Overview
Prior to COVID-19, more than 1.4 billion travelers worldwide crossed international boundaries - compared to just 25 million in 1950. [1, 2] Projections do not predict reaching 2019 levels until 2025; however, travel associated with tourism, humanitarian, or business efforts continues to increase. [3] Although COVID-19 related vaccination and travel requirements remain in a dynamic state, studies suggest only a small number of travelers seek appropriate pre-travel health advice. [1] In addition, the composition of those traveling continues to become more diverse and medically complex, creating a vastly different perspective on travel-associated medical concerns, preparations, required medical knowledge, and post-travel care precautions. [4]
Although downstream of the COVID-19 pandemic, its impact on travel requirements remain and continue to change globally. Ongoing travel requirements can be found on the CDC Travel website.
With the decreasing global boundaries and increasing activities, travel medicine is a rapidly evolving field of medicine - perhaps only paused by the COVID-19 pandemic. Classically, travel medicine focused on individuals traveling to low- and middle-income countries (LMICs) with prevention and treatment of malaria, traveler's diarrhea, cholera, and hepatitis and general vaccinations as its primary goal. Travel medicine has subsequently become a dynamic multidisciplinary specialty that encompasses aspects of infectious disease, public health, tropical medicine, wilderness medicine, immunization, and outbreak monitoring. Although these aspects are broad in reach, they are tightly integrated within the realm of travel medicine and require appropriate understanding before venturing out, as well as an increased awareness of patients presenting with illness after recent travel.
Whether you are a humanitarian aid worker in Tanzania, a volunteer working with refugees from an ongoing civil conflict, a community health educator navigating a recent measles outbreak, a tourist, or a businessperson for a multinational corporation, understanding the ongoing dynamics of travel with the interplay of healthcare will minimize the adverse effect of travel-related illnesses, increase your pre-travel awareness, and quite possibly assuage your health-related concerns while maximizing your efforts, enjoyment, and the success of your activities.
See the Medscape slideshow 12 Travel Diseases You Need To Know for information about infectious travel diseases that may pertain to your or your patients' upcoming or recent travel.
Travel Medicine: The Big Picture
Travel medicine remains dynamic and increasingly broad in its medical knowledge requirements, as it focuses on the prevention, surveillance, and management of health issues related to global travel. Areas of expertise include vaccinations, epidemiology, region-specific travel medicine, pre-travel management, travel-related illnesses, and post-travel management. This increasing globalization of travel, well over 1 billion annually (with ~80% from developed-to-LMICs), facilitates increased health exposures in different environments and the potential spread of disease.
Although the Centers for Disease Control and Prevention (CDC) and World Health Organization (WHO) provide the backbone of current medical considerations, several groups have taken a paramount role in developing a structured curriculum to better identify the realm and role of travel medicine as a subspecialty of care. Two such examples are the International Society of Travel Medicine (ISTM) and the American Society of Tropical Medicine and Hygiene (ASTMH). The formation of such groups has allowed for a more open dialogue about the required body of knowledge for the practice of travel medicine and thereby improved related resources to an ever-expanding diversity of travelers.
 Awareness of and preparation for travel-related illnesses remain essential: Aedes aegypti mosquito. Courtesy of Wikimedia Commons [author Muhammad Mahdi Karim, https://commons.wikimedia.org/wiki/File:Aedes_aegypti.jpg].
Awareness of and preparation for travel-related illnesses remain essential: Aedes aegypti mosquito. Courtesy of Wikimedia Commons [author Muhammad Mahdi Karim, https://commons.wikimedia.org/wiki/File:Aedes_aegypti.jpg].
In addition, collaborative sentinel surveillance networks such as TropNet and GeoSentinel provide pre-travel and post-travel patient management by providing complementary surveillance information, facilitating communication and collaboration between participating network sites, and enabling new analytical options for travel-related research.
Pre-travel Medical Preparation
According to the CDC, 43-79% of travelers to LMICs become ill with a travel-related health problem. With a heightened interest in adventure travel, international destinations, and ecotourism, more patients return from vacations with presentations of possible exotic diseases that are beyond the scope of a primary care or emergency physician's daily practice. However, much of the illnesses encountered could be eliminated with adequate pre-travel education and preparation. When prophylactic treatment and lifestyle modification fail, physicians need to know what to look for and where to find clinical information on exotic diseases beyond the scope of daily practice. Further information can be quickly and easily accessed through the CDC Yellow Book, an online resource providing country-specific information related to endemic diseases and important travel medicine updates. Another important tool is the Pre-Travel Providers’ Rapid Evaluation Portal (Pre-Travel PREP) that aids physicians (and their patients) by acting as an interactive Yellow Book.
