Practice Essentials
The oropharynx is a common location of upper aerodigestive tract malignancies, and each subsite of the oropharynx, including the base of tongue, has different diagnostic, therapeutic, and prognostic characteristics. The majority of base of tongue malignancies are squamous cell carcinomas (SCCs), but other malignant processes can arise, including lymphoepithelial carcinomas, hematolymphoid tumors, salivary gland tumors, and mucosal melanomas. [1] (See the images below.)
 A sagittal computed tomography (CT) scan of the neck with contrast demonstrates a pedunculated soft tissue lesion at the left base of the tongue without invasion of the floor of the mouth or adjacent structures. The mass measures approximately 2.7 x 1.8 x 2.8 cm.
A sagittal computed tomography (CT) scan of the neck with contrast demonstrates a pedunculated soft tissue lesion at the left base of the tongue without invasion of the floor of the mouth or adjacent structures. The mass measures approximately 2.7 x 1.8 x 2.8 cm.
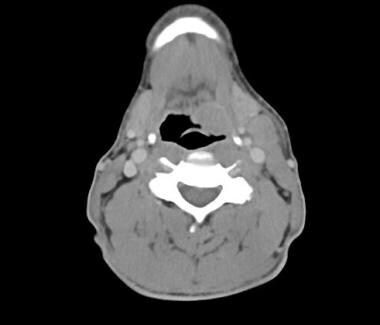 An axial CT scan of the neck with contrast again demonstrates a soft tissue left base of tongue lesion with slight extension into the glossotonsillar sulcus. There is also an enlarged, pathologic-appearing, left level II cervical lymph node.
An axial CT scan of the neck with contrast again demonstrates a soft tissue left base of tongue lesion with slight extension into the glossotonsillar sulcus. There is also an enlarged, pathologic-appearing, left level II cervical lymph node.
Historically, tobacco and/or alcohol use were the primary risk factors for oropharyngeal tumors. However, there has been a significant change in the epidemiology of base of tongue tumors, with a substantial increase in human papillomavirus (HPV)–associated oropharyngeal SCC. Fortunately, patients with these HPV-associated tumors have a much better response to treatment and improved prognosis compared with individuals with traditional, non-HPV oropharyngeal SCCs. [2, 3] It is estimated that overall, oropharyngeal SCCs will make up about 47% of all head and neck cancers in the United States by 2030. [4]
Careful multidisciplinary assessment of base of tongue tumors is paramount for appropriate treatment, which is based on staging, pathology, tumor location, functional outcomes, and patient preference. Survival and prognosis depend on early detection and initial staging of the disease. Because of the nonspecific nature of associated symptoms, however, patients with base of tongue tumors may present with advanced disease. Moreover, the disease process and associated treatment modalities can often affect adjacent upper aerodigestive structures, which impacts speech, swallowing, and quality of life (QOL).
Despite the complex anatomy associated with base of tongue tumors, as well as concerns regarding posttreatment functional deficits, significant changes in management options for such neoplasms have vastly improved outcomes in recent years.
Workup in malignant tumors of the base of tongue
Imaging
Cross-sectional imaging is an important tool for the diagnosis and clinical staging of malignant tumors of the tongue base. High-resolution computed tomography (CT) scanning of the neck with intravenous (IV) contrast is the most commonly utilized modality and has the advantages of increased availability and speed, with excellent spatial resolution, demonstration of bone infiltration, and lymph node visualization.
Magnetic resonance imaging (MRI) of the neck is more costly but can be utilized as an alternative to neck CT scanning.
Positron emission tomography (PET) scanning with CT imaging is used in the evaluation of unknown primary tumors, synchronous primary tumors, and distant metastases. [5]
Biopsy
Biopsy via endoscopic examination of the primary site with the patient under anesthesia remains the definitive procedure to establish the diagnosis and accurately assess the primary tumor.
Management of malignant tumors of the base of tongue
The decision to use surgical excision and other treatment modalities for malignant base of tongue tumors is primarily based on pathology, initial staging, tumor location, medical comorbidities, smoking history, and patient preference. Other important considerations include a patient's overall health and the individual's ability to tolerate prolonged intraoperative anesthesia versus chemotherapy and radiation therapy. Depending on the extent of surgery required and the potential need for reconstruction, patients may require a temporary nasogastric feeding tube and/or tracheostomy tube in order to maintain adequate nutrition and protect the airway. Additionally, tumors may be considered unresectable because of their size/location or the extent of the disease or due to invasion into critical structures.
Early stage base of tongue SCC can be treated with surgical therapy and/or radiation. Advanced-staged tumors may be treated surgically with adjuvant radiation/chemoradiation versus definitive chemoradiation. Advances in surgical techniques, including endoscopic and transoral laser/robotic approaches, as well as free tissue transfers for reconstructive surgery, have decreased the morbidity historically associated with base of tongue surgery. Most recent guidelines from the National Comprehensive Cancer Network (NCCN) require p16 testing for the presence of HPV, consequently changing the treatment recommendations for and staging of these tumors.
