Practice Essentials
Malignancies of the upper aero-digestive tract are a leading cause of death in the United States, and treatment of laryngeal carcinoma has changed over the past few decades. Until approximately 1990, therapy was surgically directed. Total and partial laryngectomy surgeries were and still are the mainstream surgical procedures to treat malignant tumors of the larynx. However, a paradigm change in treatment occurred in the early 1990s with the advent of organ preservation treatments using concurrent chemoradiation therapy. This treatment approach demonstrated survival rates similar to total laryngectomy plus radiation therapy, while preserving the larynx in 63% of the patients. In addition, new developments in endoscopic surgical techniques and laser equipment are opening a new era in the treatment of malignant tumor of the larynx.
Among all the cancers of the upper aero-digestive tract, squamous cell carcinoma is the most common. Approximately 40,000 new patients are diagnosed with squamous cell carcinoma of the head and neck each year in the United States.
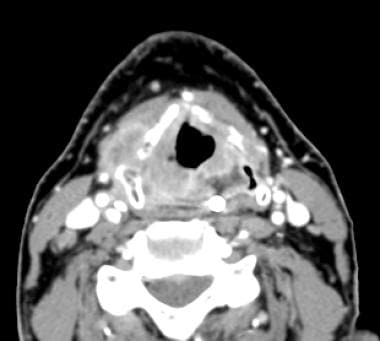
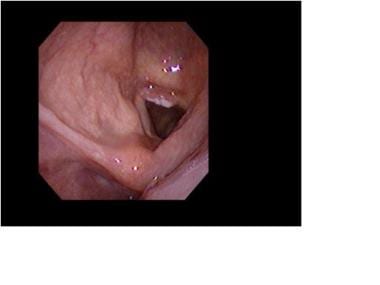
A tumor of the larynx can be seen in the image below.
Workup of malignant laryngeal tumors
Contrast-enhanced computed tomography (CT) scans obtained with appropriate section thickness (1-2 mm–thick sections through the larynx) aid in the evaluation of neck masses.
CT and magnetic resonance imaging (MRI) scans may demonstrate the extension of tumor into vital structures such as the surrounding soft tissue, the preepiglottic space. They may also show invasion though the thyrohyoid-ligament and cartilage invasion.
Positron emission tomography-CT (PET-CT) scanning is the most sensitive test available to detect metastasis or second primary tumors.
Direct laryngoscopy provides an opportunity for examination under general anesthesia, palpation and biopsy. Suspension laryngoscopy provides an excellent view of the extent of the tumor and the overall condition of the airway mucosa. When coupled with appropriate imaging such as a CT scan, the direct laryngoscopy provides the best information for tumor staging and surgical planning. The direct laryngoscopy also provides an opportunity for biopsies of the tumor to be obtained. Well-targeted biopsies will typically reveal the type and perhaps grade of the tumor.
Management of malignant laryngeal tumors
Early stage laryngeal carcinomas (stage I-II) are ideally treated with either radiation or surgical techniques (either endoscopic or open) that preserve laryngeal function. For carcinoma in situ or early stage invasive glottic or supraglottic cancer, endoscopic surgical excision or radiation therapy are both equally effective, with similar functional outcomes.
Historically, advanced-stage laryngeal carcinomas (stage III-IV) were treated with total laryngectomy, reconstruction, and adjuvant postoperative chemoradiation therapy. Although total laryngectomy is still required in cases of aggressive or extensive tumors, laryngeal preservation strategies using chemotherapy and radiation therapy protocols have now become the standard of care for many advanced laryngeal cancers.
In addition to total laryngectomy, other surgical techniques used in the treatment of malignant laryngeal tumors include transoral laser microsurgery (ideal for the management of early/intermediate glottic and supraglottic cancer), open supraglottic partial laryngectomy, and supracricoid partial laryngectomy.
History Of The Procedure
The development of the technique of direct laryngoscopy by Manuel Garcia in 1855 provided the ability to examine the larynx in a living person for the first time. The first laryngofissure procedure for cancer was performed by Gurdon Buck in 1851, while Theodor Billroth is credited with the first laryngectomy in 1873. Postoperative mortality from this procedure was very high (around 40%), mainly due to aspiration and sepsis.
Constant improvement in technique and perioperative care led to improved outcomes. A standardized laryngectomy technique perfected by Gluck and Soerensen by 1922 yielded excellent surgical outcomes with few fatalities. Billroth and Gluck also described hemilaryngectomies, but these procedures resulted in high recurrence rates and intractable dysphagia. Partial laryngectomies gradually regained an important role as a therapeutic option for laryngeal cancer mainly through improved techniques and recognition of appropriate indications. In recent years, surgery of laryngeal cancer has evolved to refined endoscopic and laser techniques.
