Overview
Neuroimaging has become a key diagnostic tool in the emergency department. Complaints of weakness, dizziness, headache, and trauma lend themselves to rapid evaluation and diagnosis through the use of computed tomography (CT) and magnetic resonance imaging (MRI). This article focuses on the basic principles and key considerations in ordering and interpreting neuroimaging in the emergency department in conjunction with the radiologist.
Trauma is the leading cause of death in patients younger than 45 years. Cranial trauma accounts for a substantial proportion of morbidity and mortality in all age groups and is the leading cause of death in patients younger than 30 years. Accurate, rapid, noninvasive assessment of people with cranial trauma is required for appropriate triage and management.
Approximately 1.4 million people sustain traumatic brain injury (TBI) annually in the United States resulting in more than 50,000 deaths. TBI is twice as likely in men as in women. Children (< 14 y) and elderly persons (>60 y) are at the highest risk for TBI and TBI-related hospitalizations and death, respectively. Child abuse accounts for more than 1 million cases of TBI each year. The overall direct and indirect medical costs including lost productivity and permanent disability from TBI totaled an estimated $60 billion in the United States in 2000. [1, 2] Computed tomography is the diagnostic procedure of choice for acute injury, while magnetic resonance imaging has greater value for evaluation in the subacute and long term.
Although TBI from closed head and penetrating trauma account for the majority of cerebral injuries, other processes, such as acute cerebral infarction (stroke) or subarachnoid hemorrhage (SAH) due to rupture of intracranial aneurysms, may mimic a traumatic injury on presentation and radiologic evaluation.
Another major indication for neuroimaging in the emergency department is stroke. Stroke is the third leading cause of death in the United States behind heart disease and cancer and is the leading cause of long-term disability. [3] An estimated 80-85% of strokes are ischemic (either thrombosis or embolism), whereas 15-20% of strokes are hemorrhagic. Stroke syndromes can present along a wide spectrum of disease from transient ischemic attacks with complete resolution of symptoms to large intracranial hemorrhages with uncal or tonsillar herniation. Rapid evaluation and neuroimaging is standard of care for all patients with suspected strokes and guides the decision to administer thrombolytics, intra-arterial intervention, or medical management. Also see Ischemic Stroke in Emergency Medicine and Hemorrhagic Stroke.
Clinical Presentation
History
See the list below:
-
Age, comorbidities
-
Head trauma
-
Motor vehicle collision
-
Fall/jump from height
-
Assault
-
Penetrating injury
-
Loss of consciousness
-
Headache
-
Changes in vision
-
Changes in strength or sensation
-
Coordination or balance problems
-
Loss of executive function or cognition
-
Seizure
-
Coagulation disorders or therapy
-
Intoxication; history of substance abuse
-
Previous neurosurgery
Physical
See the list below:
-
Altered mental status; unresponsiveness; deficits in Glasgow Coma Scale (see Table 1)
-
Amnesia
-
Depressed skull fracture
-
Penetrating head injury
-
Focal neurologic deficit such as weakness, paresthesia, gait abnormality, aphasia, cranial nerve abnormality
-
Abnormal behavior
-
Hypertension
-
Acute pupillary asymmetry or changes in reactivity
-
Intoxication
Alternate Diagnoses
Acute stroke (embolic/hemorrhagic)
Cardiac syncope
Hypertensive crisis/hemorrhage
Rupture of arteriovenous malformation/aneurysms
Intracranial mass
Seizure; postictal state
Meningitis/encephalitis/systemic infection
Toxic/metabolic disorders
Complex migraine
Diagnostic Workup
Computed tomography scanning
CT is the imaging procedure of choice in evaluation of acutely injured patients or patients with acute neurologic deficit. [4, 5] Quick, easy, reliable, and routinely available, CT is valuable in making a firm diagnosis as well as in excluding alternative diagnoses or the sequelae of other pathology, even in uncooperative patients. Patient monitoring is simple and safe, and CT is compatible with patient stabilization devices. Identification and localization of fractures and bony/metallic fragments are easily achieved, as is the assessment for acute hemorrhage and mass effect. [6, 7, 8]
Primary indications for CT include acute head trauma, suspected acute intracranial hemorrhage, mental status changes, headache, acute neurologic deficits, suspected intracranial infection, suspected hydrocephalus, brain herniation, and suspected mass tumor. In cases in which MRI is primarily indicated but unavailable, contraindicated, or delayed, CT may also be used.
In cases of trauma, CT is recommended in all patients with severe traumatic brain injury (TBI) (Glasgow Coma Scale [GCS] < 8) and moderate TBI (GCS 9-12). In mild TBI (GCS >13), CT is more controversial. Recent studies suggest that high-risk features include GCS less than 15 two hours after the injury, any signs of basal skull fracture (hemotympanum, raccoon eyes, Battle's sign), suspected open or depressed skull fracture, more than 2 episodes of vomiting, or age older than 65 years. Moderate-risk features include dangerous mechanism (fall >3 ft, pedestrian struck by automobile), and amnesia longer than 30 minutes prior to event. [9, 10] However, many providers still recommend that patients who have history of neurosurgery, coagulopathy, and loss of consciousness should also undergo CT. Elderly patients also present a greater risk of TBI and significant intracranial pathology after trauma and are more likely to present with occult injuries. [11]
The routine cranial CT protocol should at minimum include contiguous sections, 5-10 mm thick, from the skull base through the vertex (thinner at base, thicker at vertex) without contrast, reviewed at the following windows widths/levels (in Hounsfield units):
-
Bone: WW 1600-4000, WL 250-400 HU
-
Brain: WW 70-90, WL 25-30 HU
-
Subdural or intermediate: WW 150-200, WL 10-30 HU
Contrast infusion is indicated in the search for mass lesions and vascular pathology (including carotid or vertebral dissection, basilar syndromes), and in patients with a history of human immunodeficiency virus infection and neurological examination abnormalities. [12]
If CT findings are normal, stable patients who experience mild TBI can be discharged safely after a period of clinical observation. In those who experience moderate or severe TBI, a negative CT does not rule out the delayed development of hemorrhage. These patients and patients with a positive CT should undergo a follow-up scan within 24 hours or earlier if symptoms change and/or deteriorate.
