Background
Much attention has been generated regarding the topic of thyroid neoplasia and papillary thyroid carcinoma. This attention can be attributed to the frequency of benign thyroid nodules and the clinical difficulty in distinguishing these nodules from malignant thyroid lesions.
History Of The Procedure
Theodor Billroth, who performed many thyroidectomies in the mid-1800s, was the first to observe side effects of total thyroidectomy in the form of postoperative cretinoid changes. He noticed his patients became sluggish, fat, cold, and even mentally deranged, a condition that would later be termed myxedema.
Thyroidectomy began to be used in the treatment of toxic goiters in 1907. Prior to this point, the surgery was used to treat nontoxic goiters, with toxic goiter patients considered poor surgical candidates. Radioactive iodine was introduced as a therapeutic intervention in 1942 by Means, Evans, and Hertz. This was followed by the introduction of thiouracil, in 1943, by Edwin Bennet Astwood.
Landmark innovations in many disciplines, particularly in anesthesia, physiology, and radiology, as well as in methods of hemostasis and antisepsis, contributed to the development of the surgical treatment of thyroid disease. Technologic innovations, such as video-assisted thyroidectomy, have further contributed to making these operations safer . [1]
Problem
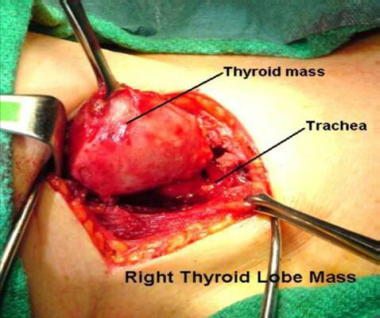
Thyroid nodules are found in up to 7% of the population. Only 4-6.5% of these nodules are malignant. Malignant tumors of the thyroid account for only about 1% of all cancers and only 0.4% of cancer-related deaths. The prognosis for papillary thyroid carcinoma is favorable; however, controversy exists regarding management of this cancer. Surgery is the primary mode of therapy for treatment, but the most appropriate type of resection for this disease is controversial. Open and minimally invasive procedures are illustrated below.
Epidemiology
Frequency
The American Cancer Society estimated that 44,280 new cases of thyroid cancer would be diagnosed in 2021. [2] Papillary thyroid carcinoma accounts for about 80% of all thyroid carcinomas in the United States.
The US incidence of thyroid cancer has more than tripled since the late 20th century, growing from nearly 5.0 new cases per 100,000 persons in 1975 to 15.5 new cases per 100,000 persons per year in the period between 2014 and 2018. [3, 4] Much of the increase has been due to a rise in the incidence of papillary thyroid cancer, which grew from 7.8 cases per 100,000 persons in 2003 to 15.4 cases per 100,000 persons in 2013. [4]
Despite the growth in the incidence of thyroid cancer, the disease's mortality rate has remained the same (0.5 deaths per 100,000). [5] Between 1988 (the first year the Surveillance, Epidemiology, and End Results [SEER] program collected data on tumor size) and 2002, 49% of the increase in thyroid cancer was attributable of tumors measuring 1 cm or smaller.
These trends, combined with the known existence of a substantial reservoir of subclinical cancer and stable overall mortality, have suggested that the rise in thyroid cancer's incidence has reflected increased detection of subclinical disease. Nonetheless, although controversy exists, there is growing evidence that the expanded incidence of reported thyroid cancer may be due to an increase in new cases. [6]
Thyroid cancer tumors most often occur in individuals aged 20-50 years. In adults, the female-to-male ratio of clinically diagnosed papillary carcinoma of the thyroid is 3:1; in children, the tumor is distributed nearly equally by sex. Although this condition is more common in females, they have a better overall prognosis. Papillary thyroid carcinoma occurs more often in whites than in blacks.
Etiology
The etiology of papillary carcinoma has yet to be elucidated, but a number of associations have been made. Multiple genetic and epigenetic mutations result in the activation of signaling pathways that precipitate thyroid cancer. Common mutations include point mutations of the BRAF and RAS genes and chromosomal rearrangements of RET/PTC and PAX8/PPARG. [7]
Moreover, research indicates that a link exists between higher body mass index (BMI) and greater tumor size, extrathyroidal invasion, and advanced tumor, node, metastasis (TNM) staging. [8]
Molecular
Activation of receptor tyrosine kinases (RET/PTC, TRK, MET), whether by rearrangement or gene amplification, appears to be specific for the transformation of thyroid follicular cells into papillary thyroid carcinomas. Often associated with exposure to ionizing radiation, these rearrangements produce chimeric proteins with tyrosine kinase activities that contribute to the development of the malignant phenotype. Approximately 40% of adults with sporadic papillary carcinoma have RET gene rearrangement, and about 15% have NTRK1 rearrangement. This rearrangement is higher (60%) in children.
