Overview
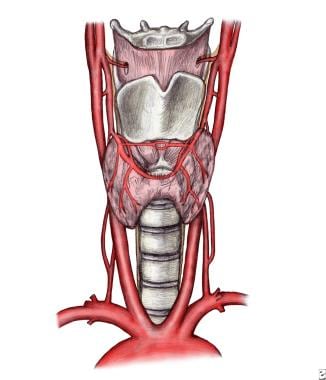
The thyroid is a highly vascular, brownish-red gland located anteriorly in the lower neck, extending from the level of the fifth cervical vertebra down to the first thoracic. The gland varies from an H to a U shape and is formed by 2 elongated lateral lobes with superior and inferior poles connected by a median isthmus, with an average height of 12-15 mm, overlying the second to fourth tracheal rings. (See the image below.) The isthmus is encountered during routine tracheotomy and must be retracted (superiorly or inferiorly) or divided. Occasionally, the isthmus is absent, and the gland exists as 2 distinct lobes. The video below depicts an ultrasonographic view of the right lobe of the thyroid gland. [1, 2]
Each lobe is 50-60 mm long, with the superior poles diverging laterally at the level of the oblique lines on the laminae of the thyroid cartilage. (The video below depicts an ultrasonographic view of the right lobe of the thyroid gland.) The lower poles diverge laterally at the level of the fifth tracheal cartilage. Although thyroid weight varies, it averages 25-30 g in adults (it is slightly heavier in women). The gland enlarges during menstruation and pregnancy.
A conical pyramidal lobe often ascends from the isthmus or the adjacent part of either lobe (more often the left) toward the hyoid bone, to which it may be attached by a fibrous or fibromuscular band, the levator of the thyroid gland. Remnants of the thyroglossal duct may persist as accessory nodules or cysts of thyroid tissue between the isthmus and the foramen caecum of the tongue base. Usually, 2 pairs of parathyroid glands lie in proximity to the thyroid gland. (See also Embryology of the Thyroid and Parathyroids.)
Innervation of the thyroid
Principal innervation of the thyroid gland derives from the autonomic nervous system. Parasympathetic fibers come from the vagus nerves, and sympathetic fibers are distributed from the superior, middle, and inferior ganglia of the sympathetic trunk. These small nerves enter the gland along with the blood vessels. Autonomic nervous regulation of the glandular secretion is not clearly understood, but most of the effect is postulated to be on blood vessels, hence the perfusion rates of the glands.
Structure
Under the middle layer of deep cervical fascia, the thyroid has an inner true capsule, which is thin and adheres closely to the gland. Extensions of this capsule within the substance of the gland form numerous septae, which divide it into lobes and lobules. The lobules are composed of follicles, the structural units of the gland, which consist of a layer of simple epithelium enclosing a colloid-filled cavity (see the image below).
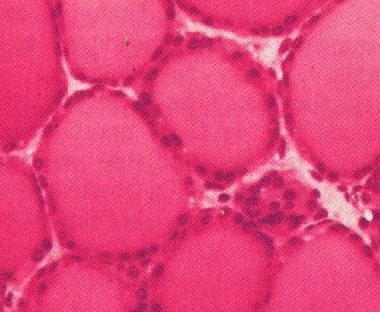 Follicles of the thyroid gland, consisting of a layer of simple epithelium enclosing a colloid-filled cavity.
Follicles of the thyroid gland, consisting of a layer of simple epithelium enclosing a colloid-filled cavity.
This colloid (pink on hematoxylin and eosin [H&E] stain) contains an iodinated glycoprotein, iodothyroglobulin, a precursor of thyroid hormones. Follicles vary in size, depending upon the degree of distention, and they are surrounded by dense plexuses of fenestrated capillaries, lymphatic vessels, and sympathetic nerves.
Epithelial cells are of 2 types: principal cells (ie, follicular) and parafollicular cells (ie, C, clear, light cells). Principal cells are responsible for formation of the colloid (iodothyroglobulin), whereas parafollicular cells produce the hormone calcitonin, a protein central to calcium homeostasis. Parafollicular cells lie adjacent to the follicles within the basal lamina.
Fascia and Ligament
The thyroid gland is ensheathed by the visceral fascia, a division of the middle layer of deep cervical fascia, which attaches it firmly to the laryngoskeleton. The anterior suspensory ligament extends from the superior-medial aspect of each thyroid lobe to the cricoid and thyroid cartilage. The posteromedial aspect of the gland is attached to the side of the cricoid cartilage, first and second tracheal ring, by the posterior suspensory ligament (ie, Berry ligament). This firm attachment of the gland to the laryngoskeleton is responsible for movement of the thyroid gland and related structures during swallowing.
On its way to the larynx, the recurrent laryngeal nerve usually passes deep to the Berry ligament or between the main ligament and its lateral leaf. Deep to the ligament, but lateral to the nerve, is a posteromedial portion of the thyroid lobe, which may be overlooked during thyroidectomy.
Strap Muscles
The lateral surface of the thyroid is covered by the sternothyroid muscle, and its attachment to the oblique line of the thyroid cartilage prevents the superior pole from extending superiorly under the thyrohyoid muscle. More anteriorly are the sternohyoid and superior belly of the omohyoid muscle, overlapped inferiorly by the anterior border of the sternocleidomastoid muscle. The sternohyoid and sternothyroid muscles are joined in the midline by an avascular fascia that must be incised to retract the strap muscle laterally in order to access the thyroid gland during thyroidectomy. If strap muscles are to be transected for better exposure, do so high in the neck, because the motor nerve supply from the ansa cervicalis enters these muscles inferiorly.