Magnetic resource imaging
MRI is valuable in identifying subtle abnormalities on initial and subacute evaluation and in dating injury [13] . MRI is generally better than conventional CT at detecting abnormalities in and progression of posterior fossa and brainstem injuries, child abuse, cortical contusions, and shearing injuries. [14] However, MRI is not as readily available as CT. Appropriate patient monitoring is difficult and unreliable due to strong magnetic fields, time-varying magnetic gradients, and restricted access to the patient. Many newer-generation MRI machines have improved these conditions. Additionally, patients who have cardiac pacemakers, ferromagnetic intracranial aneurysm clips, and certain ferromagnetic foreign bodies or electronic devices or implants should not undergo MRI.
Primary indications for MRI include evaluation of seizures, cranial nerve dysfunction, diplopia, ataxia, acute and chronic neurologic deficits, suspicion of neurodegenerative disease, primary and secondary neoplasm, aneurysm, vasculitis, encephalitis, headache, mental status change, hydrocephalus, ischemic disease and infarction, suspected pituitary dysfunction, inflammation or infection of the brain or meninges or their complications, demyelination and dysmyelination disorders, vascular malformations, and arterial or venous/dural sinus abnormalities. Patients who have cardiac pacemakers, ferromagnetic intracranial aneurysm clips, and certain ferromagnetic foreign bodies or electronic devices or implants should not undergo MRI.
The routine MRI protocol varies considerably based on strength of the unit's field, machine capabilities, and suspected diagnosis. Most centers perform sagittal T1-weighted and axial T1- and T2-weighted sequences of the brain routinely, with the addition of specific additional sequences depending on the clinical indications. T2-weighted gradient echo sequences are more sensitive for subacute/chronic parenchymal hemorrhage/shearing injuries, while fluid-attenuated inversion recovery (FLAIR) sequences have been shown to be more sensitive for subtle subarachnoid blood. Magnetic resonance angiography and venography, diffusion and perfusion imaging, and spectroscopy may all be valuable in selected circumstances. [15]
MRI with diffusion-weighted imaging (DWI) has become more routinely used in the detection of acute stroke because of its improved sensitivity, negative predictive value, and accuracy compared with CT and conventional MRI. [16] MRI with DWI has also been helpful in the detection of the early stages of brain infection such as meningitis, toxoplasmosis, herpes simplex, and West Nile virus.
Conventional catheter angiography
Conventional catheter angiography is the criterion standard in defining pathologic vascular neuroanatomy and can also serve as a treatment modality, but it is limited due to the invasiveness of the procedure. Depending on practice patterns at individual centers, angiography can be indicated in patients with penetrating trauma for examining possible vessel injury, subarachnoid hemorrhage, parenchymal hemorrhage, aneurysm, vascular malformation, thromboembolic/hemorrhagic stroke, veno-occlusive disease, and vasospasm. Relative contraindications include hypotension, severe hypertension, coagulopathy, renal insufficiency, congestive heart failure, and sensitivity to iodinated contrast material. Patients should be stabilized, and tenuous conditions should be corrected prior to study.
Conventional radiography
Due to the advancements and accessibility of imaging technology, conventional radiography generally does not serve a role in the evaluation of the patient with acute head injury unless CT and MRI are unavailable. In cases in which skull radiographs may have been requested in the past, CT can more readily characterize the complexity of soft tissue or bony injuries while simultaneously showing associated intracranial abnormalities. Radiography is not a useful screening tool, and negative findings on skull films do not exclude intracranial injury.
Types of Injury
Epidural hematoma
The dura mater is composed of 2 layers closely invested with each other: the visceral or meningeal layer, which lines the intracranial space, and the parietal layer, which functions as the periosteum fused to the calvarium. The dura, therefore, adheres tightly to the cranial sutures.
A skull fracture that crosses an arterial branch may bleed into the closed space between the calvarium and the periosteal layer, forming a homogeneously high-density lens-shaped or biconvex collection, termed epidural hematoma (EDH) (see the images below). Because of the transmitted arterial pressure, epidural hematoma tends to continue to enlarge, with resultant increasing mass effect. This explains the classic presentation associated with epidural hematoma of an initial loss of consciousness followed by a lucid interval with subsequent neurologic deterioration. However, a lucid interval is present in only 40% of cases and is not pathognomonic for epidural hematoma.
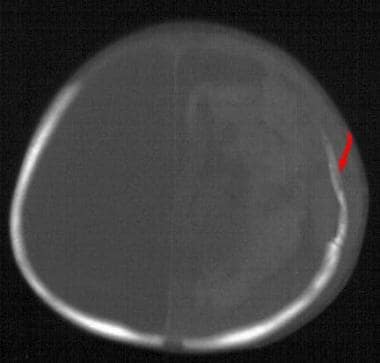
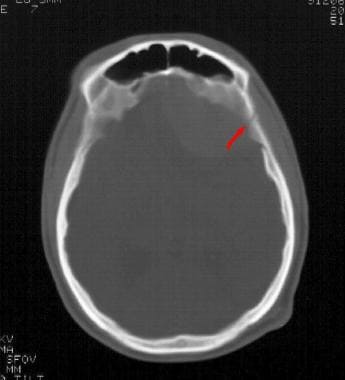 Linear skull fracture - Emergency neuroradiology. Axial CT scan, bone window, shows linear skull fracture through the temporal squamosa (arrow).