Problem
New strategies using chemotherapy, radiotherapy and surgery have not substantially changed the survival rate of patients with advanced malignant tumors of the larynx in the last 30 years. Tobacco and alcohol are recognized as the major risk factors for developing malignant tumors of the larynx. New efforts in understanding the molecular biology and carcinogenesis of laryngeal malignancies have given us knowledge in the evolution of this disease and have shown therapeutic potential. The main challenge in laryngeal cancer treatment is improving survival while preserving function by limiting treatment toxicities.
Epidemiology
Frequency
According to the Surveillance, Epidemiology, and End Results (SEER) program of the National Cancer Institute (NCI), an estimated 12,380 men and women were diagnosed with cancer of the larynx (0.6% of all new cancer cases) in 2023, with an estimated 3820 deaths from the disease (0.6% of all cancer deaths) that year. The age-adjusted incidence of laryngeal cancer is 2.7 new cases per 100,000 men and women annually, with an age-adjusted mortality rate of 0.9 per 100,000 people annually. [1]
According to the NCI, the age-adjusted rate for new cases of laryngeal cancer dropped by an average of 2.4% per year between 2008 and 2017, while the age-adjusted death rate decreased by an average of 2.3% annually between 2009 and 2018. [1]
Sex
A study by Marchiano et al indicated that subglottic squamous cell carcinoma cases have a male-to-female ratio of 3.83:1. The report included 889 cases from the NCI's SEER program database. [2]
Age
According to the Marchiano study, subglottic squamous cell carcinoma predominantly occurs in the fifth to seventh decade of life. [2]
Etiology
Until the complex molecular interactions of all associated etiologic agents for any cancer can be understood, these interactions are best thought of as associations. Thinking of intrinsic (eg, genetic) factors and/or extrinsic (eg, smoking) factors as causes is too simple. [3]
To most people, a cause implies a condition that is both necessary and sufficient to produce a prespecified result. Laryngeal carcinomas have multiple associations.
The foremost risk factor for the development of laryngeal cancer is tobacco use. The risk of developing laryngeal cancer with tobacco increases with use and decreases after cessation. When associated with the intake of alcohol, a strong synergistic effect is created. However, whether or not alcohol alone is an independent risk factor is still unclear. Potential risk factors linked to the development of laryngeal cancer include:
-
Tobacco use
-
Excessive ethanol use
-
Male sex
-
Infection with human papillomavirus
-
Increasing age
-
Diets low in green leafy vegetables
-
Diets rich in salt preserved meats and dietary fats
-
Metal/plastic workers
-
Exposure to paint
-
Exposure to diesel and gasoline fumes
-
Exposure to asbestos
-
Exposure to radiation
-
Laryngopharyngeal reflux
A study by Zhao et al suggested that an association exists between overexpression of histone deacetylase 1 (HDAC1) and the clinical characteristics of laryngeal squamous cell carcinoma. A correlation was indicated, for example, between upregulation of HDAC1 expression and T classification, tumor clinical stage and location, lymph node metastases, and the cancer’s sensitivity to radiotherapy, with higher expression of HDAC1 found in the low-sensitivity squamous cell cancer samples. Patients in whom HDAC1 was overexpressed and with low sensitivity to radiotherapy had a poorer overall 5-year survival rate. [4]
Pathophysiology
The larynx is an essential organ that is responsible for the following vital functions:
-
Maintaining an open air way
-
Vocalizing
-
Protecting the lungs from direct exposure to noxious fumes and gases of unsuitable temperatures
-
Protecting the lungs from aspiration of solids and liquids
-
Allowing leverage, by closing the glottis during a Valsalva maneuver, to increase upper-body strength and to ease defecation
Malignant tumors of the larynx may affect laryngeal physiology depending on tumor location and size. Supraglottic tumors may not alter laryngeal function until they reach a relatively large size, at which time airway obstruction may be the first symptom. Conversely, glottic tumors alter voice quality early in their development and are thus often discovered at an early stage. In addition, malignant tumors of the larynx affect swallowing physiology. The mechanism of swallowing is altered when tumors invade and alter the physiology of the swallowing muscles. This may lead to either dysphagia or aspiration.
Development and progression of malignant tumors of the larynx occurs at the molecular and histologic level. The molecular steps involved in tumorigenesis have not been fully elucidated and likely vary from patient to patient. Histologic progression occurs from normal laryngeal mucosa to dysplastic mucosa to carcinoma in situ to invasive carcinoma. This progression is a multistep process of accumulated genetic events that lead to the development of larynx tumors.