Somatic point mutation in the BRAF gene may be the most common mutation among papillary thyroid cancers. Considered to be a poor prognostic marker, it varies from 29-69% in different series. This gene encodes a serine/threonine kinase acting on the RAS-RAF-MEK-MAPK signaling pathway. BRAF mutations seem to be much less common in childhood thyroid carcinomas. Identification of the BRAF mutation is making inroads into clinical practice as a diagnostic tool for the management of papillary thyroid cancers.
A 10-fold increased risk of thyroid cancer in relatives of patients with thyroid cancer suggests a genetic basis for susceptibility to these tumors. A correlation between papillary thyroid carcinoma and human leukocyte antigen (HLA)-DR7 has also been observed. Also, a parallel incidence has been described for this tumor in monozygotic twins.
Iodine excess
Papillary thyroid cancer has been induced in animals with the administration of excess iodine. In Vienna, Austria, during a period when iodide intake was low in the population, papillary carcinoma accounted for only 25% of all thyroid cancers instead of the expected 80%.
In areas where goiters are endemic, the addition of iodine to the diet has increased the proportion of papillary carcinomas relative to follicular thyroid cancer. However, these cancers are less aggressive and have a better prognosis for long-term survival.
While iodine excess has been linked to point mutations, however, a study of post-Chernobyl thyroid cancer indicated that an association exists between RET/PTC chromosomal rearrangements and iodine deficiency. [9] Conversely, excess iodine has been shown to have an antioncogenic role during RET/PTC3 oncogene activation. Studies have demonstrated a decreased papillary thyroid carcinoma rate in radiation-exposed regions where populations have an iodine-rich diet. [10]
Radiation
External radiation to the neck increases the incidence of papillary carcinoma of the thyroid later in life. Irradiation during childhood has been associated with the greatest risk for acquiring papillary thyroid cancer. As many as 9% of children irradiated for conditions such as tonsillar hypertrophy, thymic enlargement, and acne have developed thyroid cancer over a period of 20 years. Of the survivors of the atomic bomb explosions in Japan, 6.7% developed papillary thyroid cancers.
This percentage is much higher than what is expected in the general population. More recently, data have become available from studies of over 4000 people who developed thyroid cancer after the Chernobyl nuclear accident in 1986. [11] They revealed that radiation exposure during childhood carries an increased risk of thyroid cancer and that the risk is radiation dose dependent. The youngest children are most sensitive to radiation-induced carcinogenesis, and the minimal latent period for thyroid cancer development after exposure is as short as 4 years. The vast majority of these cancers are papillary carcinomas. On the molecular level, chromosomal rearrangements (such as RET/PTC) are more common than point mutations of BRAF and other genes.
Most studies have found that radiation exposure increases the risk of developing thyroid cancer without affecting the patient's prognosis or the aggressiveness of the tumor. Some studies, however, have suggested that radiation may induce a more aggressive course. [12] While treatment with radioactive iodine has not been shown to raise the incidence of thyroid cancers, a meta-analysis demonstrated an increase in the risk of thyroid, kidney, and stomach cancer at diagnostic doses of greater than 1 Gy. [13]
Pathophysiology
Gross description
Papillary carcinomas can range in size from microscopic, clinically undetectable lesions to masses of up to 10 cm in diameter. The average tumor size at diagnosis is 2.3 cm. Up to 75% of these tumors are multifocal within the thyroid. Most are pale and firm on gross examination; less than 10% of papillary carcinomas are truly encapsulated, with larger nodules usually unencapsulated and locally invasive. Penetration of the capsule of the thyroid gland occurs in about 40% of cases.
Microscopic description
Well-differentiated thyroid carcinomas are the most common types of thyroid carcinoma. These include papillary and follicular thyroid carcinomas. Both arise from the endodermally-derived follicular cells that synthesize thyroxine and thyroglobulin. This is in contrast to medullary thyroid carcinoma, which is derived from the neuroendocrine calcitonin-producing parafollicular C cells of the thyroid.
Papillary tumors can have pure papillary histopathology, but more than one half contain an admixture of follicular elements. Regardless of the precise proportions, all neoplasms containing some papillary areas have identical biologic behavior; therefore, they are classified under the papillary, rather than the follicular, carcinomas.