Linear skull fracture - Emergency neuroradiology. Axial CT scan, bone window, shows linear skull fracture through the temporal squamosa (arrow).
 Epidural hematoma - Emergency neuroradiology. Axial CT scan, brain window, at the same level as the previous image, shows left frontal epidural hematoma (arrow) displacing the falx and brain posteriorly and to the right.
Epidural hematoma - Emergency neuroradiology. Axial CT scan, brain window, at the same level as the previous image, shows left frontal epidural hematoma (arrow) displacing the falx and brain posteriorly and to the right.
Because of the tightly adherent dura at the cranial sutures, epidural hematomas tend not to cross suture lines, but instead, may cross the falx. Because the dura splits to encase the major venous sinuses and form the falx cerebri and tentorium cerebelli, inward displacement of the superior sagittal or transverse sinus indicates an epidural process. Venous epidural hematomas occur when the fracture disrupts one of the sinuses, and they occur more commonly in the posterior fossa (see the images below).
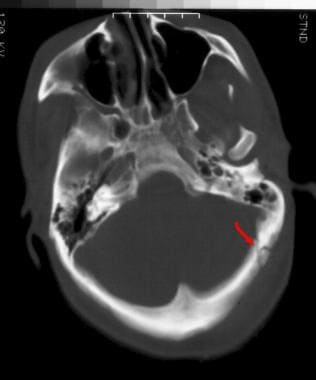 Linear skull fracture - Emergency neuroradiology. Axial CT scan through the posterior fossa shows a linear skull fracture of the occipital bone (arrow), near the sigmoid sinus.
Linear skull fracture - Emergency neuroradiology. Axial CT scan through the posterior fossa shows a linear skull fracture of the occipital bone (arrow), near the sigmoid sinus.
 Subdural hematoma - Emergency neuroradiology. Axial CT scan at the same level as the previous image, brain window, shows venous epidural hematoma (arrow).
Subdural hematoma - Emergency neuroradiology. Axial CT scan at the same level as the previous image, brain window, shows venous epidural hematoma (arrow).
Prognosis is generally good for acute hematomas in conscious patients who undergo immediate surgical correction. Mortality is approximately 5%.
Subdural hematoma
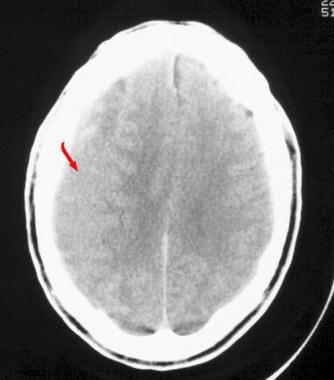
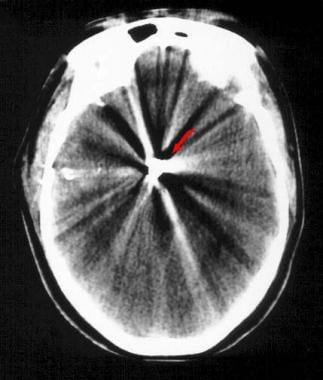
The subdural space is bound externally by the meningeal layer of the dura and internally by the arachnoid mater. Hematomas are confined by the reflected dura of the tentorium and falx but easily spread into the intervening potential space to form crescentic or convex-out/concave-in collections called subdural hematomas (SDHs) (see the image below). Abrupt acceleration/deceleration injury tearing bridging cortical veins that traverse this space accounts for most subdural hematomas. This is more likely to occur in elderly patients and other patients with atrophy, where the subdural space is enlarged.
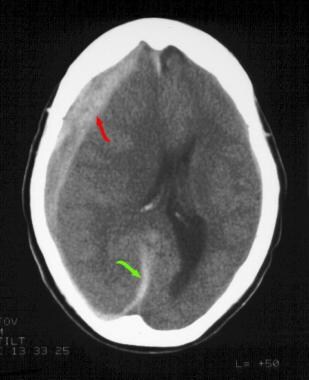 Subdural hematoma - Emergency neuroradiology. Axial CT scan though the level of the lateral ventricles shows right-sided subdural hematoma along the convexity (red arrow) and falx (green arrow), with severe midline shift from right to left.
Subdural hematoma - Emergency neuroradiology. Axial CT scan though the level of the lateral ventricles shows right-sided subdural hematoma along the convexity (red arrow) and falx (green arrow), with severe midline shift from right to left.
Acute hemorrhage is dense on CT with brain windowing, assuming normal hematocrit. As blood ages, it becomes less dense, so that by about 7-10 days, it approximates the same density as adjacent brain tissue. At this stage, the isodense subdural hematoma (see the first image below) is described. Detection requires careful inspection of the subdural or intermediate windowing, which usually shows inward displacement of the cortical gray/white matter junction and mass effect, otherwise unexplained by the imaging findings. Intravenous contrast has been shown to increase detection with enhancement of the bridging veins possibly defining the collection (see the second image below). Homogeneous density within a subdural collection generally represents interval hemorrhage into a preexisting chronic subdural hematoma (SDH).
 Subdural hematoma (noncontrast) - Emergency neuroradiology. Axial CT scan above the lateral ventricles shows extra-axial material (arrow) of approximately the same density as brain parenchyma, displacing the grey-white matter interface internally. Mild midline shift is seen.
Subdural hematoma (noncontrast) - Emergency neuroradiology. Axial CT scan above the lateral ventricles shows extra-axial material (arrow) of approximately the same density as brain parenchyma, displacing the grey-white matter interface internally. Mild midline shift is seen.
