Practice Essentials
Carpal tunnel syndrome (CTS) is a compressive neuropathy of the median nerve at the wrist. [1] The carpal tunnel is located at the base of the palm and is bounded on 3 sides by carpal bones and anteriorly by the transverse carpal ligament. Inside run the median nerve, the flexor tendons, and their synovial sheaths. It is the most common entrapment neuropathy, with repetitive, forceful angular hand movements or vibration placing persons at risk for the condition. Diagnosis is based on clinical history and findings, along with corroborating electrodiagnostic studies. [2, 3, 4, 5, 6, 7]
Carpal tunnel syndrome is caused predominantly by compression of the median nerve at the wrist because of hypertrophy or edema of the flexor synovium. Pain is thought to be secondary to nerve ischemia rather than direct physical damage of the nerve. [8, 9, 10] Among working adults in the United States, estimated lifetime and 12-month prevalence are 6.7% and 3.1% respectively. [11] Early in the course of CTS, the neurologic findings are reversible. If left untreated, CTS can result in thenar atrophy, chronic hand weakness, and numbness in the median nerve distribution of the hand. CTS is more prevalent in females than in males and most common in middle age. [2, 12]
Carpal tunnel syndrome (CTS) is a collection of characteristic symptoms and signs that occurs following compression of the median nerve within the carpal tunnel. Usual symptoms include numbness, paresthesias, and pain in the median nerve distribution. These symptoms may or may not be accompanied by objective changes in sensation and strength of median-innervated structures in the hand. Patients typically complain of an intermittent "pins-and-needles" paresthesia in the median nerve distribution of the hand. Classic carpal tunnel syndrome (CTS) is associated with symptoms that affect at least 2 of the first through third digits; symptoms affecting the fourth and fifth digits, wrist pain, and radiation of pain proximal to the wrist may also occur, but classic CTS is not associated with symptoms on the palm or dorsum of the hand. [13]
Electrophysiologic studies, including electromyography (EMG) and nerve conductions studies (NCS), are the first-line investigations in suggested carpal tunnel syndrome (CTS). Nerve conduction studies show a high specificity (95%) with a wide range of sensitivity depending on the choice of cutoff values (75-92%). Due to this high specificity, nerve conduction studies are recommended prior to considering surgical intervention [14] .
In the emergency department setting, the mainstay of treatment for carpal tunnel syndrome (CTS) is rest, wrist immobilization with a splint, and nonsteroidal anti-inflammatory drugs (NSAIDs). For some individuals with CTS, nonsurgical management is curative; however, more than 50% of patients undergoing nonsurgical management progress to surgery within 1 year. [15]
Definitive therapy consists of surgical release of the transverse carpal ligament. Surgery for CTS has a long-term success rate of greater than 75%.
(See the images below.)
 Carpal tunnel syndrome. Carpal and Guyon tunnels. Drawing showing the proximal level of the carpal tunnel delimited by the pisiform (P) and the scaphoid (S). The flexor retinaculum (medium gray region) forms the roof of the carpal tunnel and the floor of the Guyon tunnel. The palmar carpal ligament (dark gray region) forms the volar boundary of the Guyon tunnel. * = flexor pollicis longus tendon, * = flexor carpi radialis tendon. From Martinoli C, Bianchi S, et al. US of nerve entrapments in osteofibrous tunnels of the upper and lower limbs. Radiographics 2000; 20:S199-S217. Used by permission of the authors and RSNA.
Carpal tunnel syndrome. Carpal and Guyon tunnels. Drawing showing the proximal level of the carpal tunnel delimited by the pisiform (P) and the scaphoid (S). The flexor retinaculum (medium gray region) forms the roof of the carpal tunnel and the floor of the Guyon tunnel. The palmar carpal ligament (dark gray region) forms the volar boundary of the Guyon tunnel. * = flexor pollicis longus tendon, * = flexor carpi radialis tendon. From Martinoli C, Bianchi S, et al. US of nerve entrapments in osteofibrous tunnels of the upper and lower limbs. Radiographics 2000; 20:S199-S217. Used by permission of the authors and RSNA.
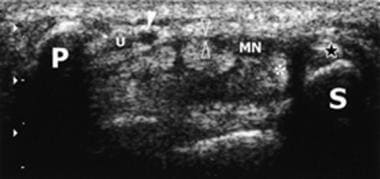 Carpal tunnel syndrome. Carpal and Guyon tunnels. Transverse 5-12-MHz ultrasound scan corresponding to the image above shows the proximal level of the carpal tunnel delimited by the pisiform (P) and the scaphoid (S). The flexor tendons and median nerve (MN) extend through the carpal tunnel, with the nerve lying palmar and radial. The flexor retinaculum (open arrowheads) forms the roof of the carpal tunnel and the floor of the Guyon tunnel. At the level of the pisiform, the ulnar nerve (U) courses medial to the ulnar artery (solid arrowhead) within the Guyon tunnel. * = flexor pollicis longus tendon. From Martinoli C, Bianchi S, et al. US of nerve entrapments in osteofibrous tunnels of the upper and lower limbs. Radiographics 2000; 20:S199-S217. Used by permission of the authors and RSNA.
