Practice Essentials
Myringitis, or inflammation of the tympanic membrane (TM), may be accompanied by hearing impairment and a sensation of congestion and earache. After 3 weeks, acute myringitis becomes subacute and, within 3 months, chronic.
The extremely thin and delicate TM is the first component of the middle ear conductive system. The TM is easily traumatized, and diseases of the TM deprive patients of their ability to work and to enjoy life.
The TM lies across the end of the external auditory canal (EAC) and looks like a flattened cone with its apex pointed inward, as seen in the image below. The diameter of the TM is about 8-10 millimeters. Its outer surface is slightly concave.
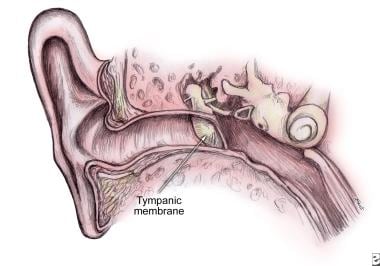 Tympanic membrane (TM) as continuation of the upper wall of external auditory canal (EAC) with angle of incline up to 45 degrees on the border between middle ear and the EAC.
Tympanic membrane (TM) as continuation of the upper wall of external auditory canal (EAC) with angle of incline up to 45 degrees on the border between middle ear and the EAC.
The edge of the membrane is thickened and attached to a groove in an incomplete ring of bone, the tympanic annulus, which almost encircles it and holds the membrane in place as seen in the image below.
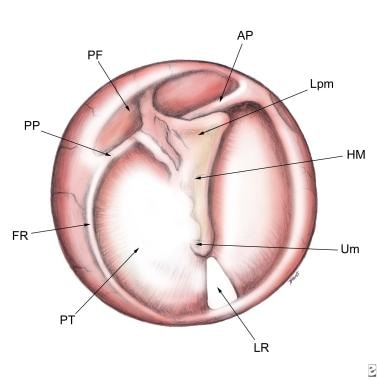 Normal tympanic membrane. Pars tensa (PT), pars flaccida (PF), light reflex (LR), fibrous ring (FR), umbo (Um), handle of malleus (HM), lateral process of malleus (Lpm), anterior plica (AP), posterior plica (PP).
Normal tympanic membrane. Pars tensa (PT), pars flaccida (PF), light reflex (LR), fibrous ring (FR), umbo (Um), handle of malleus (HM), lateral process of malleus (Lpm), anterior plica (AP), posterior plica (PP).
In newborns, the angle of incline of the TM is more than 30° relative to the horizontal plane. In addition, the TM in newborns is thicker than in adults; consequently, in the newborn, examining the TM is sometimes difficult.
The uppermost small area of the membrane, where the ring is open, is under no tension; this part is known as the pars flaccida. The majority of the membrane is tightly stretched; this is called the pars tensa. The loose part of the TM, or the pars flaccida, borders on the pars tensa from above and is considerably smaller, about one-eighth the size of the pars tensa. See the image below.
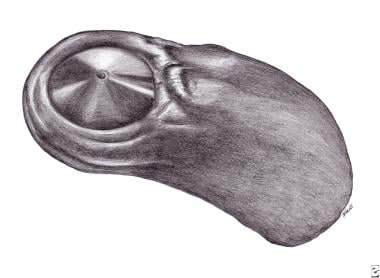 Mirror display of a tympanic membrane surface on the polymeric masc from external acoustical canal of healthy man. Masc of tympanic membrane surface (MtmS).
Mirror display of a tympanic membrane surface on the polymeric masc from external acoustical canal of healthy man. Masc of tympanic membrane surface (MtmS).
The physiologic function of the TM involves conduction of sound to the middle ear through a system of small bones, the ossicles. The surface of the TM is approximately 25 times larger than that of the stapes footplate, with the resulting amplification of sound to 45 decibels, or 27 times ambient volume levels. At the same time, the TM forms a safe shield with the round window of the labyrinth against direct sound waves. This window is necessary for movement of the liquid in the cochlea, providing for transmission of the sound to the acoustic receptors in the organ of Corti. In addition, the TM protects the gentle mucosa of the middle ear from the external environment.