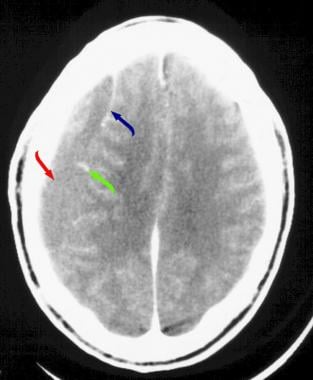 Subdural hematoma (contrast enhanced) - Emergency neuroradiology. Axial CT scan with intravenous contrast infusion, obtained at the same level as the previous image, demonstrates the right isodense subdural hematoma (red arrow), enhancing veins (green arrow), and enhancement of the membrane (blue arrow).
Subdural hematoma (contrast enhanced) - Emergency neuroradiology. Axial CT scan with intravenous contrast infusion, obtained at the same level as the previous image, demonstrates the right isodense subdural hematoma (red arrow), enhancing veins (green arrow), and enhancement of the membrane (blue arrow).
The mortality rate for acute subdural hematoma is 37-57%. Most patients with decreased sensorium have poor outcomes, likely secondary to associated diffuse cerebral brain swelling. In these cases, immediate surgical evacuation does not always improve outcome.
Subarachnoid hemorrhage
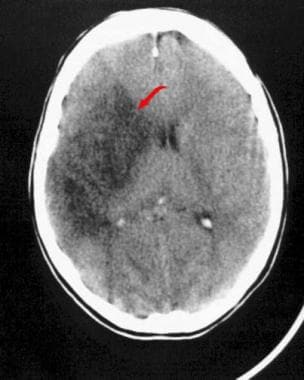
The subarachnoid space extends between the subdural space and the cortical/pia mater surface of the brain. Hemorrhage into this space interdigitates with the sulci and gyri of the brain as seen in traumatic subarachnoid hemorrhage (SAH) (see the first image below). Focal dense clot often signifies the location of hemorrhage, particularly in patients with aneurysm rupture. More subtle or diffuse bleeding is often due to cortical contusion, dilution from a focal collection, or intraventricular hemorrhage due to delayed presentation. Catheter angiography is usually indicated on an emergency basis to identify cerebral aneurysms [17] and to define their anatomy prior to surgical intervention (see the second image below). The prognosis for patients with subarachnoid hemorrhage is variable depending on the extent of injury. Traumatic subarachnoid hemorrhage is common and often associated with other injuries affecting outcome.
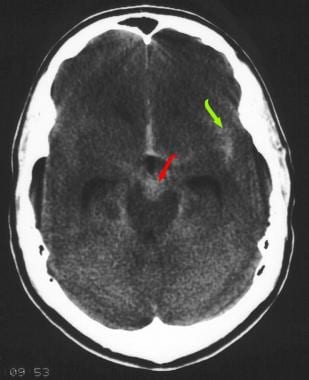 Subarachnoid hemorrhage - Emergency neuroradiology. Axial CT scan at the level of the mesencephalic cistern shows subarachnoid hemorrhage in the left sylvian fissure (green arrow) and the ambient cistern (red arrow). At least part of the density in the ambient cistern represents the aneurysm itself.
Subarachnoid hemorrhage - Emergency neuroradiology. Axial CT scan at the level of the mesencephalic cistern shows subarachnoid hemorrhage in the left sylvian fissure (green arrow) and the ambient cistern (red arrow). At least part of the density in the ambient cistern represents the aneurysm itself.
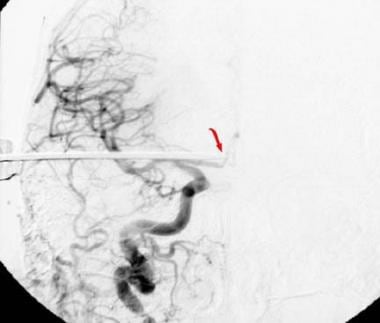
 Cerebral aneurysm - Emergency neuroradiology. Cerebral angiogram, anteroposterior projection, of a left vertebral artery injection demonstrates an aneurysm of the tip of the basilar artery (arrow).
Cerebral aneurysm - Emergency neuroradiology. Cerebral angiogram, anteroposterior projection, of a left vertebral artery injection demonstrates an aneurysm of the tip of the basilar artery (arrow).
Parenchymal lesions
Focal cortical hemorrhage is common as a sequela of head trauma and may be multifocal, as in coup (direct) and contrecoup (indirect) injuries, or diffuse. Focally dense gyri with subjacent edema, particularly those adjacent to the inner calvarial structures (ie, orbit roof-frontal pole, petrous ridge, sphenoid wing-temporal pole) represent contusions (see the images below).
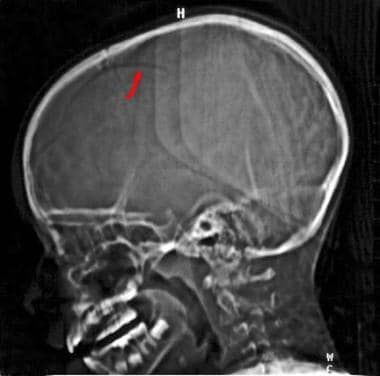 Skull fracture - Emergency neuroradiology. Lateral scout image from a CT brain examination shows linear lucency representing a right posterior frontal skull fracture (arrow).
Skull fracture - Emergency neuroradiology. Lateral scout image from a CT brain examination shows linear lucency representing a right posterior frontal skull fracture (arrow).