Carpal tunnel syndrome. Carpal and Guyon tunnels. Transverse 5-12-MHz ultrasound scan corresponding to the image above shows the proximal level of the carpal tunnel delimited by the pisiform (P) and the scaphoid (S). The flexor tendons and median nerve (MN) extend through the carpal tunnel, with the nerve lying palmar and radial. The flexor retinaculum (open arrowheads) forms the roof of the carpal tunnel and the floor of the Guyon tunnel. At the level of the pisiform, the ulnar nerve (U) courses medial to the ulnar artery (solid arrowhead) within the Guyon tunnel. * = flexor pollicis longus tendon. From Martinoli C, Bianchi S, et al. US of nerve entrapments in osteofibrous tunnels of the upper and lower limbs. Radiographics 2000; 20:S199-S217. Used by permission of the authors and RSNA.
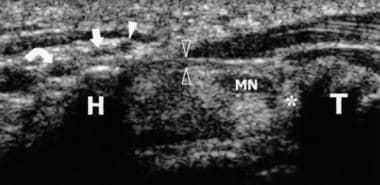 Carpal tunnel syndrome. Carpal and Guyon tunnels. Transverse 5-12-MHz ultrasound scan corresponding to the image above shows the distal level of the carpal tunnel delimited by the hook of the hamate (H) and the tubercle of the trapezium (T). The flexor retinaculum (open arrowheads) forms the roof of the carpal tunnel. The flexor tendons and median nerve (MN) extend through the carpal tunnel, with the nerve lying palmar and radial. At the level of the pisiform, the ulnar nerve courses medial to the ulnar artery (solid arrowhead) within the Guyon tunnel. At the level of the hamate, the ulnar nerve divides into two terminal branches, a deep motor branch (curved arrow) and a superficial sensory branch (straight arrow). From Martinoli C, Bianchi S, et al. US of nerve entrapments in osteofibrous tunnels of the upper and lower limbs. * = flexor pollicis longus tendon. Radiographics 2000; 20:S199-S217. Used by permission of the authors and RSNA.
Carpal tunnel syndrome. Carpal and Guyon tunnels. Transverse 5-12-MHz ultrasound scan corresponding to the image above shows the distal level of the carpal tunnel delimited by the hook of the hamate (H) and the tubercle of the trapezium (T). The flexor retinaculum (open arrowheads) forms the roof of the carpal tunnel. The flexor tendons and median nerve (MN) extend through the carpal tunnel, with the nerve lying palmar and radial. At the level of the pisiform, the ulnar nerve courses medial to the ulnar artery (solid arrowhead) within the Guyon tunnel. At the level of the hamate, the ulnar nerve divides into two terminal branches, a deep motor branch (curved arrow) and a superficial sensory branch (straight arrow). From Martinoli C, Bianchi S, et al. US of nerve entrapments in osteofibrous tunnels of the upper and lower limbs. * = flexor pollicis longus tendon. Radiographics 2000; 20:S199-S217. Used by permission of the authors and RSNA.
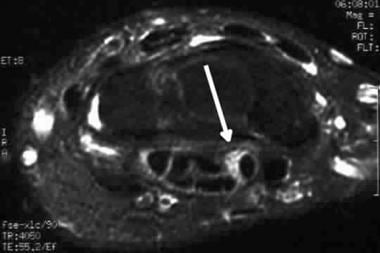 Carpal tunnel syndrome. Axial fast spin-echo T2-weighted MRI with fat saturation. Note the increased T2-weighted signal within the median nerve (arrow). A slightly increased cross sectional area of the nerve is noted but the nerve architecture is preserved, consistent with early or mild inflammation.
Carpal tunnel syndrome. Axial fast spin-echo T2-weighted MRI with fat saturation. Note the increased T2-weighted signal within the median nerve (arrow). A slightly increased cross sectional area of the nerve is noted but the nerve architecture is preserved, consistent with early or mild inflammation.
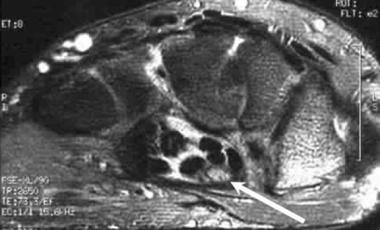 Carpal tunnel syndrome. Fast spin-echo T2-weighted MRI illustrates more pronounced increased signal within the median nerve (arrow). Note the small amount of fluid within the carpal tunnel, a secondary sign of inflammation. Slightly less optimal fat saturation is noted than on other images, which is a common occurrence.