The histopathologic diagnosis of follicular variant of papillary thyroid carcinoma (FVPCA) can be difficult. Lloyd (2004) examined interobserver variation by 10 experienced thyroid pathologists in the diagnosis of FVPCA in 87 tumors. [14] A concordant diagnosis of FVPCA was made by all 10 reviewers with a cumulative frequency of 39%. Diagnostic criteria used to diagnose FVPCA, including pseudoinclusions, nuclear grooves, and powdery nuclei, are clearly not uniformly recognized, even by experts. Immunohistochemical markers, such as single nucleotide polymorphisms and messenger ribonucleic acid (mRNA) expression of VEGF-A, are being shown to provide more objective diagnostic criteria. [15, 16]
Initially, the immunohistochemical expression of cytokeratin 19, galectin-3 and HBME-1, 3 malignancy-related markers in thyroid papillary carcinoma, including its follicular variant, was used with caution. [17, 18] However, a study by de Matos et al found that these biomarkers can be used to accurately diagnose malignant and benign lesions both preoperatively and postoperatively. [19]
Thus, genetic alterations in papillary carcinoma of the thyroid may hold the ultimate key to diagnosis. Three genetic alterations, including BRAF point mutations, RET/PTC rearrangements, or RAS point mutations, have been recognized in this regard. In a study by Adeniran (2006), these alterations have been shown to be associated with distinct microscopic, clinical, and biologic features of thyroid papillary carcinomas. [20] BRAF mutations were associated with older age, taller cell appearance, and more advanced tumor stage at presentation. RET/PTC rearrangements presented at a younger age, showed typical papillary histology, and were associated with a high rate of lymph node metastases. Tumors with RAS mutations were exclusively of FVPCAs.
The identification of these alterations has increasingly led to the diagnostic and prognostic use of genetic studies in papillary thyroid carcinoma. Several genetic panels have been developed to identify genes specific to thyroid cancer and are now in clinical use. [21, 22] These involved genes may also serve as targets for cancer chemotherapy in patients in whom standard thyroid cancer treatment has not been effective.
The histologic features of papillary carcinoma of the thyroid include branching papillae composed of a central fibrovascular core and a single or stratified lining of cuboidal to columnar cells. Tumor cells may form colloid-containing follicles, and foci of squamous metaplasia are frequently found. Nuclear atypia is also an important diagnostic feature.
In more than half of these tumors, the nuclei have a characteristic ground-glass appearance; laminated calcific spherules known as psammoma bodies are also often found within the histological framework. In fact, the presence of psammoma bodies is virtually diagnostic for papillary carcinoma because they are rarely found in other lesions.
Papillary thyroid carcinomas typically invade the lymphatics and spread to other sites within the thyroid gland, as well as to the regional lymph nodes. Lymph node metastases have been reported in the range of 46-90% of cases of papillary carcinoma. Vascular invasion is uncommon; however, if it does occur, the spread of tumor is usually to the lungs and bones. Direct extension into the soft tissues of the neck occurs in approximately 25% of cases.
Variants
The variants of papillary thyroid carcinoma include the following:
-
Encapsulated tumors: About 10% of papillary carcinomas are completely surrounded by a dense fibrous capsule; the prognosis for patients with such tumors is better than the prognosis for patients with unencapsulated papillary carcinoma
-
Diffuse sclerosing variant: Occurring at a younger age, the diffuse sclerosing variant constitutes 2% of papillary carcinomas and may cause a diffuse goiter without palpable nodules that can be mistaken for goitrous autoimmune thyroiditis; diffuse involvement of one or both lobes occurs with dense sclerosis, patchy lymphocytic infiltration, and abundant psammoma bodies; prognosis for individuals with the diffuse sclerosing variant is less favorable than that for individuals with typical papillary thyroid carcinoma
-
Oxyphilic (Hürthle) cell type: The oxyphilic (Hürthle) cell type variant has typical papillary architecture but may be more aggressive than usual papillary carcinoma
-
Follicular variant: The follicular variant has a purely follicular architectural pattern but may be recognized by the typical cellular features of papillary carcinoma
-
Tall cell carcinoma: Tall cell carcinoma is a more aggressive form of thyroid carcinoma that differs from the usual form by showing tall columnar cells; the frequency of more aggressive behavior is higher, but the carcinoma resembles papillary carcinoma in other morphologic and clinical aspects
-
Columnar cell carcinoma: Columnar cell carcinoma is a distinctly more aggressive form of papillary thyroid carcinoma that occurs more often in older men and is associated with a poor prognosis
-
Solid cell variant: The lesion is made up of sheets of tumor cells that have the cytologic features of typical papillary thyroid carcinoma; about one third of cases exhibit vascular invasion and extrathyroidal extension; the tumors arise more often in pediatric patients with a history of radiation exposure [23]
-
Papillary thyroid carcinoma with prominent hobnail features: Research indicates that usually more than 30% of the tumor has hobnail features; a small percentage of these lesions have been found to have tall cell and diffuse sclerosing patterns; the carcinomas are very aggressive, with mortality from metastatic papillary thyroid carcinoma reported in 50% of cases [23]
Presentation
The mainstays of the preoperative diagnosis of papillary carcinoma are a thorough history and physical examination, including an assessment of risk factors, along with ancillary tests such as cervical ultrasonography and aspiration cytology.