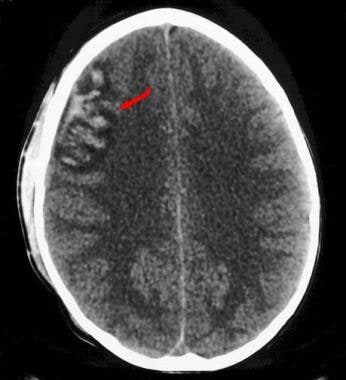 Subarachnoid hemorrhage - Emergency neuroradiology. Axial CT scan of the brain shows a right frontal cortical gyriform contusion, with a small amount of subarachnoid hemorrhage. Right scalp soft tissue swelling is also present (coup lesion).
Subarachnoid hemorrhage - Emergency neuroradiology. Axial CT scan of the brain shows a right frontal cortical gyriform contusion, with a small amount of subarachnoid hemorrhage. Right scalp soft tissue swelling is also present (coup lesion).
Diffuse axonal injury (DAI) is caused by shearing of the white matter, often at the gray-white junction. This is thought to be due to the differing tissue density or fixation between two structures in differing response to rotation, acceleration, and deceleration. Detection is often associated with changes in the lobar white matter, brainstem, and corpus callosum with ovoid or elongated regions of decreased density. Patients usually present with severe impairment of consciousness from the moment of impact. MRI (FLAIR or T2 weighted) is most useful in defining the extent of axonal shearing and nonhemorrhagic injury. CT results are often negative, but acute areas of petechial hemorrhage have been seen in early stages. Diffuse axonal injury (DAI) is one of the most common injuries resulting in long-term severe disability and vegetative state.
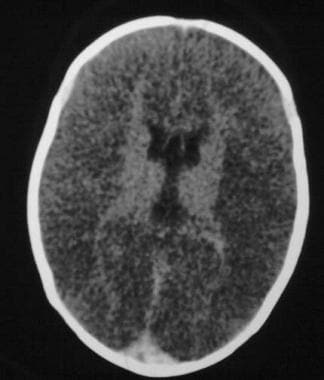
Cerebral edema may result from loss of normal autoregulation and hyperemia, diffuse edema from infectious causes, or mass lesions from cancer. With generalized edema, diffuse loss of normal sulci and cisterns with small ventricles is noted (see the images below). Mass effect, increased intracranial pressure, ischemia, and herniation contribute to poor outcomes. Children are most commonly affected; they have a 50% mortality rate, 3 times that of adults. Most commonly, this may be seen in the shaken baby syndrome and other TBI in children. As mentioned above, intravenous contrast infusion is useful to distinguish mass lesions and infectious foci with localized surrounding edema. MRI is more sensitive than CT for subtle injuries of these types, especially in the subacute or chronic phases.
 Diffuse axonal injury - Emergency neuroradiology. Axial CT scan, brain window, shows diffuse low density and loss of grey-white matter differentiation throughout the cerebral hemispheres (arrows), consistent with diffuse edema and swelling.
Diffuse axonal injury - Emergency neuroradiology. Axial CT scan, brain window, shows diffuse low density and loss of grey-white matter differentiation throughout the cerebral hemispheres (arrows), consistent with diffuse edema and swelling.
 Diffuse axonal hemorrhage - Emergency neuroradiology. Axial CT scan, 24-hour follow-up postictus, demonstrates progression of swelling and diffuse edema.
Diffuse axonal hemorrhage - Emergency neuroradiology. Axial CT scan, 24-hour follow-up postictus, demonstrates progression of swelling and diffuse edema.
Herniation syndromes
Herniation syndrome can develop as a major consequence of any of the aforementioned primary brain injuries. The cranial vault is divided into multiple compartments by bone and dura. When a primary injury develops and expands pressure is applied to contiguous structures adjacent to the displacing injury. Elevation in cranial pressure adds to the demise of the patient. Medical and surgical control of increasing intracranial pressure is of ultimate priority. (See Brain Herniation Imaging.)
Parenchymal hemorrhage
Focal parenchymal hematomas occurring in regions of end-arteries, such as the basal ganglia, thalamus, brainstem, and cerebellar hemispheres, occur most frequently in patients with chronic hypertension or hypertensive crisis, probably due to spontaneous rupture of these tiny vessels. Fewer than 1% of such patients have a radiographically definable lesion; thus, angiography is rarely indicated (see the image below).
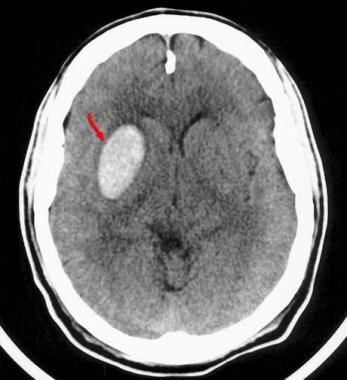 Parenchymal hemorrhage - Emergency neuroradiology. Axial CT scan shows sharply defined oval hyperdensity in the right lentiform nucleus (arrow) representing an acute hypertensive-type hemorrhage. Minimal edema is present in this acute setting.
Parenchymal hemorrhage - Emergency neuroradiology. Axial CT scan shows sharply defined oval hyperdensity in the right lentiform nucleus (arrow) representing an acute hypertensive-type hemorrhage. Minimal edema is present in this acute setting.
Focal lobar parenchymal hematomas, by contrast, are far more likely to be secondary to a structural lesion, often an arteriovenous malformation (AVM), vasculitis, or mass lesion (see the first image below). If an appropriate clinical history has been obtained, angiography (AVM) or contrast-enhanced MRI is the diagnostic procedure of choice prior to surgical intervention, unless secondary mass effect is life threatening and patient management decisions dictate otherwise (see the second image below).
