Practice Essentials
In 1979, McCabe first described a cohort of patients with idiopathic, rapidly progressive bilateral sensorineural hearing loss (SNHL). These patients' hearing improved after treatment with corticosteroids, thereby suggesting an autoimmune pathogenesis. The hallmark of this clinically diagnosed condition is the presence of a rapidly progressive, often fluctuating, bilateral SNHL over a period of weeks to months. The progression of hearing loss is too rapid to be diagnostic for presbycusis and too slow to conclude a diagnosis of sudden SNHL. Vestibular symptoms, such as true vertigo, generalized imbalance, and ataxia, may be present. [1]
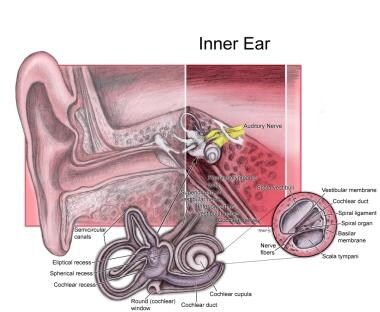
See the image below.
Signs and symptoms of autoimmune disease of the inner ear
The hallmark of immune-mediated inner ear disease is SNHL, which usually is bilateral and occurs rapidly over weeks to months.
Approximately 50% of patients complain of vestibular symptoms typical of Ménière disease. Vestibular symptoms can include disequilibrium, ataxia, motion intolerance, positional vertigo, and episodic vertigo.
As many as 25-50% of patients also have symptoms of tinnitus and aural fullness, which can fluctuate in severity.
Coexisting systemic autoimmune disease occurs in 15-30% of patients. Diagnoses include rheumatoid arthritis, ulcerative colitis, systemic lupus erythematosus, and polyarteritis nodosa.
Workup in autoimmune disease of the inner ear
Antigen-nonspecific tests are useful in routine screening for evidence of systemic immunologic dysfunction yet specifically are not known to correlate with a diagnosis of immune-mediated inner ear disease. Antigen-nonspecific tests are as follows:
-
Levels of circulating immune complexes
-
Complement levels (C3, C4)
-
Antinuclear antibody levels
-
Rheumatoid factor
-
Acute phase reactants - Erythrocyte sedimentation rate, C-reactive protein
Antigen-specific tests are as follows:
-
Migration inhibition assay
-
Lymphocyte transformation test (LTT)
-
Western blot analysis for antibodies to inner ear antigen
Management of autoimmune disease of the inner ear
Medical care
A key feature of immune-mediated inner ear disease is a positive response to immunosuppressive therapy (ie, corticosteroids) in the form of improved hearing. [2]
No standardized regimens for corticosteroid therapy exist, yet many recommend a trial of high-dose prednisone (1 mg/kg/d) for 1 month, followed by a slow taper over several weeks to a maintenance dose of 10-20 mg/d or every other day.
Cytotoxic drugs generally are used for steroid-intolerant patients or those who fail to demonstrate a continued response to steroid therapy.
Surgical care
Surgery generally is not appropriate. However, intratympanic therapy performed under local anesthesia has been found to be beneficial for some patients with immune-mediated inner ear disease.
Intratympanic drug delivery methods include the following:
-
Passive intratympanic delivery
-
Biodegradable polymer intratympanic delivery
-
Hydrogel-based intratympanic delivery
-
Nanoparticle delivery
-
Active intratympanic drug delivery
-
Round window microcatheter
-
Silverstein MicroWick
-
Preclinical Alzet osmotic pump
-
Other systems
Intracochlear drug delivery methods include the following:
-
Syringe delivery
-
Direct injection
-
Syringe pump delivery
-
Osmotic pump delivery
-
Cochlear prosthesis–based delivery
-
Other delivery devices
Pathophysiology
The term autoimmune inner ear disease (AIED) implies a direct attack of the immune system upon an endogenous inner ear antigen. Most of the evidence linking the immune system to cochleovestibular dysfunction is indirect; therefore, immune-mediated inner ear disease may be a preferred term. AIED is a clinical diagnosis based on its distinct clinical course, immune test results, and treatment response. The most important diagnostic finding is improvement in hearing observed with a trial of immunosuppressants. [3, 4, 5, 6]
Specific criteria for idiopathic progressive bilateral sensorineural hearing loss (IPBSNHL) include bilateral SNHL of at least 30 dB at any frequency with progression in at least one ear, defined as a threshold shift that is greater than 15 dB at any frequency or 10 dB at 2 or more consecutive frequencies or a significant change in discrimination score. This definition excludes patients with sudden SNHL occurring in less than 24 hours, which more likely is due to a microvascular or viral etiology.
A certain subset of patients with presumed Ménière disease (idiopathic endolymphatic hydrops) actually may have Ménière syndrome, in which the underlying pathophysiology is immune mediated. Typically, Ménière disease is initially diagnosed in these patients; however, fluctuating hearing loss in the contralateral ear develops later. This change may prompt a workup for AIED. Hughes et al found that approximately one half of their patients with AIED have manifestations of autoimmune Ménière syndrome. [7, 8]
Epidemiology
Frequency
United States
Because the existence of autoimmune inner ear disease (AIED) has been recognized only since 1979, incidence is difficult to determine. Recent studies in the literature from large referral centers are based on relatively small sample sizes of patients who fit the criteria for diagnosis of AIED. As diagnostic tests for the condition become more specific and more is known about AIED, more patients will be identified who have an autoimmune basis for inner ear symptoms.
Sex
The condition has been suggested to be more common in female patients who may or may not have concomitant systemic autoimmune disease than in male patients.
Age
In most patients, initial onset of symptoms occurs at age 20-50 years. Cases in pediatric patients are uncommon. [9]
-
Inner ear.