Structure
The soft tissue envelope of the cranial vault is called the scalp. The scalp extends from the external occipital protuberance and superior nuchal lines to the supraorbital margins. The scalp consists of 5 layers (seen in the image below): the skin, connective tissue, epicranial aponeurosis, loose areolar tissue, and pericranium. The first 3 layers are bound together as a single unit. This single unit can move along the loose areolar tissue over the pericranium, which is adherent to the calvaria. [1, 2, 3, 4]
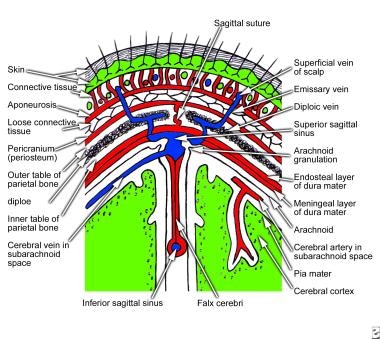 Coronal section of scalp that shows layers of the scalp (From Snell RS, Clinical Anatomy for Medical Students, 5th ed)
Coronal section of scalp that shows layers of the scalp (From Snell RS, Clinical Anatomy for Medical Students, 5th ed)
Skin
The skin of the scalp is thick and hair bearing and contains numerous sebaceous glands. As a result, the scalp is a common site for sebaceous cysts.
Connective tissue (superficial fascia)
The superficial fascia is a fibrofatty layer that connects skin to the underlying aponeurosis of the occipitofrontalis muscle and provides a passageway for nerves and blood vessels. Blood vessels are attached to this fibrous connective tissue. If the vessels are cut, this attachment prevents vasospasm, which could lead to profuse bleeding after injury.
Epicranial aponeurosis (galea aponeurotica)
The epicranial aponeurosis is a thin, tendinous structure that provides an insertion site for the occipitofrontalis muscle. Posterolaterally, the epicranial aponeurosis attachment extends from the superior nuchal line to the superior temporal line. Laterally, the epicranial aponeurosis continues as the temporal fascia. Anteriorly, the subaponeurotic space extends to the upper eyelids due to the lack of a bony insertion. This loose areolar tissue provides a potential subaponeurotic space that allows fluids and blood to pass from the scalp to the upper eyelids.
Loose areolar tissue
Areolar tissue loosely connects the epicranial aponeurosis to the pericranium and allows the superficial 3 layers of the scalp to move over the pericranium. Scalp flaps are elevated along a relatively avascular plane in craniofacial and neurosurgical procedures. However, certain emissary veins traverse this layer, which connects the scalp veins to the diploic veins and intracranial venous sinuses.
Pericranium
The pericranium is the periosteum of the skull bones. Along the suture lines, the pericranium becomes continuous with the endosteum. A subperiosteal hematoma, therefore, forms in the shape of the skull bones.
Occipitofrontalis muscle
The occipitofrontalis muscle consists of 2 occipital bellies and 2 frontal bellies. The occipital bellies arise from the superior nuchal lines on the occipital bone. The frontal bellies originate from the skin and superficial fascia of the upper eyelids. The occipital and frontal bellies insert into the epicranial aponeurosis.
Each occipital belly is innervated by the posterior auricular branch of the facial nerve, and each frontal belly is innervated by the frontal branch of the facial nerve. The frontal bellies can raise the eyebrows.
Nerve Supply
Sensory supply
The following 6 sensory nerve branches of either the trigeminal nerve or the cervical nerve supply the scalp (see the image below):
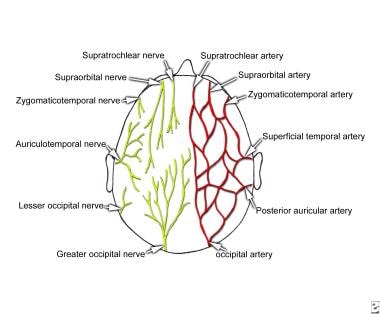 Sensory innervation and arterial supply of the scalp (From Snell RS, Clinical Anatomy for Medical Students, 5th ed)
Sensory innervation and arterial supply of the scalp (From Snell RS, Clinical Anatomy for Medical Students, 5th ed)
See the list below:
-
Supratrochlear nerve - A branch of the ophthalmic division of the trigeminal nerve; this nerve supplies the scalp in the medial plane at the frontal region, up to the vertex
-
Supraorbital nerve - Also a branch of the ophthalmic division of the trigeminal nerve; this nerve supplies the scalp at the front, lateral to the supratrochlear nerve distribution, up to the vertex
-
Zygomaticotemporal nerve - A branch of the maxillary division of the trigeminal nerve; it supplies the scalp over the temple region
-
Auriculotemporal nerve - A branch of the mandibular division of the trigeminal nerve; it supplies the skin over the temporal region of the scalp
-
Lesser occipital nerve - A branch of the cervical plexus (C2); it supplies the scalp over the lateral occipital region
-
Greater occipital nerve - A branch of the posterior ramus of the second cervical nerve; it supplies the scalp in the median plane at the occipital region, up to the vertex
Motor supply
The frontal branch of the facial nerve supplies the frontal bellies of the occipitofrontalis muscle, and the auricular branch of the facial nerve supplies the occipital bellies of the muscle.