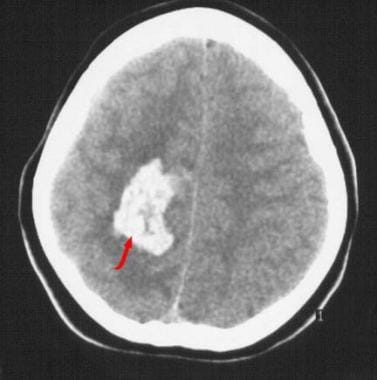 Parenchymal hemorrhage - Emergency neuroradiology. Axial CT scan shows irregularly shaped right frontoparietal acute parenchymal hemorrhage (arrow).
Parenchymal hemorrhage - Emergency neuroradiology. Axial CT scan shows irregularly shaped right frontoparietal acute parenchymal hemorrhage (arrow).
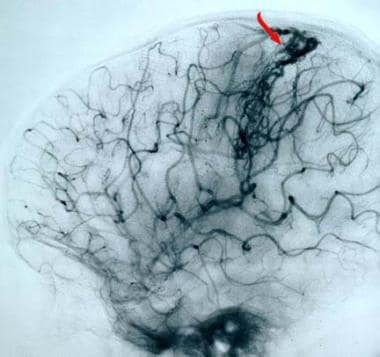 Arteriovenous malformation - Emergency neuroradiology. Cerebral angiogram, lateral projection, of a right internal carotid artery injection demonstrates a right frontoparietal arteriovenous malformation (AVM), with prominent early draining veins (arrow) extending cephalad to the superior sagittal sinus from the AVM nidus. (The patient is facing to the left.)
Arteriovenous malformation - Emergency neuroradiology. Cerebral angiogram, lateral projection, of a right internal carotid artery injection demonstrates a right frontoparietal arteriovenous malformation (AVM), with prominent early draining veins (arrow) extending cephalad to the superior sagittal sinus from the AVM nidus. (The patient is facing to the left.)
Ischemic stroke
Patients with ischemic stroke in the emergency setting may present a different course for decision-making. Ischemic stroke secondary to trauma is either due to vertebral artery dissection or carotid artery dissection. Risk factors for these injuries include penetrating trauma, C1-3 fractures, chiropractor manipulation, and possibly bruising to the neck from seatbelts. In ischemic stoke, acute (12-48 h) occlusion of one or more large vessels results in focal, wedge-shaped peripheral areas of loss of grey/white matter differentiation involving the cortex and contiguous white matter, or simply as a focal mass effect (see the image below). Anoxia or hypotension results in diffuse loss of gyral/cortical markings and diffuse mass effect.
 MCA stroke - Emergency neuroradiology. Axial CT scan shows a peripheral wedge-shaped area of decreased density (arrow) involving the right caudate head and lentiform nuclei, insula, and frontal and temporal lobes, consistent with a subacute right proximal middle cerebral artery occlusion and subsequent cerebrovascular infarction. A mild mass effect and shift of the midline to the left is shown.
MCA stroke - Emergency neuroradiology. Axial CT scan shows a peripheral wedge-shaped area of decreased density (arrow) involving the right caudate head and lentiform nuclei, insula, and frontal and temporal lobes, consistent with a subacute right proximal middle cerebral artery occlusion and subsequent cerebrovascular infarction. A mild mass effect and shift of the midline to the left is shown.
Such changes are exceedingly difficult to appreciate on noncontrast CT studies obtained hyperacutely (< 6-12 h from ictus). One exception is the dense middle cerebral artery (MCA) sign, which represents acute clot within the horizontal portion of the middle cerebral artery (see the image below). Patients with resolved neurologic deficits (ie, transient ischemic attacks) rarely demonstrate acute pathology on CT examinations without having sustained acute trauma. MRI with DWI techniques allows earlier identification and diagnosis in less than 30 minutes from initial insult with changes up to 2 weeks. [18]
 MCA stroke - Emergency neuroradiology. Axial CT scan at the level of the basal cisterns shows the "hyperdense middle cerebral artery (MCA) sign" (arrow) representing acute clot within the right middle cerebral artery, accounting for the patient's clinical symptoms.
MCA stroke - Emergency neuroradiology. Axial CT scan at the level of the basal cisterns shows the "hyperdense middle cerebral artery (MCA) sign" (arrow) representing acute clot within the right middle cerebral artery, accounting for the patient's clinical symptoms.
The emergent use of MRI in stroke is still being defined. Brain injury protocols have shown excellent results in treating such patients with intravenous (< 3 h) or intra-arterial (< 6 h) thrombolytic agents. More recent studies even suggest that treatment with thrombolytics as far as 4.5 hours out from onset of stroke may be safe and effective. [19] (See Ischemic Stroke in Emergency Medicine.)
Child abuse
Child abuse merits specific mention because of the severe morbidity and mortality of cranial injuries inflicted in abusive settings and because of the possibility of intervention to spare other household members further trauma. The key to diagnosis of child abuse is repeated injury, which is present in the majority of victims. Presence of hemorrhages of various ages and locations is pathognomonic (see the images below). Retinal hemorrhages, rib and long bone fractures, burns, and other skin lesions are common. MRI is ideal for the evaluation of such patients because of its superior sensitivity and ability to date the injuries with accuracy. It further offers the benefit of not using ionizing radiation. [20]
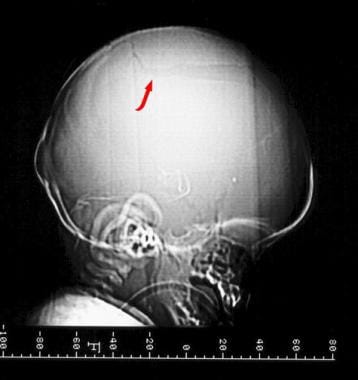 Skull fracture - Emergency neuroradiology. Lateral scout image from a CT brain examination shows linear lucency representing a left parietal skull fracture.
