Practice Essentials
A nasal septal perforation is a through-and-through defect in any portion of the cartilaginous or bony septum with no overlying mucoperichondrium or mucoperiosteum on either side. A nasal septal perforation provides direct communication between the right and left nasal cavities. [1]
Nasal septal perforations may be stratified based on size, as follows:
-
Small perforations - Diameter ≤ 0.5 cm
-
Medium perforations - Diameter between 0.5-2 cm
-
Large perforations - Diameter > 2 cm
The location and size of perforation impacts the symptoms patient’s experience.
Many nasoseptal perforations are unrecognized, though a subsection of patients experience bothersome symptoms including but not limited to crusting, recurrent epistaxis, and nasal whistling on respiration that lead patients to seek treatment.
Signs and symptoms of septal perforations
Commonly reported signs and symptoms include the following:
-
Nasal obstruction
-
Crusting
-
Epistaxis
-
Nasal discharge
-
Parosmia
-
Neuralgia
Small perforations can cause a whistling sound with inspiration. [2] Larger perforations can lead to atrophic rhinitis. Long-standing large perforations may even result in a saddle-nose deformity from a lack of dorsal nasal support producing both an aesthetic and functional problem.
Management of septal perforations
Medical therapy
Symptoms caused by septal perforations may be managed with saline nasal irrigations or regular humidification to reduce crusting. Patients who complain of pain and dryness at the perforation site often experience an improvement with antibiotic ointment or a petroleum-based ointment applied intranasally a few times a day. Although nasal hygiene and lubrication may provide some symptomatic relief, progressive enlargement of the septal perforation is a continued risk with medical therapy alone. [3]
Prosthetic use and surgical repair
Closing a nasal septal perforation can be accomplished through placement of a nasal septal prosthesis or via surgical repair.
The nasal septal prosthesis (ie, button) is the most conservative approach. It may serve as a temporary or long-term solution, especially in patients who may have a comorbid condition that precludes them from undergoing surgical treatment.
Surgical repair techniques for septal perforations can be classified broadly into several groups, from the most conservative to the most radical. These techniques include the use of local flaps, various autologous and biocompatible grafts, two-stage procedures, and free-flap repair.
Various local flaps of local endonasal mucosa have been described in the literature. Mucosal flaps may be taken from nearby healthy septum or from the inferior turbinate and pedicled posteriorly. Posteriorly based mucoperichondrial flaps have been described.
A two-stage procedure is performed when closure requires additional endonasal mucosa, usually with perforations larger than 2 cm. In the first stage, small tissue expanders are placed beneath the bilateral nasal floor mucosa, with the peripheral ports placed onto the premaxillary fossae. The second stage entails a midface degloving approach to fully expose the endonasal vault and septal perforation. Bilateral tissue expanders are removed, and posteriorly based expanded mucosal flaps are raised and medialized. The perforation is closed over an AlloDerm graft.
History of the Procedure
Treatment falls into 3 main categories:
-
Medical treatment aims to reduce symptoms rather than correct the perforation.
-
Placement of a nasal-septal prosthesis is a conservative intervention that may act as a temporary or long-term solution.
-
Surgical repair may provide a definitive solution though is accompanied by increased potential morbidity and failure.
High failure rates can be attributed to two unfavorable factors: an inadequate blood supply and a scarred host bed. Failure rates range from 60% for procedures in early studies to 18% for the best of the modern 2-stage procedures. More than 90% of small perforations can be closed reliably, whereas 70-80% of large defects can be completely closed with the newer techniques.
Although many techniques for repairing septal perforations have been described, no standardized surgical protocol has been established.
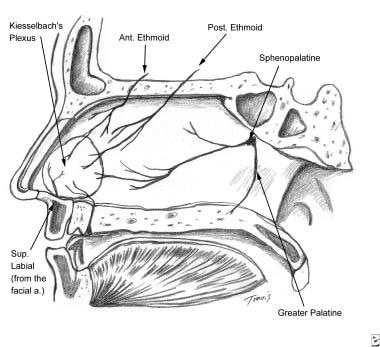
The image below depicts the blood supply to the septum.