Signs and symptoms of myringitis
Generally, the patient presents with a 2- to 3-day history of ear congestion and mild hearing loss. Sensations of heaviness and slight pain in the ear are common. Sometimes an itch is present in the EAC, or discharge from it is noted.
Workup in myringitis
Cultures may be obtained from middle ear fluid. Imaging studies that can be performed include the following:
-
Otomicroscopy with microscope or otoendoscopy with imaging display
-
Pneumatic otoscopy - Provides information on the appearance and mobility of the TM and is the preferred method for diagnosis
-
High-resolution computed tomography (CT) scanning of the temporal bones
-
Magnetic resonance imaging (MRI) - Useful for the evaluation of intracranial complications from otitis, but otherwise this modality tends to overestimate middle ear inflammatory processes
-
Acoustic otoscopy - A method to examine the TM using concurrent otoscopy and tympanometry; it is especially useful for children
Additional tests include the following:
-
Pure tone and speech audiometry - The shape of the audiogram for an individual with hearing loss can provide the otologist or audiologist with important information for determining the nature and cause of the hearing defect; the audiogram configuration of air conduction hearing loss can be used as an additional test for diagnosis of myringitis
-
Tympanometry - Tympanometry can provide evidence of fluid behind the eardrum, while multifrequency tympanometry has become an accepted objective method for determining the status of the middle ear, especially in regard to diagnosis of effusion
-
Infrared emission detection tympanic thermometry
Management of myringitis
Seek emergency department or primary care when a patient presents with acute myringitis, suspected otitis media, external otitis, or foreign bodies in the ear. Analgesics, anti-inflammatory medications, antipruritics, and antihistamines may be prescribed.
In case of suppurative complications, perforated TM, or suspicion of mastoiditis, consultation with an otolaryngology (ENT) specialist is imperative.
A useful method of myringoplasty (surgical closure of a TM perforation), described by Heermann, uses a cartilaginous framework. The TM is supported by the cartilaginous palisade without affecting mobility.
Pathophysiology
Regarding diseases of the TM, discussion of pathophysiology includes the concrete causes, mechanisms, and common regularities of source, development, and termination of myringitis.
Myringitises can develop as self-maintained primary disease of the TM (primary myringitis) or as an effect of an inflammatory process of adjacent tissues of the external or middle ear (secondary myringitis). The etiology and pathogenesis of primary myringitis and secondary myringitis are significantly different, and they require different treatments. Therefore, they should be considered separately.
Etiology of primary myringitis
See the list below:
-
Acute myringitis can occur because of direct trauma to the TM through penetration by a foreign body.
-
Primary myringitis may also be caused by unsuccessful removal of a foreign body, such as a live insect, or it may occur during self-cleaning of the ear.
-
An explosion, a change in the pressure in an airplane cabin, a blow to the ear with the palm, or even a kiss in the ear can cause trauma to the TM.
-
Acute bullous myringitis can be the consequence of a bacterial infection such as Streptococcus pneumoniae or a viral infection such as influenza, herpes zoster, or others. [1]
-
Acute hemorrhagic myringitis can also be the consequence of a bacterial or a viral infection. [2]
-
Fungal myringitis can be the consequence of a fungal infection of the TM's epidermis.
-
Eczematous myringitis can occur in cases of dermal eczema of the TM's epidermis.
-
Myringitis granulosa occurs when the TM is covered with granulation tissue. The causes of this destruction of the TM's epidermis are rarely clear, except when a similar case is demonstrated during a myringoplasty, when the epidermis perishes, or when the mucosa, expanding from a tympanic membrane perforation, erases an epidermis.
Etiology of secondary myringitis
See the list below:
-
Acute myringitis with acute otitis media
The TM is involved in the initial stage of acute otitis media (AOM), the stage when negative pressure is formed in the middle ear space.
During this time, the handle of the malleus, the lateral process of the malleus, and the TM bulge outward. The pars flaccida is also noticeably affected.
With the appearance of fluid in the middle ear, these phenomena disappear from the surface of the TM, so observing the fluid is possible.
The inflammatory process of an upper respiratory tract infection affects the TM in the form of myringitis. The TM becomes red and thickened, and the light reflex disappears.
Increased inflammation in the middle ear results in bulging of the TM, with possible perforation. This is accompanied by intense earache and by typical clinical manifestations of AOM.