Skull fracture - Emergency neuroradiology. Lateral scout image from a CT brain examination shows linear lucency representing a left parietal skull fracture.
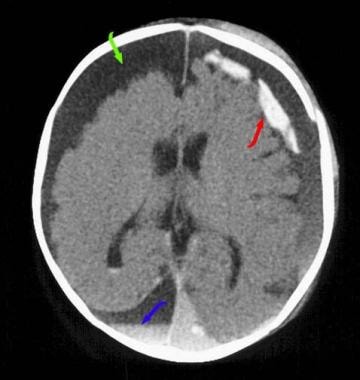 Child abuse - Emergency neuroradiology. Axial CT scan of the brain shows multiple hemorrhages of multiple ages, pathognomonic for child abuse. Hyperdense hemorrhage is seen in several left-sided chronic subdural loculations (red arrow). Right extra-axial fluid collection exerts mass effect (green arrow) and indicates prior, chronic subdural hematoma/hygroma, with acute hemorrhage dependently (blue arrow shows desaete layering). Also, a small amount of interventricular blood is present in the atrium of the right lateral ventricle.
Child abuse - Emergency neuroradiology. Axial CT scan of the brain shows multiple hemorrhages of multiple ages, pathognomonic for child abuse. Hyperdense hemorrhage is seen in several left-sided chronic subdural loculations (red arrow). Right extra-axial fluid collection exerts mass effect (green arrow) and indicates prior, chronic subdural hematoma/hygroma, with acute hemorrhage dependently (blue arrow shows desaete layering). Also, a small amount of interventricular blood is present in the atrium of the right lateral ventricle.
 Skull fracture - Emergency neuroradiology. Axial CT scan of the brain with bone windowing at a higher level shows the left parietal skull fracture (arrow) seen on the "scout" image. Absence of bone anteriorly is the anterior fontanel, with visualization of the posterior portion of the sagittal suture noted in the midline posteriorly.
Skull fracture - Emergency neuroradiology. Axial CT scan of the brain with bone windowing at a higher level shows the left parietal skull fracture (arrow) seen on the "scout" image. Absence of bone anteriorly is the anterior fontanel, with visualization of the posterior portion of the sagittal suture noted in the midline posteriorly.
Penetrating trauma
CT is the diagnostic procedure of choice for patients with gunshot wounds and other penetrating trauma. The course of the projectile may be identified, and the location of foreign bodies can be noted. Hematomas and mass effect are easily assessed (see the images below). Angiography may also aid in the diagnosis and treatment of vascular disruptions from penetrating trauma.
 Penetrating trauma - Emergency neuroradiology. Lateral scout image from a CT scan of the brain shows a metal bullet overlying the expected location of the suprasellar cistern.
Penetrating trauma - Emergency neuroradiology. Lateral scout image from a CT scan of the brain shows a metal bullet overlying the expected location of the suprasellar cistern.
 Penetrating trauma - Emergency neuroradiology. Axial CT scan of the brain at the level of the suprasellar cistern shows severe streak artifact from the hyperdense metal bullet (arrow). The bullet entered from a right temporal location (right temporalis muscle swelling) and traveled to the midline (linear horizontal hyperdensity).
Penetrating trauma - Emergency neuroradiology. Axial CT scan of the brain at the level of the suprasellar cistern shows severe streak artifact from the hyperdense metal bullet (arrow). The bullet entered from a right temporal location (right temporalis muscle swelling) and traveled to the midline (linear horizontal hyperdensity).
 Penetrating trauma - Emergency neuroradiology. Lateral scout image from a CT scan of the brain shows linear metal ice pick (arrow at ice pick point in the suprasellar cistern) overlying the anterior cranial fossa.
Penetrating trauma - Emergency neuroradiology. Lateral scout image from a CT scan of the brain shows linear metal ice pick (arrow at ice pick point in the suprasellar cistern) overlying the anterior cranial fossa.
 Penetrating trauma - Emergency neuroradiology. Axial CT scan of the brain at the level of the suprasellar cistern shows the path of the distal portion of the ice pick (arrow), extending the suprasellar cistern in the midline. This is the expected location for the internal carotid artery bifurcation.
Penetrating trauma - Emergency neuroradiology. Axial CT scan of the brain at the level of the suprasellar cistern shows the path of the distal portion of the ice pick (arrow), extending the suprasellar cistern in the midline. This is the expected location for the internal carotid artery bifurcation.
Table 1
Glasgow Coma Scale: GCS is a common tool used to access the grade and the progression of head injury over time and multiple observers.
Table. Glasgow Coma Scale (Open Table in a new window)
Eye opening |
|
4 |
Spontaneously |
3 |
To verbal command |
2 |
To pain |
1 |
None |
Verbal stimuli |
|
5 |
Oriented, converses |
4 |
Disoriented, converses |
3 |
Inappropriate words |
2 |
Incomprehensible; moans |
1 |
No response |
Motor response |
|
6 |
Obeys verbal commands |
5 |
Localizes to painful stimuli; removes pain |
4 |
Flexion withdrawal; pulls away from pain |
3 |
Abnormal flexion; decorticate rigidity |
2 |
Extension; decerebrate rigidity |
1 |
No response; hypotonic; flaccid |
-
Linear skull fracture - Emergency neuroradiology. Axial CT scan, bone window, shows linear skull fracture through the temporal squamosa (arrow).
-
Epidural hematoma - Emergency neuroradiology. Axial CT scan, brain window, at the same level as the previous image, shows left frontal epidural hematoma (arrow) displacing the falx and brain posteriorly and to the right.
-
Linear skull fracture - Emergency neuroradiology. Axial CT scan through the posterior fossa shows a linear skull fracture of the occipital bone (arrow), near the sigmoid sinus.