Carpal tunnel syndrome. Fast spin-echo T2-weighted MRI illustrates more pronounced increased signal within the median nerve (arrow). Note the small amount of fluid within the carpal tunnel, a secondary sign of inflammation. Slightly less optimal fat saturation is noted than on other images, which is a common occurrence.
American Academy of Orthopaedic Surgeons Guidelines
The AAOS has published guidelines on diagnosis and treatment of carpal tunnel syndrome, including the following [16] :
-
Thenar atrophy is strongly associated with ruling in CTS but is poorly associated with ruling it out
-
Do not use the Phalen test, Tinel sign, flick sign, or upper limb neurodynamic/nerve tension test (ULNT) criterion A/B as independent physical examination maneuvers to diagnose CTS, because alone, each has a poor or weak association with ruling in or ruling out the condition
-
Do not use the following as independent physical examination maneuvers to diagnose CTS, because alone, each has a poor or weak association with ruling in or ruling out the condition: carpal compression test, reverse Phalen test, thenar weakness or thumb abduction weakness or abductor pollicis brevis manual muscle testing, two-point discrimination, Semmes-Weinstein monofilament test, CTS-relief maneuver, pin prick sensory deficit (thumb or index or middle finger), ULNT criterion C, tethered median nerve stress test, vibration perception (tuning fork), scratch collapse test, Luthy sign, and pinwheel
-
Do not use the following as independent history interview topics to diagnose CTS, because alone, each has a poor or weak association with ruling in or ruling out the condition: sex/gender, ethnicity, bilateral symptoms, diabetes mellitus, worsening symptoms at night, duration of symptoms, patient localization of symptoms, hand dominance, symptomatic limb, age, and body mass index
-
Do not routinely use magnetic resonance imaging (MRI) for the diagnosis of CTS
-
Diagnostic questionnaires and/or electrodiagnostic studies can be used to aid the diagnosis of CTS
-
The following factors are associated with an increased risk of developing CTS: peri-menopausal, wrist ratio/index, rheumatoid arthritis, psychosocial factors, distal upper extremity tendinopathies, gardening, American Conference of Governmental Industrial Hygienists (ACGIH) hand activity level at or above threshold, assembly line work, computer work, vibration, tendonitis, workplace forceful grip/exertion
-
Physical activity/exercise is associated with a decreased risk of developing CTS
-
The use of oral contraception and female hormone replacement therapy are not associated with increased or decreased risk of developing CTS
-
The use of immobilization (brace/splint/orthosis) should improve patient reported outcomes
-
The use of steroid (methylprednisolone) injection should improve patient reported outcomes
-
Magnet therapy should not be used for the treatment of CTS
-
There is no benefit to oral CTS treatments (diuretic, gabapentin, astaxanthin capsules, nonsteroidal anti-inflammatory drugs [NSAIDs], or pyridoxine) over placebo
-
Oral steroids could improve patient reported outcomes in comparison with placebo
-
Ketoprofen phonophoresis could provide reduction in pain in comparison with placebo
-
The surgical release of the transverse carpal ligament should relieve CTS symptoms and improve function
-
Surgical treatment of CTS should have a greater therapeutic benefit at 6 and 12 months in comparison with splinting, NSAIDs/therapy, and a single steroid injection
-
There is no benefit to routine postoperative immobilization after carpal tunnel release
-
There is no benefit to routine inclusion of the following adjunctive techniques: epineurotomy, neurolysis, flexor tenosynovectomy, and lengthening/reconstruction of the flexor retinaculum (transverse carpal ligament)
-
Buffered lidocaine rather than plain lidocaine should be used for local anesthesia because buffered lidocaine could result in less injection pain
-
There is no additional benefit to routine supervised therapy over home programs in the immediate postoperative period; no evidence meeting the inclusion criteria was found comparing the potential benefit of exercise versus no exercise after surgery
Prognosis
Conservative management
Reported prognosis is widely variable for patients managed conservatively. A systematic review showed that at 3 years, between 1/4 and 2/3 of patients were shown to have a negative outcome (defined as ongoing symptoms, progression of symptoms, or requiring surgery) [17] .
Factors associated with failed nonsurgical management include [15] :
-
Higher initial scores on the Boston Carpal Tunnel Questionnaire (CTQ)-symptom severity scale that do not improve
-
Duration of symptoms greater than or equal to 1 year
-
Positive Phalen test
-
Greater intensity of nighttime symptoms
-
Thenar atrophy
-
More than 1 prior failed nonsurgical intervention.
Surgical management
Regardless of severity, most patients will experience significant symptom improvement within three months of surgery [18] .
For patients with severe disease, based on pre-operative electrodiagnostic studies, time to resolution of symptoms is longer with up to 19% of patients reporting ongoing symptoms at one year [19] .
