Background
Facial aging is a multifactorial process that is especially prominent in the upper third of the face. Techniques for brow rejuvenation have evolved over the years and must be individualized for each patient. A careful analysis of the patient's sex, age, physical attributes, and expectations must be taken into account when planning rejuvenation procedures. The trend toward minimizing incisions and reducing scars has led to the development of advanced procedures in brow rejuvenation surgery.
Problem
Descent of the soft tissues overlying the skeletal supraorbital rim leads to brow ptosis, rhytide formation, dermatochalasia, and a tired and aged appearance. Some patients primarily have cosmetic concerns, while others with more severe brow ptosis experience functional visual-field impairment.
Epidemiology
Frequency
Brow ptosis is frequently observed in patients presenting for upper eyelid blepharoplasty. If overlooked, aesthetic and functional outcomes will be suboptimal.
Etiology
Many factors contribute to aging of the upper face and brow. Signs of upper facial aging clinically appear approximately at age 34-39 years. Intrinsic factors, such as skin elasticity and pigmentation or other hereditary conditions, influence the degree and rapidity of the aging process. Extrinsic factors, including gravity and other more controllable factors (eg, sun exposure, smoking), may greatly increase an individual's aging. Facial paralysis, whether idiopathic, traumatic, or iatrogenic, usually produces dramatic brow ptosis and may be unilateral or bilateral.
Pathophysiology
Brow elevator and depressor musculature is not in balance with the depressors, with the orbicularis oculi, corrugator supercilii, and procerus muscles predominating. These muscles exert their effect over the entire length of the brow. The sole brow elevator is the frontalis muscle, which is deficient laterally. This lack of lateral brow elevation in the continued presence of lateral brow depression (ie, orbicularis oculi) results in more pronounced descent of the lateral brow.
Presentation
Most patients begin to develop faint horizontal rhytides in the third decade of life. By the fourth decade, descent of the lateral brow is noticeable, and as time passes, further descent of the medial brow occurs. As the brow continues its inevitable descent, patients rely on the frontalis muscle to elevate the brow and associated upper eyelid skin out of the visual field. This leads to even deeper horizontal rhytides.
Frontalis hyperactivity must be noted prior to periorbital surgery. Further brow descent after performing upper eyelid blepharoplasty alone in the patient with unrecognized brow ptosis is not uncommon.
Indications
Each patient presenting for cosmetic or functional eyelid surgery should be evaluated for brow ptosis. Treatment of the brow should accomplish the following goals:
-
Elevate ptotic eyebrows [1]
-
Reduce redundant upper eyelid skin
-
Correct eyebrow asymmetry
-
Reduce forehead rhytides
-
Reduce glabellar rhytides
-
Reduce lateral canthal smile lines or crow's feet
-
Elevate the forehead aesthetic unit
-
Modify the hairline (if desired)
Relevant Anatomy
Brow aesthetics
The ideally proportioned forehead occupies one third of the facial height as measured from the hairline to the glabella. The brow in women should have a gently arching shape and should lie just above the orbital rim. Some debate exists as to the ideal shape, but most surgeons agree that the highest point of the brow should lie between the lateral limbus and lateral canthus. The lateral aspect of the brow is higher than the medial aspect and parallels the free margin of the lateral upper eyelid. It should end along an oblique line connecting the lateral canthus and lateral nasal ala, as depicted in the image below.
 Woman demonstrating ideal brow aesthetics. Note the gentle curving shape of the brows, which are positioned slightly above the orbital rims. The highest arching point should lie between the lateral limbus and lateral canthus. The tail of the brow lies on a line drawn between the lateral canthus and lateral nasal ala.
Woman demonstrating ideal brow aesthetics. Note the gentle curving shape of the brows, which are positioned slightly above the orbital rims. The highest arching point should lie between the lateral limbus and lateral canthus. The tail of the brow lies on a line drawn between the lateral canthus and lateral nasal ala.
Anatomy
The brow and forehead are a single contiguous anatomical structure. The forehead and scalp have 5 layers, the terms for which can be remembered by the acronym SCALP, as follows:
-
Skin
-
Subcutaneous tissue
-
Aponeurosis
-
Loose areolar tissue
-
Periosteum
The facial skin in the forehead is the thickest of the entire face and has very little subcutaneous adipose tissue. Many tenuous fibrous septa connect the underlying musculature to the forehead and brow skin. These strong attachments and the lack of subcutaneous adipose tissue account for the relative immobility of the brow and forehead skin and also contribute to early development of rhytides.