Arterial Supply
The scalp has a rich vascular supply. The blood vessels traverse the connective tissue layer, which receives vascular contribution from the internal and external carotid arteries. The blood vessels anastomose freely in the scalp. From the midline anteriorly, the arteries present as follows:
-
Supratrochlear artery
-
Supraorbital artery
-
Superficial temporal artery
-
Posterior auricular artery
-
Occipital artery
See the image below.
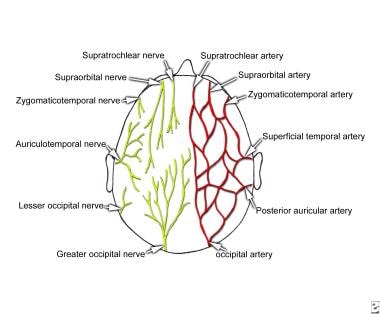 Sensory innervation and arterial supply of the scalp (From Snell RS, Clinical Anatomy for Medical Students, 5th ed)
Sensory innervation and arterial supply of the scalp (From Snell RS, Clinical Anatomy for Medical Students, 5th ed)
The supratrochlear and supraorbital arteries are 2 branches of the ophthalmic artery, which, in turn, is a branch of the internal carotid artery. These arteries accompany the corresponding nerves.
The superficial temporal artery is a terminal branch of the external carotid artery that ascends in front of the auricle. This artery, which supplies the scalp over the temporal region, travels with the auriculotemporal nerve and divides into anterior and posterior branches.
The posterior auricular artery is a branch of the external carotid artery that ascends posterior to the auricle. The occipital artery is a branch of the external carotid artery; it is accompanied by the greater occipital nerve.
Venous and Lymphatic Drainage
The veins of the scalp freely anastomose with one another and are connected to the diploic veins of the skull bones and the intracranial dural sinuses through several emissary veins. The emissary veins are valveless. The scalp veins, which are as follows, accompany the arteries and have similar names (see the image below):
-
Supratrochlear and supraorbital veins - Drain the anterior region of the scalp; these 2 veins unite to form the angular vein at the medial angle region of the eye and continue further as the facial vein
-
Superficial temporal vein - Descends in front of the auricle and enters the parotid gland; it joins the maxillary vein to form the retromandibular vein, the anterior division of which unites with the facial vein to form the common facial vein, which then drains into the internal jugular vein
-
Posterior auricular vein - Joins the posterior division of the retromandibular vein to form the external jugular vein
-
The occipital vein - Terminates in the suboccipital venous plexus, which lies beneath the floor of the upper part of the posterior triangle
Lymphatic drainage
The part of the scalp that is anterior to the auricles is drained to the parotid, submandibular, and deep cervical lymph nodes. The posterior part of the scalp is drained to the posterior auricular (mastoid) and occipital lymph nodes.
Applied Anatomy
Wounds in the scalp bleed profusely, because the fibrous fascia prevents vasoconstriction. However, wounds superficial to the aponeurosis gap much less than do wounds that cut through it, because aponeurosis holds the skin tight.
During a difficult birth, bleeding may occur between the neonate's pericranium and calvaria, usually over 1 parietal bone, because of a rupture of multiple minute periosteal arteries. The resulting collection of blood several hours after birth is known as cephalohematoma.
The emissary veins do not have valves and open in the loose areolar tissue; therefore, infection can be transmitted from the scalp to the cranial cavity. The layer of loose areolar tissue is known as the dangerous area of the scalp.
Metastatic spread of malignant lesions in front of the auricle is to the parotid and cervical groups of lymph nodes. The posterior part of the scalp is drained to the occipital and posterior auricular groups of lymph nodes.
Anastomosis exists at the medial angle of the eye, between the facial branch of the external carotid artery and the cutaneous branch of the internal carotid artery. During old age, if the internal carotid artery undergoes atherosclerotic changes, the intracranial structures can receive blood from the connection of the facial artery to the dorsal nasal branch of the ophthalmic artery.
Because it contains numerous sebaceous glands, the scalp is one of the most common sites for sebaceous cysts.
-
Coronal section of scalp that shows layers of the scalp (From Snell RS, Clinical Anatomy for Medical Students, 5th ed)
-
Sensory innervation and arterial supply of the scalp (From Snell RS, Clinical Anatomy for Medical Students, 5th ed)