Pre-travel preparation
Whether the participant is on an extended excursion in Mongolia, serving at a medical mission in Belize, or is an adventure-seeking traveler, preparation is paramount to a successful venture. This preparation should begin during the planning stages of travel, preferably months in advance of departure to allow for updated immunizations and any additional travel clinic concerns identified. Travelers should become informed about the potential hazards of the countries they are traveling to and learn how to minimize any risk to their health. Forward planning, appropriate preventive measures, and careful precautions can substantially reduce the risks for adverse health consequences. Although the medical profession and the travel industry can provide a great deal of help and advice, the traveler is ultimately responsible to ask for information, to understand the risks involved, and to take the necessary precautions for the journey. In addition, consideration should be given to any underlying medical or comorbid condition of each traveler—as medications and emergency/evacuation planning should be established prior to leaving.
Initially, travelers should ascertain the associated travel health information commonly available online. This usually includes general health information such as vaccine requirements, prophylactic medications, disease outbreaks, political environment, and medical resources. While this online overview is helpful, this should not exclude consideration for a pre-travel medical consultation and evaluation.
Although often overlooked, dental and obstetric/gynecologic (OB/GYN) checkups are advisable before travel to developing countries - especially for prolonged travel to remote areas. This is particularly important for people with chronic or recurrent dental, OB/GYN, or other health-related problems.
Medical preparation essentials for travel
Before departure for any extended or overseas travel, the following information should be obtained:
-
Geographic itinerary
-
Duration and month(s) of travel
-
Urban travel versus rural travel
-
Anticipated living conditions and resources
-
Purpose of travel
-
Plan for special activities such as extreme sports (ie, skydiving, rafting, rock climbing, scuba diving)
-
Medical care resources available during travel and health-related contingency planning, including evacuation insurance
-
Knowledge of any known disease risk or precautions advised ( CDC Yellow Book)
-
Understanding that re-entry into the United States or countries with connecting flights may be refused to travelers who have been exposed to some diseases or during specific illness outbreaks (ie, requirement for proof of negative COVID-19 test) [5]
Personal health information should be obtained and carried, including the following:
-
Personal health status (eg, age, weight, pregnant)
-
Medications (including a full supply for a duration longer than your scheduled trip) and allergies
-
Past medical history such as history of heart disease (keep an EKG copy on electronic device such as phone), stroke, recent surgery, and immunocompromising conditions
-
Medical or physical limitations
Basic health travel kit
A medical kit is an essential item that should be carried by all travelers to resource austere environments, LMICs, or where local availability of such resources remains in doubt. The kit should include standard first-aid items, simple medications for common ailments, and any items specific for that traveler's known medical conditions. In addition, consider having a list of medications along with a medical attestation signed by a physician authenticating the need of those medications for personal use. If you have specialty medications, ensure that those medications (or a substitute) are available where you are traveling should an issue arise.