Vascular Anatomy and Laryngeal Innervation
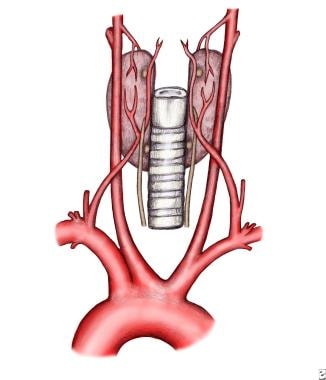
The arterial supply to the thyroid gland comes from the superior and inferior thyroid arteries and, occasionally, from the thyroidea ima. These arteries have abundant collateral anastomoses with each other, ipsilaterally and contralaterally. The thyroid ima is a single vessel that, when present, originates from the aortic arch or the innominate artery and enters the thyroid gland at the inferior border of the isthmus. (See the image below.)
Superior thyroid artery and superior laryngeal nerve
The superior thyroid artery is the first anterior branch of the external carotid artery. In rare cases, it may arise from the common carotid artery just before its bifurcation. The superior thyroid artery descends laterally to the larynx under the cover of the omohyoid and sternohyoid muscles. The artery runs superficially on the anterior border of the lateral lobe, sending a branch deep into the gland before curving toward the isthmus, where it anastomoses with the contralateral artery.
Cephalad to the superior pole, the external branch of the superior laryngeal nerve runs with the superior thyroid artery before turning medially to supply the cricothyroid muscle. High ligation of the superior thyroid artery during thyroidectomy places this nerve at risk of inadvertent injury, which would produce dysphonia by altering pitch regulation. The cricothyroid artery, a potentially bothersome branch of the superior thyroid artery, runs cephalad to the upper pole and runs toward the midline on the cricothyroid ligament. This vessel can be lacerated during emergent cricothyroidotomy. [3]
Inferior thyroid artery and recurrent laryngeal nerve
The inferior thyroid artery arises from the thyrocervical trunk, a branch of the subclavian artery. It ascends vertically and then curves medially to enter the tracheoesophageal groove in a plane posterior to the carotid sheath. Most of its branches penetrate the posterior aspect of the lateral lobe, as shown below.
The inferior thyroid artery has a variable branching pattern and is closely associated with the recurrent laryngeal nerve (seen in the image below). The latter also ascends in the tracheoesophageal groove and enters the larynx between the inferior cornu of the thyroid cartilage and the arch of the cricoid. The recurrent laryngeal nerve can be found after it emerges from the superior thoracic outlet, in a triangle bounded laterally by the common carotid artery, medially by the trachea, and superiorly by the thyroid lobe.
The relationship between the nerve and the inferior thyroid artery is highly variable, as demonstrated by the classic work of Reed, who in 1943 described 28 variations in this relationship. The nerve can be found deep to the inferior thyroid artery (40%), superficially (20%), or between branches of the artery (35%). [4] Significantly, the relationship between nerve and artery on one side of the neck is similar to that found on the other side in only 17% of the population. Furthermore, at the level of the inferior thyroid artery, branches of the recurrent laryngeal nerve that are extralaryngeal may be present (5%). Preservation of all of those branches is important during thyroidectomy.
Another hint to the location of the recurrent laryngeal nerve is the Zuckerkandl tubercle, an extension of the thyroid, which is close to the Berry ligament. [5] On rare occasions, the recurrent laryngeal nerve may pass directly from the vagus to the larynx, close to the superior thyroid vessels. This formation is nearly always observed on the right side and is associated with a retroesophageal subclavian artery. However, the formation can occur on the left side in cases of transposition of the great vessels.
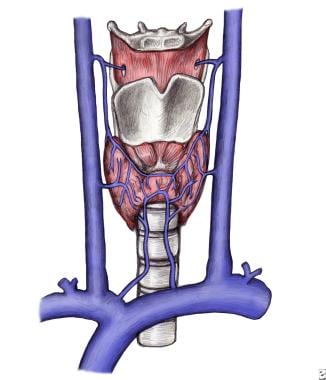
Venous Drainage and Lymphatics
Three pairs of veins provide venous drainage for the thyroid gland (see the image below). The superior thyroid vein ascends along the superior thyroid artery and becomes a tributary of the internal jugular vein. The middle thyroid vein follows a direct course laterally to the internal jugular vein. The inferior thyroid veins follow different paths on each side. The right passes anterior to the innominate artery to the right brachiocephalic vein or anterior to the trachea to the left brachiocephalic vein. On the left side, drainage is to the left brachiocephalic vein. Occasionally, both inferior veins form a common trunk called the thyroid ima vein, which empties into the left brachiocephalic vein.
Lymphatic drainage of the thyroid gland is extensive and flows multidirectionally. Immediate lymphatic drainage courses to the periglandular nodes; to the prelaryngeal (Delphian), pretracheal, and paratracheal nodes along the recurrent laryngeal nerve; and then to mediastinal lymph nodes. Regional metastases of thyroid carcinoma can also be found laterally, higher in the neck along the internal jugular vein. This can be explained by tumor invasion of the pretracheal and paratracheal nodes causing an obstruction of normal lymph flow.
-
Thyroid gland, anterior and lateral views.
-
Follicles of the thyroid gland, consisting of a layer of simple epithelium enclosing a colloid-filled cavity.
-
Distribution of thyroid arteries with associated laryngeal nerve, anterior view.
-
Distribution of thyroid arteries with associated laryngeal nerve, posterior view.
-
Distribution of thyroid veins.
-
Sonogram of a normal right lobe of the thyroid gland. Video courtesy of David L Francis, MD.