CTS during pregnancy seems to be less severe than idiopathic CTS and has milder course with fewer cases requiring surgical treatment.
Risks factors for poorer-than-average prognosis include the following [17] :
-
Advanced disease
-
Atypical symptoms (normal nerve conduction studies, symptoms in fifth digit)
-
Longer symptom duration
-
Older age
-
Coexisting disease (diabetes, other peripheral neuropathy)
-
Heavy manual occupation
-
Thenar wasting
-
Positive Phalen's test
-
Carpal tunnel syndrome. Carpal and Guyon tunnels. Drawing showing the proximal level of the carpal tunnel delimited by the pisiform (P) and the scaphoid (S). The flexor retinaculum (medium gray region) forms the roof of the carpal tunnel and the floor of the Guyon tunnel. The palmar carpal ligament (dark gray region) forms the volar boundary of the Guyon tunnel. * = flexor pollicis longus tendon, * = flexor carpi radialis tendon. From Martinoli C, Bianchi S, et al. US of nerve entrapments in osteofibrous tunnels of the upper and lower limbs. Radiographics 2000; 20:S199-S217. Used by permission of the authors and RSNA.
-
Carpal tunnel syndrome. Carpal and Guyon tunnels. Transverse 5-12-MHz ultrasound scan corresponding to the image above shows the proximal level of the carpal tunnel delimited by the pisiform (P) and the scaphoid (S). The flexor tendons and median nerve (MN) extend through the carpal tunnel, with the nerve lying palmar and radial. The flexor retinaculum (open arrowheads) forms the roof of the carpal tunnel and the floor of the Guyon tunnel. At the level of the pisiform, the ulnar nerve (U) courses medial to the ulnar artery (solid arrowhead) within the Guyon tunnel. * = flexor pollicis longus tendon. From Martinoli C, Bianchi S, et al. US of nerve entrapments in osteofibrous tunnels of the upper and lower limbs. Radiographics 2000; 20:S199-S217. Used by permission of the authors and RSNA.
-
Carpal tunnel syndrome. Carpal and Guyon tunnels. Drawing showing the distal level of the carpal tunnel delimited by the hook of the hamate (H) and the tubercle of the trapezium (T). The flexor retinaculum (medium gray region) forms the roof of the carpal tunnel. From Martinoli C, Bianchi S, et al. US of nerve entrapments in osteofibrous tunnels of the upper and lower limbs. Radiographics 2000; 20:S199-S217. Used by permission of the authors and RSNA.
-
Carpal tunnel syndrome. Carpal and Guyon tunnels. Transverse 5-12-MHz ultrasound scan corresponding to the image above shows the distal level of the carpal tunnel delimited by the hook of the hamate (H) and the tubercle of the trapezium (T). The flexor retinaculum (open arrowheads) forms the roof of the carpal tunnel. The flexor tendons and median nerve (MN) extend through the carpal tunnel, with the nerve lying palmar and radial. At the level of the pisiform, the ulnar nerve courses medial to the ulnar artery (solid arrowhead) within the Guyon tunnel. At the level of the hamate, the ulnar nerve divides into two terminal branches, a deep motor branch (curved arrow) and a superficial sensory branch (straight arrow). From Martinoli C, Bianchi S, et al. US of nerve entrapments in osteofibrous tunnels of the upper and lower limbs. * = flexor pollicis longus tendon. Radiographics 2000; 20:S199-S217. Used by permission of the authors and RSNA.
-
Carpal tunnel syndrome. Normal findings on an axial spin-echo T1 MRI of the carpal tunnel showing the intermediate signal intensity of the median nerve (arrow).
-
Carpal tunnel syndrome. Normal findings of isointense-to-hypointense appearance of the median nerve on fast spin-echo T2-weighted MRI (arrow). Note the fairly well-defined nerve fascicles within the median nerve sheath.
-
Carpal tunnel syndrome. Axial fast spin-echo T2-weighted MRI with fat saturation. Note the increased T2-weighted signal within the median nerve (arrow). A slightly increased cross sectional area of the nerve is noted but the nerve architecture is preserved, consistent with early or mild inflammation.
-
Carpal tunnel syndrome. Fast spin-echo T2-weighted MRI illustrates more pronounced increased signal within the median nerve (arrow). Note the small amount of fluid within the carpal tunnel, a secondary sign of inflammation. Slightly less optimal fat saturation is noted than on other images, which is a common occurrence.
-
Carpal tunnel syndrome. Axial fast spin-echo T2-weighted MRI with greater increase in signal and loss of definition within the nerve (arrow). Inflammatory change is noted within the carpal tunnel, adjacent to the flexor digitorum superficialis tendons. The appearance is consistent with pronounced inflammatory change within the carpal tunnel.