Some countries do not allow certain medications, commonly prescription pain medications, into the country without a physician letter and without medication being in the original pharmacy bottle. Standard toiletry items (including menstrual products, if appropriate) sufficient for the entire travel period are recommended. Procuring even the most basic items can present a challenge because of language barriers and resource constraints. [6, 7]
First-aid items to consider often include the following:
-
Glasses and contact lenses (replacement pair)
-
Wound coverings: adhesive bandages, medical tape, sterile gauze
-
Hand sanitizer (containing at least 60% alcohol) or antibacterial hand wipes
-
Eye drops (rewetting or saline) and cotton swabs (Q-tips)
-
Medical alert bracelet or necklace
-
Diabetes testing supplies
-
Water purifier/disinfectant
-
Physicians may wish to carry a small suture kit
-
Oral rehydration powder
-
Scissors, safety pins/closure devices
-
Thermometer (oral/rectal)
-
Disposable gloves
Prescription and over the counter medicines:
-
Personal medications (for current medical conditions; must not forget insulin, inhalers, and EpiPens)
-
Antinausea medication (if any water travel or winding roads anticipated) and antihistamine
-
Travelers’ diarrhea medications
-
Antifungal medication
-
Malaria prophylaxis (based on travel-clinic and/or CDC recommendations)
-
Sleeping medications
-
Motion sickness medicine
-
Decongestant, cough drops, cough suppressant, or expectorant
-
Pain and fever medicine (acetaminophen, aspirin, or ibuprofen)
Travelers insurance
Most US travelers have no travelers health insurance or are under-covered. In addition, Medicare and Medicaid, in most circumstances, do not cover medical costs overseas. After the COVID-19 pandemic, travelers insurance has increased slightly with recent statistics showing 12.8% of US travelers purchasing general travelers insurance. [8] Trip cancellation, baggage protection, medical insurance, medical/emergency evacuations, and trip cancellations are the most standard categories offered for coverage. Commonly, travelers health insurance covers accidental death, disablement, accidental medical reimbursement, and 24-hour emergency assistance. [9] In most countries, including countries with a nationalized healthcare system, travelers are most likely to pay out of pocket for any medical services. Reimbursement from your travel insurance follows. Travel insurance is especially recommended if you have chronic disease states (ie, congestive heart failure, respiratory limitations, poorly controlled diabetes, chronic renal conditions, etc.) or remain on a very restricted medical care regimen. More information can be found on the CDC website.
Vaccination and Immunization
In the Travelers' Health section, the CDC clearly delineates what one needs to know about vaccinations for a desired travel destination. There are 3 major categories of vaccinations: routine, recommended, and required.
 Patient receiving updated vaccinations prior to travel. Courtesy of the Centers for Disease Control and Prevention (CDC), National Center for Immunization and Respiratory Diseases (NCIRD) [Photo/Lauren Bishop, https://www.cdc.gov/flu/resource-center/toolkit/photo-gallery.htm].
Patient receiving updated vaccinations prior to travel. Courtesy of the Centers for Disease Control and Prevention (CDC), National Center for Immunization and Respiratory Diseases (NCIRD) [Photo/Lauren Bishop, https://www.cdc.gov/flu/resource-center/toolkit/photo-gallery.htm].
Routine vaccinations are the immunizations that are routinely provided as a part of one’s normal health maintenance (eg, MMR and tetanus immunization). These vaccines are necessary for protection from diseases that remain common in many parts of the world, although infrequently in the United States.
Recommended vaccinations are predicated on a number of factors including one’s travel destinations, planned activities, season, previous immunizations, urban/rural location, age, and current health status. These vaccinations are recommended to protect travelers from illnesses present in other parts of the world and to prevent the importation of infectious diseases across international borders. For example, there is a current outbreak of diphtheria in several states in Nigeria. All travelers aged 2 months and older or travelers who have not received a booster dose within 5 years should receive an age appropriate dose of a diphtheria toxoid-containing vaccine. Special considerations for aging, immune compromised, pregnant, immigrant, chronically ill, students, and disabled travelers are essential.
Required vaccines vary greatly depending on the points of travel. Considering the COVID-19 pandemic, the support for required vaccines have garnered increased focus. Currently, all non-US citizen and non-US immigrant travelers must show proof of being fully vaccinated. The International Health Regulations require yellow fever vaccination for travel to certain countries in sub-Saharan Africa and tropical South America. In addition, those traveling during the Hajj are required by the government of Saudi Arabia to obtain the meningococcal vaccination. Belize, among other countries, does not allow cruise ship or airplane passengers to disembark without yellow fever vaccination because of destinations the traveler(s) may have visited during the trip, not necessarily because yellow fever is in the country. Travel itineraries often do not explain these details. The recommendations are subject to change as new diseases invade new areas, and existing diseases may change or develop medication resistance (eg, malaria). A list of required, recommended, and routine vaccines can be found on the World Health Organization (WHO) website.
Depending on the intended destination, it is essential to remember the risk for exposures to diseases that are rare in the United States. Understanding the role and importance of country specific vaccinations is vital prior to traveling. Once the regions of anticipated travel are identified, scheduling a visit to one’s doctor or a travel medicine provider is essential. It is ideal to schedule an appointment 4-6 weeks before the trip because most vaccinations require a period of days or weeks to become effective. Important questions to ask before getting vaccines include locations of travel, health status (ie, pregnancy and immunocompromise), and the vaccinations previously received. If uncertain regarding previous immunizations, variable tests are available to identify appropriate titer levels and whether updated boosters are indicated. A list of vaccine preventable diseases and specific laboratory collection methods can be found on the CDC website.