Presentation
Given the functions of the larynx mentioned above, one can easily imagine the consequences of a carcinoma destroying and/or obstructing the laryngeal structures and their functions (eg, vocal-cord movement). Symptoms vary with the structures involved by malignancy and its accompanying inflammatory reaction. Although the particular tumor, the site, and the patient's constitution all contribute to the spectrum of symptoms seen in any given individual, laryngeal cancers as a whole can cause any of the following findings, alone or in combination:
-
Dysphonia/aphonia
-
Dysphagia
-
Dyspnea
-
Aspiration
-
Blood-tinged sputum
-
Fatigue and weakness
-
Cachexia
-
Pain
-
Expectoration of tissue
-
Neck mass
-
Otalgia (Outside the field of otorhinolaryngology, many physicians do not realize that otalgia may be a sign of laryngeal cancer. This seems to be especially true if the arytenoids are involved.)
History
As in all clinical evaluations, the history is the first step in gathering the facts. Assess or inquire about the following:
-
Weight loss
-
Fatigue
-
Pain
-
Difficulty breathing or swallowing
-
Vocal changes noted by the patient and his or her family
-
Ear pain
-
Coughing up blood or solid material
Physical examination
The patient's general condition and nutritional status should be evaluated. A full head and neck examination should be completed. Head and neck examination includes inspection and palpation of the oral cavity and oropharynx to rule out second primary tumors or other lesions, as well as evaluation of dentition. Inspection of the larynx is best accomplished using a flexible laryngoscope. Flexible laryngoscopy allows the otolaryngologist to evaluate the function and anatomy of the entire larynx. Evaluation of vocal cord mobility and the location and extension of the tumor are crucial to stage the patient accurately. Palpation of the neck looking for enlarged lymph nodes is paramount in the patient's evaluation. Thorough evaluation of the cranial nerves should also be included in the physical examination.
Indications
Many laryngeal tumors may appear late with distant metastasis and near-total destruction of some neck structures. Others may appear early. Treatment is necessary for all tumors. Treatment may include single therapy or combinations of surgery, radiation therapy, and/or chemotherapy. In advanced metastatic tumors, treatment may be only palliative, but it should still be addressed because tumors of the larynx can cause severe misery for the patient and his or her loved ones. To select proper therapy, all of the necessary information must first be obtained before available options are discussed with the patient.
The anatomy of the larynx is complex and difficult to visualize. Nevertheless, the team caring for each patient must understand it. Specialists in the areas of head and neck surgery, pathology, radiation oncology, and radiology understand this anatomy well. For family members, patients, and clinicians who do not deal with anatomic detail in their daily practice, this is a complicated arena. The entire team must effectively understand each other and communicate with the family.
Relevant Anatomy
Entire books are written about gross and microscopic laryngeal anatomy. The discussion below is an abbreviated version of the relevant anatomy. It should provide the information any clinician needs to understand this anatomic region, and it should explain why different procedures are indicated in different areas. It also helps in clarifying the consequences of each procedure.
The larynx is divided into the supraglottic larynx, the glottis or glottic larynx, and the subglottic larynx. The supraglottic larynx includes the epiglottis, the preepiglottic space, the laryngeal aspects of the aryepiglottic folds, the false vocal cords, the arytenoids, and the ventricles. The inferior boundary is a horizontal plane drawn trough the apex of the laryngeal ventricles. This corresponds to the area of transition from squamous epithelium superiorly to respiratory epithelium inferiorly. The glottis consists of the true vocal cords extending to roughly 1 cm below the true cords, the paraglottic space, and the anterior and posterior commissures. The subglottic larynx has its superior border at the inferior border of the glottis, that is, approximately 1 cm below the true vocal cords and extending inferiorly to the trachea.
See the image below.
Contraindications
Therapy has no "contraindications." However, a multitude of issues must be discussed in deciding which therapy is best for each patient. These issues include such things as the tumor stage, the patient's co-morbid status, prior treatments, and, of course, the patient's desires. Even in the setting of tumor recurrence and incurability, the patient should be offered palliative care.
-
Fiberoptic endolaryngeal view of an early glottic lesion of the right true vocal cord extending to the anterior commissure.
-
Axial view on CT scan of an advanced right laryngeal tumor invading through the thyroid cartilage.
-
PET/CT image of a laryngeal cancer showing increased FDG avidity.
-
Tracheostoma and skin flap reconstruction following total laryngectomy for a locally advanced laryngeal cancer invading the skin of the neck.