The most common presentation of thyroid cancer is a nontender palpable nodule. However, a diagnostic dilemma is present as this is the presentation of most benign thyroid conditions. A palpable nodule occurs in up to 7% of the general female population. A single nodule has a 5-12% malignancy rate, while multiple nodules have a 3% malignancy rate in the general population.
Papillary carcinoma may also present as a nodule with enlarged cervical lymph nodes or cervical lymphadenopathy in the absence of a palpable thyroid nodule. Benign thyroid tissue can be found in the neck anywhere medial to the sternocleidomastoid muscle. Any thyroid tissue lateral to the sternocleidomastoid muscle should be considered malignant.
Unlike follicular thyroid carcinoma, distant metastases of papillary thyroid carcinoma are rarely observed at the time of presentation. When distant metastases are present at the time malignancy is discovered, the primary tumor is almost invariably large and easily palpable.
Indications
During routine physical examination or ultrasonography, symptoms of dysphagia, odynophagia, or shortness of breath may lead to the discovery of a thyroid mass. The presence of a mass in the thyroid requires further investigation, especially in high-risk patients.
Lobectomy is indicated in patients who have isolated, indeterminate, solitary nodules who prefer a more limited surgical procedure. Lesions of less than 1 cm that are low-risk, unifocal, or intrathyroidal in the absence of prior head and neck irradiation can also qualify for lobectomy. Total thyroidectomy is indicated for the following:
-
Lesions of greater than 1 cm
-
Indeterminate nodules that have large tumors (>4 cm) with atypia on biopsy
-
Biopsy readings that are suspicious for papillary carcinoma
-
Patients with a family history of thyroid carcinoma
-
Patients with a history of radiation exposure
-
Patients with indeterminate nodules who have bilateral nodular disease [24]
In patients with clinically involved central or lateral neck lymph nodes, total thyroidectomy should be accompanied by clearance of the central neck of disease by therapeutic central-compartment (level VI) neck dissection. If the central neck lymph nodes are clinically uninvolved, patients with papillary thyroid carcinoma can still undergo prophylactic, ipsilateral or bilateral central-compartment neck dissection. However, in patients with small (T1 or T2), noninvasive papillary thyroid cancer that is clinically node-negative, thyroidectomy without central neck dissection may be appropriate. [24]
Lateral neck compartmental lymph node dissection is indicated when there is biopsy-proven metastatic lateral cervical lymphadenopathy. [24]
Relevant Anatomy
Knowledge of the anatomy of the infrahyoid neck and thyroid region aids in the identification and preservation of structures (eg, recurrent laryngeal nerve, superior laryngeal nerve, superior thyroid artery, inferior thyroid artery). The isthmus of the thyroid usually overlies the third tracheal ring, although this middle portion of the gland may be absent altogether in some individuals. The thyroid gland consists of a superior pole that may extend as far as the oblique line of the thyroid cartilage, and an inferior pole that may extend as far as the sixth tracheal ring.
The external branch of the superior laryngeal nerve innervates the cricothyroid muscle near the superior pole. The left recurrent laryngeal nerve lies in the tracheoesophageal groove, while the right recurrent laryngeal nerve approaches the thyroid gland from a more lateral position. The superior thyroid artery is the first branch of the external carotid artery and often accompanies the external laryngeal branch of the superior laryngeal nerve near the superior pole of the thyroid as it runs superficially toward the isthmus. The inferior thyroid artery arises from the thyrocervical trunk, which comes off of the subclavian artery. This artery runs in the tracheoesophageal groove and sends branches to the posterior aspect of the lateral thyroid lobe. The inferior thyroid artery has a longitudinal branch that anastomoses with the superior thyroid artery near the superior pole.
Contraindications
Surgical excision of papillary thyroid carcinoma has no absolute contraindications. Even people with distant metastasis would benefit from surgical removal of the primary disease, neck dissection, and ablation with iodine-131.
A total thyroidectomy may be contraindicated in people with disease limited to only one lobe of the thyroid who are likely to be noncompliant with thyroid replacement therapy. These individuals may be better suited for a hemithyroidectomy.
-
Standard open thyroidectomy.
-
Minimally invasive video-assisted thyroidectomy. Courtesy of Ruggieri et al. BMC Surgery 2005 5:9 doi:10.1186/1471-2482-5-9
-
Minimally invasive thyroidectomy; identification of the recurrent laryngeal nerve.
-
Minimally invasive thyroidectomy closure.
-
Minimally invasive thyroidectomy; division of isthmus and delivery.
-
Minimally invasive thyroidectomy; incision and exposure.
-
Minimally invasive thyroidectomy; initial dissection.
-
Minimally invasive thyroidectomy; superior pole release.