Common Health Problems Associated With Travel
A great resource to identify common health problems associated with travel can be found online through the Diseases Related to Travel section of Travelers' Health on the CDC Web site. Whether dealing with COVID-19, malaria, cholera, dengue fever, or altitude sickness, having a basic understanding of the common illnesses specific to the region of travel is essential.
By far, the most common health risk for travelers, especially those visiting developing countries, is traveler's diarrhea (TD). Every year, the CDC reports that 30-70% of international travelers (an estimated 12-15 million people) develop diarrhea, usually within the first week of travel. Traveler’s diarrhea, however, may occur at any time while traveling, even after returning home. TD occurs equally in males and females. The primary cause is contaminated food or water, typically found in areas with poor sanitation. Common symptoms of traveler’s diarrhea include abrupt onset, cramps, increased frequency/urges, bloating, flatus, fever, and malaise. Infectious agents are the primary cause of traveler’s diarrhea. Bacterial enteropathogens cause approximately 80% of traveler’s diarrhea cases. The most common causative agent isolated in countries surveyed has been enterotoxigenic Escherichia coli (ETEC). Strict adherence to preventive measures is encouraged, and bismuth subsalicylate should be used as an adjunct if prophylaxis is needed and the traveler is able to take it.
Advice for travelers
Travelers should be advised to eat only food that is hot or boiled and to drink only bottled beverages, making certain the seal has not been broken prior to it being placed in front of them. In addition, it's vital to avoid eating fruits that are not peeled and vegetables that are not washed. These actions and meticulous handwashing can prevent nearly all cases of traveler’s diarrhea.
Treatment of traveler's diarrhea
Traveler's diarrhea rarely is life threatening. Most cases are benign and resolve in 1-2 days without treatment, 90% of cases resolve within 1 week, and 98% resolve within 1 month. Because traveler's diarrhea usually is self-limiting, oral rehydration often is the only treatment recommended. Clear liquids routinely are recommended for adults. If a traveler develops 3 or more loose stools in an 8-hour period and has associated nausea, vomiting, abdominal cramps, fever, or blood in stools, they may benefit from antimicrobial therapy. If vomiting is not well controlled or diarrhea is very frequent, oral rehydration salts are recommended and necessary.
Although nearly 90% effective, antibiotics are not recommended as prophylaxis. Routine antimicrobial prophylaxis increases the traveler's risk for adverse reactions and for infections with resistant organisms, specifically extended-spectrum beta-lactamase–producing Enterobacteriaceae (ESBL-PE). Antibiotics provide no protection against either viral pathogens or parasitic pathogens; therefore, they can give travelers a false sense of security. Antibiotics, which should be reserved for moderate to severe cases, may reduce the duration of diarrhea by 1-2 days.
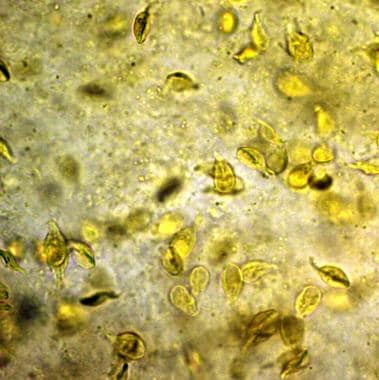
While fluoroquinolones have been the drug of choice, increasing microbial resistance, especially among Campylobacter isolates, may limit their usefulness in some destinations such as Thailand and other countries in southeast Asia, where Campylobacter is prevalent. Increasing cases of fluoroquinolone resistance have been reported from other destinations. Alternatives in this situation include azithromycin, rifaximin, or rifamycin SV. [7, 10] Other causes to consider for traveler's diarrhea include protozoan infections. The most common cause is Giardia duodenalis. Treatment consideration with metronidazole, tinidazole, and nitazoxanide is recommended by the CDC.
Other common health problems associated with travel to LMICs include malaria, influenza, and other respiratory tract infections. More information can be found at Diseases Related to Travel section of Travelers' Health on the CDC Web site.