Epidemiology
Frequency
The frequency of nasal septal perforations is correlated with the number of nasal procedures performed and history of cocaine use ingested by the nasal route. The incidence has no geographic correlation, and the condition is not clearly and directly associated with age, sex, diabetes, or smoking.
Using facial bone computed tomography (CT) scans from 3708 patients, a study by Gold et al found the prevalence of nasal septal perforation in a US urban population to be 2.05%. A history of drug abuse was the predominant risk factor, with cocaine being the most commonly used drug. [4]
A broad examination of the Swedish population revealed a 0.9% prevalence of septal perforation.
Etiology
The etiology of nasal septal perforations can be classified into the following main categories: traumatic, iatrogenic, inflammatory/malignant, infectious, and inhalant related. See the image below.
Most traumatic or iatrogenic perforations result from mucosal lacerations on corresponding sides of the septum with exposure of the underlying cartilage or a fracture of the cartilaginous septum. Cartilage relies on the overlying mucoperichondrium for its blood supply and nutrients. Defects in the mucoperichondrium cause ischemia of the underlying cartilage, resulting in breakdown and subsequent perforation. Traumatic injuries may be self-induced from nose picking or may result from facial trauma.
Iatrogenic causes include nasal surgical procedures and nasal intubation or nasogastric tube placement. Overall, prior nasal septal surgery (septoplasty) is the most common cause of septal perforations with a risk of roughly 1%. A review found that patients are not at increased risk of nasal septal perforation when undergoing septoplasty if they carry the diagnosis of allergic rhinitis. [5]
Septal hematoma, if not identified and treated early, may also result in perforation secondary to loss of cartilaginous structure, infection, and/or abscess formation.
Infectious and inflammatory etiologies, including tuberculosis, syphilis, Wegener granulomatosis, and sarcoidosis, should always be considered in the differential diagnosis.
Newly identified, bevacizumab, an anti-angiogenesis monoclonal antibody, may be associated with nasoseptal perforation. [6, 7]
Abuse of nasal inhalants is often implicated in septal perforation. Irritants including chromic or sulfuric acid fumes, glass dust, mercurials, and phosphorous have been associated.
Septal perforation is more commonly associated with cocaine abuse or, in a similar mechanism, use of vasoconstrictive nasal sprays. These patients often present with large and expanding perforations. See Pathophysiology for a more detailed explanation of the role of cocaine in nasal-septal perforation.
Pathophysiology
Nasal septal perforations result from trauma to the mucoperichondrium of the septum. Diminished blood supply can lead to cartilaginous and mucosal necrosis. After perforation occurs, the mucosal edges epithelialize, preventing closure of the defect. Symptoms arise from altered nasal laminar airflow and may be severely disturbing to the patient. Some patients may be completely asymptomatic.
The mechanism of cocaine induced nasal septal perforation is multifaceted: First, vasoconstrictive properties lead to ischemia and subsequent breakdown of the cartilage. Second, illicit cocaine contains adulterants that act as chemical irritants damaging the nasal mucosa. Third, vasoconstriction may produce a micro-aerophilic environment suitable for anaerobic infection. Chronic abuse leads to physiologic changes in the mucosa, making repairs difficult and increasing the rate of failure.
A study by Hulterström et al found that in patients with symptomatic perforation of the nasal septum, the nasal mucosa had a high prevalence of Staphylococcus aureus compared with that of controls (88% vs 13%, respectively), indicating that S aureus can sustain chronic inflammation in such patients. In addition, the S aureus strains were genetically heterogeneous in patients and controls, suggesting no association between septal perforation and a specific S aureus genotype. [8]
A study by Li et al found that in patients with nasal septal perforation, wall shear stress and heat flux were significantly higher, particularly along the posterior perforation margin, in symptomatic individuals than in asymptomatic ones. The report indicated that a wall shear stress cutoff of 0.72 Pa has an 87% sensitivity and 100% specificity in separating asymptomatic from symptomatic perforations. [9]
Presentation
Symptoms tend to be related to the size and location of the perforation. Most symptomatic perforations are large and anterior. Posterior perforations tend to be less symptomatic than others because of humidification from the nasal mucosa and turbinates. A low-grade perichondritis may persist and require long-term antibiotic treatment.
