natural maxillary ostium through the newly created inferior antrostomy is possible. This usually occurs when inferior turbinate reduction is also performed.
-
Endoscopic view right nasal cavity; lacrimal bone (L), uncinate process (U), ethmoid bulla (B), middle turbinate (MT), nasal septum (S).
-
Hypoplastic right maxillary sinus.
Tables
What would you like to print?
- Surgical Overview
- Confirmatory CT Scans
- Anatomy of the Maxillary Sinus
- Surgical Options
- Preoperative Steps
- Endoscopic Maxillary Antrostomy
- Caldwell-Luc Procedure
- Inferior Antrostomy
- Postoperative Steps
- Postoperative Follow-up
- Common Causes of FESS Failure
- Prognosis After FESS
- Surgical Complications
- Show All
- Media Gallery
- References