-
Subdural hematoma - Emergency neuroradiology. Axial CT scan at the same level as the previous image, brain window, shows venous epidural hematoma (arrow).
-
Subdural hematoma - Emergency neuroradiology. Axial CT scan though the level of the lateral ventricles shows right-sided subdural hematoma along the convexity (red arrow) and falx (green arrow), with severe midline shift from right to left.
-
Subdural hematoma (noncontrast) - Emergency neuroradiology. Axial CT scan above the lateral ventricles shows extra-axial material (arrow) of approximately the same density as brain parenchyma, displacing the grey-white matter interface internally. Mild midline shift is seen.
-
Subdural hematoma (contrast enhanced) - Emergency neuroradiology. Axial CT scan with intravenous contrast infusion, obtained at the same level as the previous image, demonstrates the right isodense subdural hematoma (red arrow), enhancing veins (green arrow), and enhancement of the membrane (blue arrow).
-
Subarachnoid hemorrhage - Emergency neuroradiology. Axial CT scan at the level of the mesencephalic cistern shows subarachnoid hemorrhage in the left sylvian fissure (green arrow) and the ambient cistern (red arrow). At least part of the density in the ambient cistern represents the aneurysm itself.
-
Cerebral aneurysm - Emergency neuroradiology. Cerebral angiogram, anteroposterior projection, of a left vertebral artery injection demonstrates an aneurysm of the tip of the basilar artery (arrow).
-
Skull fracture - Emergency neuroradiology. Lateral scout image from a CT brain examination shows linear lucency representing a right posterior frontal skull fracture (arrow).
-
Subarachnoid hemorrhage - Emergency neuroradiology. Axial CT scan of the brain shows a right frontal cortical gyriform contusion, with a small amount of subarachnoid hemorrhage. Right scalp soft tissue swelling is also present (coup lesion).
-
Diffuse axonal injury - Emergency neuroradiology. Axial CT scan, brain window, shows diffuse low density and loss of grey-white matter differentiation throughout the cerebral hemispheres (arrows), consistent with diffuse edema and swelling.
-
Diffuse axonal hemorrhage - Emergency neuroradiology. Axial CT scan, 24-hour follow-up postictus, demonstrates progression of swelling and diffuse edema.
-
Parenchymal hemorrhage - Emergency neuroradiology. Axial CT scan shows sharply defined oval hyperdensity in the right lentiform nucleus (arrow) representing an acute hypertensive-type hemorrhage. Minimal edema is present in this acute setting.
-
Parenchymal hemorrhage - Emergency neuroradiology. Axial CT scan shows irregularly shaped right frontoparietal acute parenchymal hemorrhage (arrow).
-
Arteriovenous malformation - Emergency neuroradiology. Cerebral angiogram, lateral projection, of a right internal carotid artery injection demonstrates a right frontoparietal arteriovenous malformation (AVM), with prominent early draining veins (arrow) extending cephalad to the superior sagittal sinus from the AVM nidus. (The patient is facing to the left.)
-
MCA stroke - Emergency neuroradiology. Axial CT scan shows a peripheral wedge-shaped area of decreased density (arrow) involving the right caudate head and lentiform nuclei, insula, and frontal and temporal lobes, consistent with a subacute right proximal middle cerebral artery occlusion and subsequent cerebrovascular infarction. A mild mass effect and shift of the midline to the left is shown.
-
MCA stroke - Emergency neuroradiology. Axial CT scan at the level of the basal cisterns shows the "hyperdense middle cerebral artery (MCA) sign" (arrow) representing acute clot within the right middle cerebral artery, accounting for the patient's clinical symptoms.
-
Skull fracture - Emergency neuroradiology. Lateral scout image from a CT brain examination shows linear lucency representing a left parietal skull fracture.
-
Child abuse - Emergency neuroradiology. Axial CT scan of the brain shows multiple hemorrhages of multiple ages, pathognomonic for child abuse. Hyperdense hemorrhage is seen in several left-sided chronic subdural loculations (red arrow). Right extra-axial fluid collection exerts mass effect (green arrow) and indicates prior, chronic subdural hematoma/hygroma, with acute hemorrhage dependently (blue arrow shows desaete layering). Also, a small amount of interventricular blood is present in the atrium of the right lateral ventricle.
-
Skull fracture - Emergency neuroradiology. Axial CT scan of the brain with bone windowing at a higher level shows the left parietal skull fracture (arrow) seen on the "scout" image. Absence of bone anteriorly is the anterior fontanel, with visualization of the posterior portion of the sagittal suture noted in the midline posteriorly.
-
Penetrating trauma - Emergency neuroradiology. Lateral scout image from a CT scan of the brain shows a metal bullet overlying the expected location of the suprasellar cistern.
-
Penetrating trauma - Emergency neuroradiology. Axial CT scan of the brain at the level of the suprasellar cistern shows severe streak artifact from the hyperdense metal bullet (arrow). The bullet entered from a right temporal location (right temporalis muscle swelling) and traveled to the midline (linear horizontal hyperdensity).
-
Penetrating trauma - Emergency neuroradiology. Lateral scout image from a CT scan of the brain shows linear metal ice pick (arrow at ice pick point in the suprasellar cistern) overlying the anterior cranial fossa.
-
Penetrating trauma - Emergency neuroradiology. Axial CT scan of the brain at the level of the suprasellar cistern shows the path of the distal portion of the ice pick (arrow), extending the suprasellar cistern in the midline. This is the expected location for the internal carotid artery bifurcation.
-
Angiography - Emergency neuroradiology. Anteroposterior projection of a right common carotid artery angiogram shows the close proximity of the ice pick (arrow) and the internal carotid artery bifurcation into the anterior and middle cerebral arteries.