The blood supply to this area is provided by both the internal carotid and external carotid systems. The terminal branches of the external carotid (superficial temporal artery) supply the lateral aspect of the brow and forehead. The supraorbital and supratrochlear branches, fed by the internal carotid system, supply the medial forehead and scalp. The 2 vascular systems freely interconnect, providing robust blood supply to the region.
All 3 divisions of the trigeminal nerve contribute to brow and forehead sensory innervation. The first division gives rise to the supratrochlear and supraorbital nerves. Medial brow sensation is provided by the supratrochlear nerves, as depicted in the image below. The lateral brow, to the vicinity of the temporal line and posteriorly to the vertex, is supplied by the supraorbital nerves. The second division of the trigeminal nerve supplies the anterior aspect of the temporal region via the zygomaticotemporal nerve. The posterior aspect of the temporal area receives its sensory innervation from the auriculotemporal nerve, a branch of the third division of the trigeminal nerve.
The musculature of this region can be grouped into brow depressors or elevators. Brow depressors predominate and include the orbicularis oculi, corrugators, and procerus. Brow elevation is accomplished only by the frontalis muscle. The orbicularis muscle is an oval-shaped muscle originating from the medial palpebral ligament, the frontal process of the maxilla, and the nasal process of the frontal bone. It inserts into the lateral palpebral raphe, the frontalis muscle, the corrugator muscle, and the superior and inferior tarsal plates. The muscle is supplied by the temporal and zygomatic branches of the facial nerve.
Contraction of the orbicularis muscles closes the eyes, and, over time, it causes prominent crow's feet, rhytides emanating from the lateral canthus. The orbicularis muscle action also contributes to lateral brow ptosis and hooding. Brow ptosis is usually more severe laterally because this region of the brow has no corresponding elevator. The corrugator supercilii muscle, which lies deep to the frontalis and orbicularis muscle, arises from the medial orbital rim and inserts into the dermis covering the supraorbital foramen or notch, as depicted in the image below. Contraction of this muscle draws the brow inferomedially and produces the vertically oriented glabellar frown line.
The corrugators are innervated by the temporal and zygomatic nerves. The procerus muscle originates on the inferior portion of the nasal bones and inserts into the dermis above the glabella. Contraction of the procerus causes inferior descent of the medial brow and produces a horizontally oriented rhytide. The buccal branch of the facial nerve innervates the procerus.
The single elevator is the frontalis muscle. The frontalis muscle is the anterior portion of the epicranius muscle and is not attached to bone. The fibers originate from the superficial periorbital musculature (ie, corrugators, procerus, orbicularis oculi) and insert into the galea aponeurotica just anterior to the coronal suture. The frontalis muscle raises the brow and produces the horizontal wrinkles of the forehead. The muscle fibers are located laterally only to approximately the level of a vertical line drawn through the lateral canthus. The temporal branch of the facial nerve innervates this muscle.
A very important landmark of the region is the temporal fascia. The temporalis muscle is covered by a dense, tough fascia known as the deep temporal fascia. The deep temporal fascia is continuous with the periosteum of the skull at the temporal line known as the conjoint tendon. The deep temporal fascia splits into superficial and deep layers a few centimeters above the zygomatic arch. Between these 2 layers of fascia is the superficial temporal fat pad.
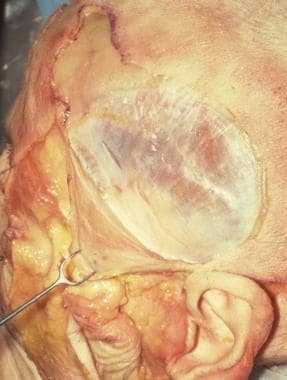
Superficial to the deep temporal fascia is another distinct fascial layer called the superficial temporal fascia or temporoparietal fascia, as depicted in the image below. It lies immediately deep to the dermis and is continuous with the galea aponeurotica above and the superficial musculoaponeurotic system below. A distinct avascular plane containing fine, wispy fascial fibers separates the temporoparietal fascia from the deep temporal fascia. The superficial temporal artery, vein, and temporal branch of the facial nerve all lie within the temporoparietal fascia. The temporal branch of the facial nerve consistently courses along a line projected from a point 0.5 cm inferior to the tragus to a point 1.5 cm above the lateral aspect of the eyebrow.
Contraindications
Browplasty has few absolute contraindications. Care must be observed when the patient has had prior upper eyelid blepharoplasty. If excessive skin was excised during the blepharoplasty, subsequent elevation of the brow to the ideal location may result in lagophthalmos and corneal exposure. This further emphasizes the need to evaluate the entire brow and periorbital area preoperatively. Browplasty with conservative upper eyelid blepharoplasty generally produces more favorable outcomes than aggressive blepharoplasty alone.
