Practice Essentials
Otitis media with effusion (OME) is characterized by a nonpurulent effusion of the middle ear that may be either mucoid or serous. Symptoms usually involve hearing loss or aural fullness but typically do not involve pain or fever. In children, hearing loss is generally mild and is often detected only with an audiogram. Serous otitis media is a specific type of otitis media with effusion caused by transudate formation as a result of a rapid decrease in middle ear pressure relative to the atmospheric pressure. The fluid in this case is watery and clear. [1, 2]
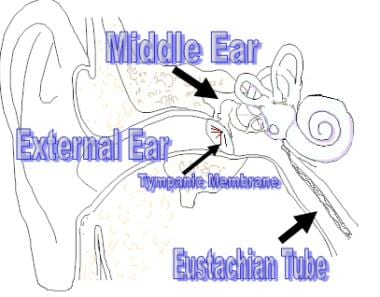
Understanding the difference between otitis media with effusion and other forms of middle ear infection is important. [3] Otitis media is a generic term defined as an inflammation of the middle ear without reference to a specific etiology or pathogenesis. Because all pneumatized spaces of the temporal bone are contiguous, inflammation of the middle ear may involve inflammation in the other 3 spaces: the mastoid, the perilabyrinthine air cells, and the petrous apex. The term otitis media is often used to describe any of a continuum of related diseases: acute otitis media (AOM), recurrent acute otitis media (RAOM), otitis media with effusion, and chronic otitis media with effusion (COME). See the image below.
Workup
Traditionally, laboratory tests have rarely been used in the workup and diagnosis of otitis media with effusion (OME) unless another process is suspected. History taking and physical examination are sensitive and specific enough to facilitate accurate diagnosis and treatment of the disease.
Computed tomography (CT) scanning is important in attempting to rule out potential complications of otitis media (eg, mastoiditis, sigmoid sinus thrombosis, erosion of bone with intracranial extension) or unusual lesions (eg, cholesteatoma). This imaging modality is particularly important in unilateral otitis media with effusion when a nasopharyngeal or eustachian tube mass must be ruled out.
Magnetic resonance imaging (MRI) is especially useful in the workup for soft-tissue masses that may be contributing to middle ear effusions (MEE) because of its superior ability to delineate borders within soft tissues and to help determine the extent of potential intracranial extension (often helpful in nasopharyngeal masses). In addition, MRI and its closely associated variants magnetic resonance venography (MRV) and magnetic resonance arteriography (MRA) demonstrate complications such as thrombosis of the intracranial sinuses very well. However, when intracranial extension is present, either from invasion from the nasopharynx or the temporal bone, CT scanning helps to define the bony anatomy more specifically and should be used in conjunction with MRI.
Tympanometry is perhaps the most useful of all tests in association with otitis media with effusion (OME). This test reveals a type B result (flat) in 43% of cases of otitis media with effusion and a type C result (negative pressure) in 47% of cases.
Tympanocentesis involves the aspiration of effusion from the middle ear. This procedure can be performed as an office procedure, even in small children, if necessary. Tympanocentesis can serve as both a therapeutic procedure and a diagnostic one. [4]
The criterion standard for documentation of a middle ear effusion is myringotomy, which has the advantage of increased exposure and better suctioning relative to tympanocentesis. [5]
Management
An otolaryngologist should be consulted whenever the primary care physician (PCP) is concerned about persistent conductive hearing loss in children, especially those with signs of language development delay.
In addition, an otolaryngologist (ENT) should be consulted if the disease is recurrent, if the appropriate medical therapies available to the primary care physician are exhausted, and/or if the criteria for surgical intervention have been met.
An allergist, audiologist, and/or a speech therapist may be consulted, when appropriate. In select cases, an immunologist may be consulted for the workup for a possible immunocompromised state.
Several investigators have reported mixed results when attempting to determine if autoinflation, compared with no intervention, improves effusion clearance rates. The ambiguity in the data may be a result of great variability in autoinflation methods and/or noncompliance in patients.
Pharmacologic management of otitis media with effusion (OME) includes administration of antimicrobial agents, steroids, antihistamines and decongestants, and mucolytics. However, an international consensus conference of the 2017 International Federation of Oto-rhino-laryngological Societies Congress recommended against the treatment of otitis media with effusion (OME) with steroids, antibiotics, decongestants, or antihistamines, citing concerns regarding side effects and cost, as well as a lack of evidence for long-term therapeutic effectiveness. [6]
Surgery has become the most widely accepted therapeutic intervention for persistent otitis media with effusion (OME), and it is clearly effective. The interventions include myringotomy with or without tube insertion, adenoidectomy, or both. Tonsillectomy has been shown to be of little benefit as a primary treatment of otitis media with effusion.