Nasal obstruction, crusting, epistaxis, nasal discharge, parosmia, and neuralgia are commonly reported symptoms. Small perforations can cause a whistling sound with inspiration. [2] Larger perforations can lead to atrophic rhinitis. Long-standing large perforations may even result in a saddle-nose deformity from a lack of dorsal nasal support producing both an aesthetic and functional problem.
Indications
Surgical repair is an elective procedure reserved for patients who seek resolution of the aforementioned symptoms.
Relevant Anatomy
The nasal septum is composed of 2 major structural components: the anterior quadrangular cartilage and the posterior bony portion, predominately consisting of the vomer and perpendicular plate of the ethmoid bone. According to data from cadaveric studies, the cartilaginous septum accounts for approximately 34% of the nasal septum. The septum is inferiorly attached to the crest of the maxillary and palatine bones by dense fibrous tissue.
The arterial supply is a rich anastomosis of 4 major blood supplies (see the image below), which is important, especially when repair with various flaps is considered. The anterior and posterior ethmoid arteries supply the septum superiorly. Branches of the facial artery supply the septum anteriorly. The sphenopalatine artery supplies the septum posteriorly, and the greater palatine artery supplies the septum inferiorly.
Contraindications
Current use of cocaine is an absolute contraindication for surgical repair. Postoperative cocaine abuse inevitably results in repeat perforation. If an obvious specific cause for perforation cannot be clearly identified or if the perforated edges do not appear well mucosalized, biopsy should be considered before repair is attempted. Further laboratory evaluation to rule out autoimmune or infectious etiologies may also be warranted. Control of autoimmune disease must precede attempt at nasal septal perforation closure. Lastly, active infection is a contraindication to repair.
-
Surgical aspects of septal perforation. Blood supply to the nasal septum.
-
Surgical aspects of septal perforation. Photo of 1- and 2-piece septal button prostheses.
-
Surgical aspects of septal perforation. Exposure of a nasal septal perforation by using the extended external rhinoplasty approach. A is the retracted columella flap, B is a cartilaginous perforation, C is a mucosal perforation, and D is mucosa elevated and reflected laterally.
-
Surgical aspects of septal perforation. Bilateral closure of mucosal flaps with an interposition graft of acellular dermal graft (AlloDerm). A is AlloDerm dermal matrix covering a septal perforation, and B is a mucosal perforation closed with interrupted sutures.
-
Surgical aspects of septal perforation. Completion of flap elevation rotation and repair of perforation. A is the middle turbinate, B is the posterior naris, C is the inferior turbinate infractured, D is the raw surface area left by flap rotation, E is a full-thickness skin graft on the floor of the nose, F is the rotated flap, and G is the anterior septal angle.
-
Surgical aspects of septal perforation. Closure of the perforation and nasal packing. A is the AlloDerm dermal graft, B is the rotated nasal floor mucosal flaps, C is the thin silicone sheeting secured to nasal mucosal flaps, D is a surgical sponge (Telfa) dressing, E is a surgical sponge (Merocel), and F is a skin graft covering the donor site.
-
Surgical aspects of septal perforation. A 1 X 3-cm tissue expander is inserted into a submucoperiosteal pocket on the nasal floor. A is the nasal septal perforation, B is the long-term expanded nasal floor mucosa (arrows), and C is the peripheral port implanted onto the maxillary fossa.
-
Surgical aspects of septal perforation. Incision used for midfacial degloving. A is the intercartilaginous incision, B is the septal perforation, C is the complete transfixion incision, D is the nasal floor sill incision, and E is the gingivobuccal incision.
-
Surgical aspects of septal perforation. Areas of dissection for midfacial degloving over the nasal dorsum, upper lateral cartilages, and premaxilla (periosteal elevator through intercartilaginous incision).
-
Surgical aspects of septal perforation. Completing midfacial degloving. A is the nasal bone, B is the upper lateral cartilages, C is the infraorbital nerve, D is the anterior septal angle, and E is soft tissue lateral to the pyriform aperture being divided by electrocautery.
-
Different Etiologies of Nasal Septal Perforations