-
Woman demonstrating ideal brow aesthetics. Note the gentle curving shape of the brows, which are positioned slightly above the orbital rims. The highest arching point should lie between the lateral limbus and lateral canthus. The tail of the brow lies on a line drawn between the lateral canthus and lateral nasal ala.
-
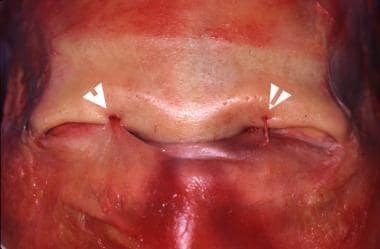
Cadaver dissection demonstrating supraorbital nerves (arrowheads); periosteum has been incised.
-
Cadaver dissection of corrugator musculature.
-
Cadaver specimen showing the temporoparietal fascia (held by a skin hook) dissected from the deep temporalis fascia; the temporalis muscle fibers are visible through the deep temporal fascia.
-
Preoperative photograph of 61-year-old man concerned with visual-field limitation in superior and lateral gaze. Note marked brow ptosis and dermatochalasis with hooding. This patient is a candidate for functional browplasty and blepharoplasty.
-
Visual-field test of 61-year-old man concerned with visual-field limitation in superior and lateral gaze. Note the dramatic improvement in visual fields when the brows and upper eyelid skin are elevated and taped (blue line, relaxed; red line, taped; green area, visual-field improvement).
-
Photograph of 61-year-old man concerned with visual-field limitation in superior and lateral gaze, two months following endoscopic browlift and upper and lower blepharoplasties. The patient's visual-field complaints resolved with surgery.
-
Preoperative photo of a 59-year-old woman prior to an endoscopic browlift, lower lid transconjunctival blepharoplasty, rhytidectomy, and carbon dioxide laser resurfacing.
-
Postoperative photo of a 59-year-old woman six months after an endoscopic browlift, lower lid transconjunctival blepharoplasty, rhytidectomy, and carbon dioxide laser resurfacing.
-
A: Brow and facial asymmetry resulting from left idiopathic facial nerve paralysis. B: Four-month postoperative view showing improved brow symmetry following trichophytic browplasty. Plication of the left facial superficial musculoaponeurotic system and placement of a facial sling were performed simultaneously.
-
Reverse beveling of the trichophytic incision encourages hair growth through the incision.
-
A: Trichophytic frontal incision. B: Subgaleal dissection of the flap is quick and relatively bloodless. Arrowheads denote supraorbital nerves that should be preserved.
-
Early postoperative view of trichophytic incision. Reverse beveling of the incision at the time of surgery promotes hair growth through the incision.
-
A 76-year-old man with left unilateral facial paresis. Note the marked brow ptosis, absence of horizontal forehead rhytides, and lower eyelid paralytic ectropion. This patient is an ideal candidate for midforehead browlift, gold weight placement, and ectropion repair.
-
A: Preoperative view of a 52-year-old woman who desires browplasty. The patient did not want sedation or general anesthesia. A midforehead browlift was performed with local anesthesia. The authors usually reserve the midforehead browlift for men with deep horizontal forehead rhytides. B: Three months status post midforehead browlift. Note the well-healed forehead incisions. Dermabrasion, although not used in this patient, may improve scar camouflage.
-
A: Elderly patient with paralytic brow ptosis on right (note hyperactive left frontalis muscle). B: Early postoperative result demonstrating improved brow symmetry. The left frontalis muscle is no longer overcompensating. C: Staggered fusiform incisions and proposed site of suspension sutures. D: orbicularis oculi fibers identified prior to brow suspension.
-
Preoperative frontal view of a patient with brow ptosis and dermatochalasis prior to endoscopic browlift and lower lid blepharoplasties.
-
Four-month postoperative view of a patient with brow ptosis and dermatochalasis prior to endoscopic browlift and lower lid blepharoplasties. Note mild elevation in hairline that is invariably observed following endoscopic and coronal browlift procedures. The patient was counseled about the hairline change preoperatively.
-
This is a 50-year-old woman prior to endoscopic browlift, carbon dioxide laser resurfacing, and botulinum toxin injection of periorbital rhytides (preoperatively).
-
Six-month postoperative view of a 50-year-old woman after endoscopic browlift, carbon dioxide laser resurfacing, and botulinum toxin injection of periorbital rhytides.
-
Endoscopic view of right supraorbital neurovascular bundle. Note the relatively bloodless subperiosteal dissection plane.
-
Endoscopic view of right supraorbital nerve following periosteal release.
-
Bulky dressing seen immediately upon completion of trichophytic browlift.