See also Otitis Media, Acute Otitis Media, Complications of Otitis Media, Chronic Suppurative Otitis Media, Emergent Management of Acute Otitis Media, and Ear Anatomy.
Pathophysiology
Otitis media with effusion (OME) can occur during the resolution of acute otitis media (AOM) once the acute inflammation has resolved. Among children who have had an episode of acute otitis media, as many as 45% have persistent effusion after 1 month, but this number decreases to 10% after 3 months.
Classic theory
Two main theories of the cause of acute otitis media exist. The classic explanation proposes that eustachian tube dysfunction is the necessary precursor. The eustachian tube has been traditionally described to provide 3 main functions: equilibration of pressure between the middle and external ears, clearance of secretions, and protection of the middle ear. Its dysfunction can be caused by any number of circumstances from anatomic blockage to inflammation secondary to allergies, upper respiratory tract infection (URTI), or trauma.
If eustachian tube dysfunction is persistent, a negative pressure develops within the middle ear from the absorption and/or diffusion of nitrogen and oxygen into the middle ear mucosal cells. If present for long enough and with appropriate magnitude, the negative pressure elicits a transudate from the mucosa, leading to the eventual accumulation of a serous, essentially sterile effusion. Because the eustachian tube is dysfunctional, the effusion becomes a sessile medium ideal for the proliferation of bacteria and resultant acute otitis media. This classic model is somewhat incorrect, as multiple studies have revealed that the same pathogenic bacteria are present in otitis media with effusion as in acute otitis media.
Newer theories
The newer models describe the primary event as inflammation of the middle ear mucosa caused by a reaction to bacteria already present in the middle ear. Indeed, Bluestone and others have shown (using radiographic evidence) that reflux up the eustachian tube is demonstrable in children prone to otitis media. [7] Furthermore, Crapko et al demonstrated the presence of pepsin in the middle ear space of 60% of children with otitis media with effusion, [8] although this reflux certainly may also occur in otherwise healthy individuals.
Similarly, in a prospective study of 129 pediatric patients with otitis media who underwent myringotomy with tympanostomy tube placement, O’Reilly et al found that ear samples from 64 patients tested positive for pepsin A, evidence that these children had aspirated gastric contents into the nasopharynx. The investigators suggested that this may in turn have initiated inflammation or exacerbated a preexisting condition. [9]
The inflammatory mediators released as a result of bacterial antigenic challenge induce the upregulation of mucin genes. The production of a mucin-rich effusion then provides an ample medium for the proliferation of bacteria and resultant acute otitis media.
Yilmaz et al published a study that documented significant changes in oxidative stress in patients with otitis media with effusion. [10] The investigators demonstrated a significantly improved but not normalized level of oxidants following the placement of ventilation tubes. However, the role of antioxidants in the treatment of otitis media with effusion has yet to be fully investigated.
Middle ear effusion
Regardless of the cause of acute otitis media, eustachian tube dysfunction is nearly universal in otitis media with effusion. As further evidence, ligation of the eustachian tube in animals invariably leads to the formation of a persistent middle ear effusion (MEE). Once the acute inflammation and bacterial infection have resolved, a failure of the middle ear clearance mechanism allows middle ear effusion to persist. Many factors have been implicated in the failure of the clearance mechanism, including ciliary dysfunction; mucosal edema; hyperviscosity of the effusion; and, possibly, an unfavorable pressure gradient.
Otitis media with effusion does not necessarily follow acute otitis media. Theories to explain the development of middle ear effusion in this case include the secretion of fluid from inflamed middle ear mucosa. This theory proposes that the middle ear mucosa is sensitized by previous exposure to bacteria, and continued antigenic challenge from occasional reflux induces the production of the effusion. Again, multiple studies have revealed that the same flora of bacteria is present in otitis media with effusion as in acute otitis media; these findings indicate that this effusion is not sterile, as was once believed.
Cleft palate
Otitis media with effusion is ubiquitous in children who have a cleft palate. The cause is simply the lack of proper insertion of the tensor veli palatini muscle in the soft palate. The muscle is, therefore, unable to open the eustachian tube on swallowing or wide mouth opening. A functional obstruction of the tube results. [11]
Etiology
The same flora found in acute otitis media can be isolated in otitis media with effusion. [12] With otitis media with effusion, the inflammatory process has clearly resolved, and the volume of bacteria has decreased. However, because of the similarity of these 2 conditions, reviewing the pathogenic organisms in acute otitis media is worthwhile.