Background
The oropharynx is a common location of upper aerodigestive tract malignancies, and each subsite of the oropharynx, including the base of tongue, has different diagnostic, therapeutic, and prognostic characteristics. The majority of base of tongue malignancies are squamous cell carcinomas (SCCs), but other malignant processes can arise, including lymphoepithelial carcinomas, hematolymphoid tumors, salivary gland tumors, and mucosal melanomas. [1] (See the images below.)
 A sagittal computed tomography (CT) scan of the neck with contrast demonstrates a pedunculated soft tissue lesion at the left base of the tongue without invasion of the floor of the mouth or adjacent structures. The mass measures approximately 2.7 x 1.8 x 2.8 cm.
A sagittal computed tomography (CT) scan of the neck with contrast demonstrates a pedunculated soft tissue lesion at the left base of the tongue without invasion of the floor of the mouth or adjacent structures. The mass measures approximately 2.7 x 1.8 x 2.8 cm.
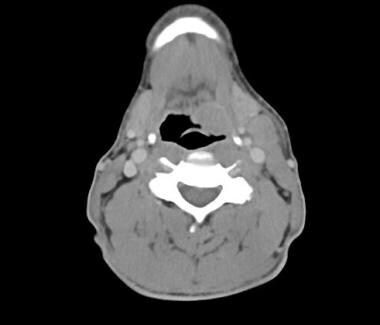 An axial CT scan of the neck with contrast again demonstrates a soft tissue left base of tongue lesion with slight extension into the glossotonsillar sulcus. There is also an enlarged, pathologic-appearing, left level II cervical lymph node.
An axial CT scan of the neck with contrast again demonstrates a soft tissue left base of tongue lesion with slight extension into the glossotonsillar sulcus. There is also an enlarged, pathologic-appearing, left level II cervical lymph node.
Historically, tobacco and/or alcohol use were the primary risk factors for oropharyngeal tumors. However, there has been a significant change in the epidemiology of base of tongue tumors, with a substantial increase in human papillomavirus (HPV)–associated oropharyngeal SCC. Fortunately, patients with these HPV-associated tumors have a much better response to treatment and improved prognosis compared with individuals with traditional, non-HPV oropharyngeal SCCs. [2, 3] It is estimated that overall, oropharyngeal SCCs will make up about 47% of all head and neck cancers in the United States by 2030. [4]
Careful multidisciplinary assessment of base of tongue tumors is paramount for appropriate treatment, which is based on staging, pathology, tumor location, functional outcomes, and patient preference. Survival and prognosis depend on early detection and initial staging of the disease. Because of the nonspecific nature of associated symptoms, however, patients with base of tongue tumors may present with advanced disease. Moreover, the disease process and associated treatment modalities can often affect adjacent upper aerodigestive structures, which impacts speech, swallowing, and quality of life (QOL).
Despite the complex anatomy associated with base of tongue tumors, as well as concerns regarding posttreatment functional deficits, significant changes in management options for such neoplasms have vastly improved outcomes in recent years.
Management of malignant tumors of the base of tongue
The decision to use surgical excision and other treatment modalities for malignant base of tongue tumors is primarily based on pathology, initial staging, tumor location, medical comorbidities, smoking history, and patient preference. Other important considerations include a patient's overall health and the individual's ability to tolerate prolonged intraoperative anesthesia versus chemotherapy and radiation therapy. Depending on the extent of surgery required and the potential need for reconstruction, patients may require a temporary nasogastric feeding tube and/or tracheostomy tube in order to maintain adequate nutrition and protect the airway. Additionally, tumors may be considered unresectable because of their size/location or the extent of the disease or due to invasion into critical structures.
Early stage base of tongue SCC can be treated with surgical therapy and/or radiation. Advanced-staged tumors may be treated surgically with adjuvant radiation/chemoradiation versus definitive chemoradiation. Advances in surgical techniques, including endoscopic and transoral laser/robotic approaches, as well as free tissue transfers for reconstructive surgery, have decreased the morbidity historically associated with base of tongue surgery. Most recent guidelines from the National Comprehensive Cancer Network (NCCN) require p16 testing for the presence of HPV, consequently changing the treatment recommendations for and staging of these tumors.