Activity Specific Consideration
Most travel experiences are bundled with special activities such as scuba diving, rafting, mountain climbing (exposure to high altitude), wilderness travel, and many more activities. Special considerations must be taken to ensure the safety of travelers while performing their activities. For example, travelers must avoid airplane travel for 12 to 48 hours after scuba diving to avoid decompression sickness. Regarding high-altitude sickness, travelers should be educated on the symptoms of mountain sickness, high-altitude pulmonary edema, and high-altitude cerebral edema. Modifiable risk factors such as rate of ascent and pharmacologic measures such as acetazolamide as prophylaxis and treatment of acute mountain sickness could be considered. [11]
Wilderness travel encompasses travel to remote areas that lack clinics, and exposure to extreme climates is common. Resource utilization is important to discuss with travelers. Improvisation (ie, creative use of unusual supplies for diagnosing, treating, splinting, transporting) is an invaluable skill taught in Wilderness Medical Society (WMS) and other similar courses. Efficient selection and knowledge of medications lightens the medical kit. For example, rather than carrying multiple antibiotics of choice for several possible infections, consider carrying a medication, such as ciprofloxacin, which despite some growing resistance issues, treats traveler's diarrhea (TD) as well as respiratory, wound, bladder, and other infections. Another example is diphenhydramine, which is excellent as an injectable local anesthetic as well as treatment for nausea, allergic reactions, and insomnia.
COVID-19 Travel Considerations
The COVID-19 pandemic has accelerated innovative ways to use technology to deliver care abroad and has pushed travel advisories (ie, CDC, WHO) to continually update and educate travelers on travel-associated medical considerations including vaccines. [12] One important consideration is understanding COVID-19 country-specific requirements prior to travel. Health screening questionnaires and a negative COVID-19 PCR/serology testing are required by most countries. Travelers must also consider return requirements from certain destinations such as China or Hong Kong. Travelers aged 2 years and older flying to the United States from China, Hong Kong, or Macau, or who have been in these areas in the past 10 days and are flying from certain airports, are required to show a negative COVID-19 test result or documentation of recovery from COVID-19 before boarding their flight to the United States. Non-US citizens are required to be fully vaccinated with accepted COVID- 19 Vaccine. A list of proof and acceptable vaccines can be found on the CDC website.
Other Factors To Consider
Unique Circumstances
Physicians planning to serve as an expedition physician are advised to take a course provided by the WMS or a similar course by other providers. Requisite emergency skills may vary based on location, weather, activities, and availability of medical care resources. A physician may need knowledge of unusual diseases and injuries specific to certain activities or locations. These could include extrication and rescue skills in various environmental situations and improvisational skills and treatment of many medical emergencies. Many of these skills can be easily identified with adequate travel preparation and an understanding of the environment in which one will be traveling. However, regardless of the level of preparation, unplanned emergencies often occur, and one's level of preparation may dictate the success with which care is provided. [13, 14] Detailed logistical planning, skills, equipment, medications, and resources for varied groups and destinations are beyond the scope of this article. Such information is readily available in both courses and textbooks from the WMS and the International Society of Travel Medicine (ISTM).
Legal Issues
Travel medicine providers are subject to legal actions whether the medical care is planned or unplanned. Before understanding the specific nuances and details of medical liability with regard to wilderness and travel medicine, an understanding of the general framework is essential.
Legal consideration in planned medical care:
Whether contracted to provide care for an expedition or volunteering at a medical clinic in a developing country, legal protection can vary as much as one's moral obligation to treat. It is advised to provide written documentations of any pretravel recommendations, medications, and vaccinations to travelers. In the unfortunate circumstance of a poor treatment outcome, a patient's signed release or a documentation provided often will not protect a physician from legal actions. It is highly recommended to review the malpractice domains where care will be delivered, confirm the medical coverage, and assess the medical liability associated with the planned travel destinations. Physicians who are paid to provide care to a group have increased liability and must ascertain the level of malpractice coverage.
Legal consideration in unplanned medical care:
Situations may arise in which physicians feel a moral obligation to help but have no legal protection. Malpractice and Good Samaritan laws differ from state to state and in foreign countries. Providers must understand the limitations of such laws (ie, Good Samaritan) prior to travel. For example, 1 legal argument used against the Good Samaritan defense has been that possession of any medical equipment showed that the physician had planned to practice medicine and therefore was not protected by the Good Samaritan law. In regards to unplanned medical care delivery, physicians are advised to decide ahead of time where to draw the line.