-
Acute myringitis with acute otitis externa
Acute myringitis can occur in cases of posttraumatic acute otitis externa.
Myringitis can be the consequence of bacterial acute otitis externa.
Myringitis can also be the consequence of viral acute otitis externa.
Fungal myringitis can occur in cases of fungal otitis externa.
Eczematous myringitis can occur in cases of dermal eczema of the external acoustic canal.
Acute myringitis can occur in cases of an exacerbation of chronic inflammation of the EAC.
See also Middle Ear, Acute Otitis Media, Surgical Treatment and Middle Ear, Acute Otitis Media, Medical Treatment.
-
Perforation of the tympanic membrane
In untreated patients, as middle ear pressure increases, the TM eventually perforates, pain decreases, and mucopurulent discharge with blood appears in the EAC.
In cases of favorable cessation of AOM, the inflammatory process and all the inflammatory phenomena gradually regress with restoration of the TM and normal hearing.
Similar phenomena occur in cases of viral myringitis (influenza). With viral myringitis, as with acute bullous myringitis, bubbles filled with blood form on the surface of the TM and burst with effusing blood; however, the TM is not perforated.
-
Chronic myringitis with chronic otitis media
In cases of adverse courses of the inflammatory process, perforation of the TM persists. Persisting perforation is one characteristic sign of chronic otitis media (COM).
Chronic inflammation of the TM accompanies inflammation of the middle ear. On the surface of the TM, the epidermis is actively displaced into the ear canal, and, in 15% of cases, it may penetrate through small perforations of the TM. As a result, the middle ear is isolated, with resulting long-term hearing impairment.
This takes place in cases in which the speed of mucosal displacement and that of epidermal displacement coincide. If perforation of the TM is considerable, the epidermis and the mucous membrane meet on the edge of the perforation.
Some evidence exists that chronic otitis media may be related to extra-esophageal reflux. [3]
-
Mucoepidermal conflict
If the speed of the epidermis displacement and that of the mucosal displacement are different, conflict, which is typical for chronic myringitis, develops.
When the redundant mucous membrane penetrates the perforation and extends over the edges of the dermis, growth of the epithelium ceases.
The maceration of the dermis and its tendency to grow into the injured tissue become the main sources of inflammation. Lacking the necessary support, the mucous membrane forms granulation tissue and polyps.
When redundant tissue has formed within the middle ear mucosa, the epidermis penetrates into the middle ear space through the edge of the perforated TM and expands there; it is exposed to desquamation, and cholesteatoma is formed.
All types of dermatitis of the external ear affect the TM, involving it in similar inflammation.
-
Chronic myringitis with chronic otitis externa
Chronic myringitis is often accompanied by chronic bacterial inflammation of the EAC.
Chronic myringitis can also be the consequence of viral chronic otitis externa.
Chronic fungal myringitis can occur in cases of chronic fungal otitis externa.
Chronic eczematous myringitis can occur in cases of chronic dermal eczema of the external acoustic canal.
See also Middle Ear, Acute Otitis Media, Surgical Treatment and Middle Ear, Acute Otitis Media, Medical Treatment.
Epidemiology
Frequency
United States
Approximately 8% of children age 6 months to 12 years with AOM have acute bullous myringitis.
Mortality/Morbidity
Morbidity from myringitis is correlated with morbidity in cases of otitis media, external otitis, and foreign bodies in the ear.
Race
Data on racial distributions of TM diseases have not been collected. See also Middle Ear, Otitis Media with Effusion.
Sex
Males and females are affected by diseases of the TM with equal frequency.
Age
People of all ages are affected.
-
Tympanic membrane (TM) as continuation of the upper wall of external auditory canal (EAC) with angle of incline up to 45 degrees on the border between middle ear and the EAC.
-
Normal tympanic membrane. Pars tensa (PT), pars flaccida (PF), light reflex (LR), fibrous ring (FR), umbo (Um), handle of malleus (HM), lateral process of malleus (Lpm), anterior plica (AP), posterior plica (PP).
-
Mirror display of a tympanic membrane surface on the polymeric masc from external acoustical canal of healthy man. Masc of tympanic membrane surface (MtmS).