Etiology
Chronic alcohol use and prolonged tobacco consumption, including smokeless tobacco use, are traditional and synergistic risk factors for head and neck malignancies such as base of tongue SCC. [6, 7] HPV infection is another significant risk factor and is closely associated with the rise in oropharyngeal SCC cases, especially among healthy, middle-aged Caucasian males. A meta-analysis by Mehanna et al showed a drastic and significant increase in the overall prevalence of HPV-positive oropharyngeal SCC over time, as follows [8] :
-
Before 2000 - 40.5%
-
2000-2004 - 64.3%
-
2005-2009 - 72.2%
Persistent oral HPV infection is the most likely precursor for the development of HPV-associated oropharyngeal SCC, but the pathophysiology of the disease and how it arises from the initial infection are still unclear. [9, 10, 3] Some studies have suggested that sexual history, including engagement with multiple sexual partners and in oral sex, is associated with HPV infection and the risk of HPV-associated SCC. [11, 12] Among the oncogenic HPV subtypes that have been identified in oropharyngeal SCCs, the high-risk subtype 16 has been found to be present in 90% of them. [1, 13]
Pathophysiology
The tongue is a vital organ that plays a critical role in speech, taste, mastication, and swallowing. During the oral phase of swallowing, food and liquid are propelled toward the oropharynx from the oral cavity by the tongue. During the subsequent pharyngeal phase, the tongue seals the oropharynx and the vocal cords close while the epiglottis moves to cover the laryngeal vestibule. The larynx elevates in the process and moves anteriorly. These key motions are important in protecting the airway from aspiration.
Alterations in tongue and pharynx mobility can result in altered speech, while surgical resection and/or adjuvant radiation treatment of the base of tongue may lead to dysphagia and odynophagia. Due to posttreatment changes in swallowing, it is recommended that most patients with a base of tongue tumor who have undergone surgery and/or radiation therapy be seen and evaluated by speech and language pathologists in the pretreatment and posttreatment settings.
Presentation
Dysphagia, odynophagia, foreign body sensation, referred otalgia, oral bleeding, and a neck mass are the most common clinical manifestations for base of tongue tumors. Patients may present in a delayed fashion and with advanced disease due to the vague nature of the symptoms and their relatively late appearance (which can be attributed to the limited number of free nerve endings in the base of tongue). Patients with advanced disease can also present with obstructive symptoms, including dyspnea, and an inability to tolerate secretions when the tumor has spread to surrounding structures.
A detailed and thorough base of tongue examination may be difficult to perform owing to inadequate visualization, unavailability of appropriate equipment, poor patient compliance (ie, strong gag reflex), and the submucosal presence of disease. Indirect or flexible fiberoptic laryngoscopy in the office is a useful adjunct to the physical examination.
Patients may have bilateral palpable adenopathy because of the proximity of the disease to midline and a high propensity for regional lymph node metastases.
Relevant Anatomy
The base of tongue is bound anterior-superiorly by the circumvallate papillae, posterior-inferiorly by the vallecula, and laterally by the glossopalatine sulci. However, since there is a lack of distinct anatomic boundaries, primary tumors of the base of tongue can easily spread from this oropharyngeal subsite to other areas, including the oral cavity, nasopharynx, and larynx. The base of tongue is part of Waldeyer's ring within the oropharynx and contains a rich, intricate lymphatic network. [1] Despite this, oropharyngeal tumors characteristically drain to clinical neck levels II, III, and IV, with possible spread to other regions with extensive disease. [14, 15, 16] Base of tongue tumors have a higher incidence of metastatic spread to bilateral cervical lymph nodes primarily because of the tumors' proximity to midline but also due to known contralateral lymphatic drainage. [17] A thorough understanding of lymphatic drainage patterns based on the primary tumor's size and location is critical when determining surgical and/or adjuvant treatment options. Malignancies of the base of tongue require that both sides of the neck be addressed.
The blood supply of the tongue is based off the lingual artery and has complex capillary and venous systems. Sensory and taste innervation for the base of tongue is primarily provided by the glossopharyngeal nerve, although such innervation is provided to the most posterior-inferior aspect by the internal branch of the superior laryngeal nerve. [1] Tongue musculature includes both intrinsic and extrinsic muscles, which contribute to the varied and subtle movements involved in speech, mastication, and swallowing. The muscles are served by efferent motor fibers from the hypoglossal nerve; the exception is the palatoglossus muscle, which is innervated by the vagus nerve.
Because the mucosa of the base of tongue contains squamous epithelium, minor salivary glands, and lymphoid tissue, malignant neoplasms may arise from any of these tissues.
-
An axial positron emission tomography (PET) scan shows asymmetrical hypermetabolic uptake within the left base of the tongue/tonsillar region consistent with a primary tumor. Intense hypermetabolic left cervical lymphadenopathy is also seen and is concerning for metastatic disease.
-
A sagittal computed tomography (CT) scan of the neck with contrast demonstrates a pedunculated soft tissue lesion at the left base of the tongue without invasion of the floor of the mouth or adjacent structures. The mass measures approximately 2.7 x 1.8 x 2.8 cm.
-
An axial CT scan of the neck with contrast again demonstrates a soft tissue left base of tongue lesion with slight extension into the glossotonsillar sulcus. There is also an enlarged, pathologic-appearing, left level II cervical lymph node.