Medical Tourism
The currently used definition of "Medical Tourism" refers primarily to a phenomenon of travelers leaving family and friends to seek care abroad, often in less developed countries, along with the organizations that support or offer incentives for such travel. Although not exact, it is estimated that up to 20 million medical tourists (1.9 million US residents) receive care beyond their borders annually. In traditional medical tourism, patients used to travel to developed economies (ie, Europe and the United States) to receive high-end treatments, owing to lack of or delays with treatment options in a patient's respective country. However, the scenario has shifted to medical care being provided in developing countries with improving infrastructure and a focus on the lucrative medical tourism industry. It is reported that the medical and dental tourism industry exceeds $400 billion and is growing. The reported cost savings for the treatments in these settings are 30-70% of the total treatment cost.
The specific risks of medical tourism depend on the procedure being performed, the area being visited, the resources available for the procedure at that location, and the associated issues related to travel and follow-up care. [15] As medical tourism continues to increase, physicians should be either familiar with up-to-date sources of information (eg, Travelers' Health) or referral options, and inquire whether or what role travel plays in their patient's life and medical care. The Joint Commission International is a US-based healthcare facility certification organization that will attest to specific care standards and may provide insight into a patient's desired care site.
Cruise Ship Medicine
Travel by cruise ship often congregates large groups of people from different parts of the United States and the world. In such settings, diseases (influenza, measles, rubella, Norwalk virus, gastrointestinal illnesses) can spread from person-to-person contact. Additionally, if a ship comes to port and passengers disembark to sightsee, they may be at risk for other geographic specific diseases, although such risk is difficult to quantify given the limited duration of exposures. Note that certain diseases can be transmitted before symptoms are apparent and that some people who become ill while on a cruise ship may have been infected prior to travel. Add to that the complexity often seen with an increasingly mobile aging population with multiple medical problems and one can see that staffing a medical facility on a cruise ship can present many unique challenges.
Cruise ships have onboard medical staff who should be sought for any illness. While historically different, today, most cruise ships require a ship physician to have some emergency medicine experience. Many ships have minimal medications and few, if any, have laboratory or radiographic capabilities. However, some have mini–critical care units complete with monitors, ventilators, defibrillators/pacers, and appropriate medications. In general, the lack of resources can exhaust a physician's diagnostic and medical skills on a regular basis. One critical patient or an outbreak of Norwalk virus can overwhelm the ship’s hospital staff and use up all available resources while at sea. Ship authorities will report infectious diseases of public health significance to state or federal health officials.
Advice for cruise ship travelers
Those planning cruise ship travel, especially those older than 65 years, those with chronic illnesses, or those who are pregnant or breastfeeding should consult with a healthcare provider before travel for advice, medical planning, and possible preventive medications and immunizations. For those with chronic illnesses, ensuring optimal medications and any needed devices (ie, NIPPV for OSA) and power adapters are critical for a successful venture. Common hand hygiene remains paramount for all travelers, but even more so for those at risk. Keep in mind that handrails, elevator buttons, salt shakers, or any other surfaces have been touched by hundreds of people from endless locations in variable states of health. Travelers who become ill should report to the infirmary for assessment and subsequently limit contact with the general population on board as much as possible to reduce further spread of disease. Medical follow-up after returning from a trip also is important - especially if an individual became symptomatic during or after their travels.
For those clinicians that provide on-board patient care, cruise ship medicine is not all work and no play. Travel and entertainment opportunities are endless. The volume of patients seen and the level of illness may vary. Conversely, cruise ship epidemics may require the physician and staff to remain quarantined at sea for weeks. For more information on serving as a cruise ship physician, contact the ACEP Cruise Ship and Maritime Medicine Section.
Summary
Travel medicine is a dynamic field because conditions worldwide are subject to rapid change and are highly variable as they relate to the medical resources at hand. Clinicians must maintain a current base of knowledge encompassing a wide variety of disciplines including epidemiology, infectious disease, public health, tropical medicine, immigrant and refugee health, and occupational medicine. As a unique and rapidly growing specialty (in light of COVID-19 pandamic), standards of practice have been established to identify the scope of competencies expected of travel medicine practitioners, guide their professional training and development, and ensure a uniform level of patient care. Whether related to traveling abroad for leisure, work, or study, having updated health information, medications, and vaccinations helps to ensure safe and healthy travel.