Common pathogens
The most common bacteria in acute otitis media, in order of frequency, are Streptococcus pneumoniae, Haemophilus influenzae, and Moraxella catarrhalis. These pathogens are also the most frequent organisms associated with sinusitis and pneumonia. Together, these pathogens account for 85% of acute ear infections, as follows:
-
S pneumoniae is found in 35% of cases, and the prevalence does not seem to vary with age; the serotypes most commonly isolated, in order of frequency, are 19, 23, 6, 14, and 3
-
H influenzae is found in 20% of cases; of these cases, 25-45% involve beta-lactamase production, with a clear trend of increasing resistance
-
M catarrhalis is found in 4-13% of cases of acute otitis media, with a great frequency in winter and autumn; of these cases, 70-100% involve beta-lactamase production
Additional bacterial pathogens include Streptococcus pyogenes, Staphylococcus aureus, gram-negative enteric bacteria, and anaerobes. When an effusion is present for longer than 3 months, Pseudomonas species predominate.
In 30% of examined tympanocentesis specimens, microorganisms are not found. In a meta-analysis of results from 10 studies of tympanocentesis in acute otitis media from the early 1990s, 29 (4.4%) of 663 patients had a virus that could be isolated. In other more recent studies, viruses have been isolated in conjunction with bacteria in 15-20% of cases of acute otitis media. Respiratory syncytial virus (RSV) and influenza virus were the most frequent.
The relation between viral and bacterial infection is controversial. Because viruses have been identified as the sole infective agents in only 4-6% of middle ear aspirates obtained from children with acute otitis media, viruses may promote bacterial superinfection by impairing eustachian tube function.
The only difference with the pathogens in otitis media with effusion compared with acute otitis media is that the frequency of S pneumoniae is not as high, and H influenzae and M catarrhalis are moderately more common.
Predisposing factors
Environmental factors, age, and disruption of the eustachian tube have been associated with otitis media with effusion.
Environmental factors
Besides the actual pathogens, environmental factors have been shown in numerous epidemiologic studies to be strongly associated with increased prevalence of otitis media with effusion. These factors include bottle feeding, feeding while supine, having a sibling with otitis media, attending daycare, having allergies to common environmental entities, having a lower socioeconomic status, living in a home in which people smoke, and having a parental history of otitis media with effusion. [13, 14]
Age
Age is clearly another predisposing factor in the development of otitis media with effusion. In infants, the eustachian tube has a nearly horizontal orientation (relative to the ground) and develops the 45° angle (as in adults) after several years. In addition, the size and shape of the eustachian tube at birth, unlike those in adults, are unfavorable for ventilation of the middle ear.
Multiple studies of children in Denmark revealed that by the time children were aged 1 year, tympanograms were either type B (flat) or type C (negative pressure) in 24% of their ears. Improvement occurred in the spring and summer, whereas worsening was more common in the winter. Type B tympanograms peaked in children aged 2-4 years, and, as expected with the prevalence of otitis media with effusion, decreased in children older than 6 years.
In adults, recognizing unilateral otitis media with effusion is crucial. [15] This entity must be considered a nasopharyngeal mass until definitively proven otherwise.
Eustachian tube disruption
Disruptions in the normal opening of the eustachian tube orifice in the nasopharynx are also associated with an increased prevalence of otitis media with effusion. These commonly occur in patients who have a cleft palate and in children with Down syndrome and other disorders affecting the palate. In addition, the decreased mucociliary clearance and higher viscosity of mucus in cystic fibrosis have been hypothesized to account for a higher prevalence of otitis media with effusion in patients with these conditions.
Diet
A study by Choi et al suggested that a high-fat diet is a risk factor for otitis media with effusion in children but that body mass index category; protein, water, and sodium intake; and distribution of carbohydrate intake are not. [16]
Other
In contrast to the Choi study, however, a study by Kaya et al suggested that in children, a link exists between chronic otitis media with effusion (OME) and the presence of overweight or obesity. The report, which looked at weight-for-height percentiles in 60 children with chronic otitis media with effusion (OME) and 86 controls, aged 2-10 years, found a higher prevalence of overweight and obesity in the otitis media group, indicating that overweight and obesity may increase the risk for chronic otitis media with effusion (OME), or vice versa. [17]
A study by Walker et al found that preschool children with chronic otitis media with effusion tended to be characterized by nasal obstruction, snoring (always or often), a greater number of hours per week in daycare, frequent colds, siblings in whom tympanostomy tube placement had been performed, long labor, and early introduction of cow’s milk. However, Asian ethnicity and the existence of older siblings were associated with a lower risk of the condition. [18]
Epidemiology
In the United States, middle ear infections are the most common medical problem in infants and children of preschool age, and they are the most frequent primary diagnoses in children younger than 15 years who are examined at physicians' offices.