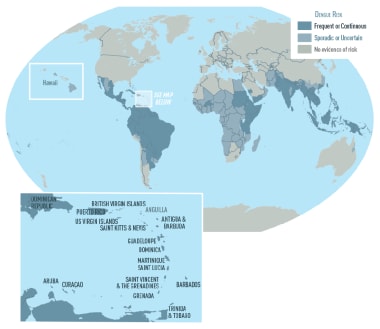 Awareness of potential illness threats improves travel preparations. Courtesy of the Centers for Disease Control and Prevention (CDC) [https://www.cdc.gov/dengue/index.html].
Awareness of potential illness threats improves travel preparations. Courtesy of the Centers for Disease Control and Prevention (CDC) [https://www.cdc.gov/dengue/index.html].
As outbreak locations continue to change, it is important to inquire about recent travel history for anyone presenting with acute illness. In addition, realizing that many serious diseases initially present similarly to common viral illnesses places even more importance on that travel history and the providers’ due diligence. With global travel being common, keep in mind that modern travel vessels, whether airplane or high-speed train, may contain passengers from 50 countries or 50 states. Documenting recent travel for a patient with ”the flu” may, 1 month later, provide a clue for the CDC or the WHO.
The following are important points to consider prior to departure:
-
Consult a travel medicine professional before leaving home. They can provide vital information for staying healthy, updating vaccinations, and providing prophylactic and precautionary medications.
-
US travelers going overseas should enroll in the Smart Traveler Enrollment Program (STEP) to receive ongoing travel updates their area(s) of travel
-
Assess physical and medical limitations related to the anticipated travel; develop a care plan and follow the precautions related to the planned travel comorbid conditions.
-
Colds are a common problem among tourists, especially when confined to crowded conditions (eg, buses, cruise ships). Practice exquisite handwashing and limiting personal contact with others to minimize contamination.
-
Sexually transmitted diseases frequently are associated with unsafe practices while traveling. Instruct patients to avoid unsafe sex to protect themself and their partner.
-
Gastrointestinal disorders are very common ailments among travelers. Purified hydration and good hygiene are essential.
-
Travelers should be aware of those with whom they are traveling, and help them get the proper medical attention when necessary.
-
Travelers should check with their insurance carrier as to whether they have international coverage and evacuation insurance. If not, they should consider a short-term policy during travel.
-
When traveling globally, travelers should respect the unique aspects of the culture and people, and they should remain considerate to best ensure a pleasant, enjoyable trip.
Useful Resources
Available resources
Available resources include the following:
-
CDC Travelers' Health Automated Information Line (877) FYI-TRIP
Preparation for nonmedical emergencies
The following website provides information on preparing for nonmedical emergencies:
Recommended texts
Recommended texts include the following:
-
CDC Yellow Book 2020: Health Information for International Travel (The Yellow Book). Oxford University Press; 2020.
-
Rose SR, Keystone JS. International Travel Health Guide; 2019 Online Edition.
-
Auerbach PS. Wilderness Medicine: Management of Wilderness and Environmental Emergencies. 7th ed. Mosby; 2017.
-
Global travel remains on the rebound after COVID-19.
-
Awareness of and preparation for travel-related illnesses remain essential: Aedes aegypti mosquito. Courtesy of Wikimedia Commons [author Muhammad Mahdi Karim, https://commons.wikimedia.org/wiki/File:Aedes_aegypti.jpg].
-
Create a basic health kit specific to your travel plans and needs.
-
Patient receiving updated vaccinations prior to travel. Courtesy of the Centers for Disease Control and Prevention (CDC), National Center for Immunization and Respiratory Diseases (NCIRD) [Photo/Lauren Bishop, https://www.cdc.gov/flu/resource-center/toolkit/photo-gallery.htm].
-
Stool specimen of a traveler with diarrhea after a tainted water exposure.
-
Awareness of potential illness threats improves travel preparations. Courtesy of the Centers for Disease Control and Prevention (CDC) [https://www.cdc.gov/dengue/index.html].