Clinical guidelines from a joint commission of specialties document that screening surveys of healthy children between infancy and age 5 years show a 15-40% point prevalence in middle ear effusion (MEE). Furthermore, among children examined at regular intervals for 1 year, 50-60% of child care attendees and 25% of school-aged children were found to have a middle ear effusion at some point during the examination period, with peak incidence during the winter months.
Between 84% and 93% of all children experience at least 1 episode of acute otitis media (AOM). Furthermore, approximately 80% of children have had an episode of otitis media with effusion (OME) when younger than 10 years. At any given time, 5% of children aged 2-4 years have hearing loss due to a middle ear effusion that lasts 3 months or longer. The prevalence of otitis media with effusion is highest in those aged 2 years or younger, and it sharply declines in children older than 6 years.
A 7-year study of otitis media conducted in the greater Boston area revealed the frequency of acute otitis media. In children younger than 1 year, 62% had at least 1 episode of acute otitis media, and 17% had 3 or more episodes. In children younger than 3 years, 83% had at least 1 episode of acute otitis media, and 46% had 3 or more episodes.
In another study, 12.8 million episodes of otitis media occurred in children younger than 5 years. Of children younger than 2 years, 17% had recurrent disease. Because at least 30% and as many as 45% of children with acute otitis media had otitis media with effusion after 30 days, and 10% had otitis media with effusion after 90 days, at least 3.84 million episodes of otitis media with effusion occurred the year studied; of these, 1.28 million episodes persisted at least 3 months.
Racial and sexual differences in incidence
The prevalence of otitis media with effusion is higher in Native Americans, particularly Navajo and Eskimo peoples, than in other races. The reason for the higher frequency in these populations has been attributed to a number of factors, but no findings have confirmed the most likely etiologies. No difference in prevalence rates between white and black populations exists.
Although no statistically significant difference exists between the sexes in terms of incidence or prevalence, some findings suggest that males may have a slightly higher frequency.
Prognosis
Otitis media with effusion (OME) is the leading cause of hearing loss in children. This condition is associated with delayed language development in children younger than 10 years, and the loss is usually conductive, with an average air conduction threshold of 27.5 decibels (dB), but otitis media with effusion has also been associated with sensorineural hearing loss. Both prostaglandins and leukotrienes have been found in high concentrations in middle ear effusions (MEE), and their ability to cross the round window membrane has been demonstrated. Chronic exposure to these metabolites of arachidonic acid may cause a temporary and sometimes permanent sensorineural hearing loss.
In general, the prognosis for otitis media with effusion is good. Most episodes spontaneously resolve without intervention, and many resolve undiagnosed. Still, 5% of children who are not treated surgically have persistent otitis media with effusion at 1 year. Surgical intervention significantly improves the clearance of middle ear effusion in this population, but the benefits for speech and language development as well as quality of life remain controversial.
Following spontaneous tube extrusion, 20-50% of patients will have a recurrence of otitis media with effusion, potentially requiring the replacement of pressure equalization tubes (PETs) and, in most cases, simultaneous adenoidectomy.
Complications
Because otitis media with effusion lacks the inflammation found in acute otitis media, it has few complications. As noted above, the most important complications and reasons for treatment are hearing loss and potential language development delay. Nonetheless, persistent effusion provides an exceptional environment for the proliferation of bacteria. Therefore, recurrent acute otitis media (RAOM) with its potential complications is also a threat.
The complications of the various surgical interventions are discussed in Treatment.
Patient Education
On a primary care level, ongoing education of primary care providers (PCPs) and pediatricians is important and often falls into the responsibility of the otolaryngologists (ENTs). Equally important is educating parents and teachers to be aware of the potential for delayed language development in affected children. These measures make early intervention possible if problems are noted.
Prevention
The following modifications may help decrease the frequency of otitis media with effusion (OME):
-
Avoiding secondhand smoke
-
Breastfeeding whenever possible
-
Avoiding feeding, either by breast or bottle, while completely supine
-
Avoiding exposure to a large number of children, particularly in daycare centers
-
Avoiding exposure to children who are known to be affected
Dietary and activity considerations
Breastfed babies have a lower risk of acute otitis media (AOM) and otitis media with effusion. Moreover, placing a child in the supine position while bottle feeding substantially increases the risk of otitis media with effusion, presumably because it contributes to eustachian tube reflux during swallowing.
During active otitis media with effusion, activity need not be limited. However, because of potential hearing loss, children may wish to sit closer to the teacher in their classrooms.
-
Anatomy of the external and middle ear.