Background
Carotid artery dissection begins as a tear in one of the carotid arteries of the neck, which allows blood under arterial pressure to enter the wall of the artery and split its layers. The result is either an intramural hematoma or an aneurysmal dilatation, either of which can be a source of microemboli, with the latter also causing a mass effect on surrounding structures.
Carotid artery dissection is a significant cause of ischemic stroke in all age groups, but it occurs most frequently in the fifth decade of life and accounts for a much larger percentage of strokes in young patients. [1] Dissection of the internal carotid artery can occur intracranially or extracranially, with the latter being more frequent. Internal carotid artery dissection can be caused by major or minor trauma, or it can be spontaneous, in which case, genetic, familial, or heritable disorders are likely etiologies.
Although in practice, dissections are labeled spontaneous in the absence of major blunt or penetrating trauma, [2] when they are associated with minor mechanism trauma they may be caused or influenced by an underlying arteriopathy. [3] Patients can present in a variety of settings, such as a trauma bay with multiple traumatic injuries; a physician’s office with nonspecific head, neck, or face pain; or an emergency department (ED) with a partial Horner syndrome. [4]
Sophisticated imaging techniques, which have improved over the past two decades, are required to confirm the presence of dissection. Most ischemic cerebral symptoms arise from thromboembolic events; therefore, early institution of antithrombotic treatment provides the best outcome. [5]
Once diagnosed and treated, patients with carotid artery dissection require regular follow-up and imaging studies of both carotid arteries. Healing usually takes 3-6 months, and the incidence of contralateral dissection is higher in these patients than in the general population. When the condition is diagnosed early, the prognosis is usually good. A high index of suspicion is required to make this difficult diagnosis.
For patient education resources, see the Brain & Nervous System Center, as well as Worst Headache of Your Life, Transient Ischemic Attack (TIA, Mini-Stroke), and Stroke.
Pathophysiology
Although the cause of internal carotid artery dissection remains elusive, mechanical forces (eg, trauma, blunt injury, and stretching) and underlying arteriopathies (eg, Ehlers-Danlos syndrome IV [6] and other connective tissue disorders and aberrations), either alone or in combination, account for most of the pathophysiology. It is widely accepted that carotid artery dissection is a multifactorial disease. [7]
Carotid artery dissection begins as a tear in the tunica intima or directly within the tunica media (possibly originating from the vasa vasorum). [1] The blood dissects along the artery to create an intramural hematoma that leads to a thrombus, which can narrow the carotid artery lumen and become a nidus for distal embolization (see the image below). [2]
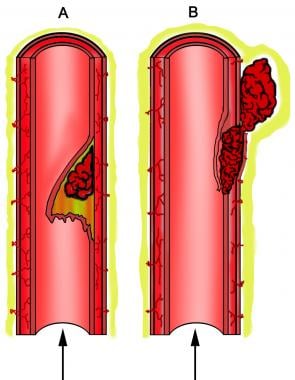 Arterial dissection. (A) Tear and elevation of intima from wall of artery, resulting in luminal stenosis. Illustration shows stasis of flow in false lumen beneath elevated intima. This condition creates blind pouch that predisposes patient to thrombus formation. (B) Subadventitial dissection represents hemorrhage between media and adventitia. Artery may become dilated as result of thickening of arterial wall, with some degree of luminal narrowing. Elevation of intimal flap is not commonly associated with this type of dissection. Hemorrhage may extravasate through adventitia, resulting in pseudoaneurysm or fistula formation.
Arterial dissection. (A) Tear and elevation of intima from wall of artery, resulting in luminal stenosis. Illustration shows stasis of flow in false lumen beneath elevated intima. This condition creates blind pouch that predisposes patient to thrombus formation. (B) Subadventitial dissection represents hemorrhage between media and adventitia. Artery may become dilated as result of thickening of arterial wall, with some degree of luminal narrowing. Elevation of intimal flap is not commonly associated with this type of dissection. Hemorrhage may extravasate through adventitia, resulting in pseudoaneurysm or fistula formation.
Sometimes, the dissection plane lies between the tunica media and the tunica adventitia, resulting in an aneurysmal outpouching of the arterial wall that may also become a source of distal emboli. Aneurysmal dilatation can also cause a mass effect on nearby structures such as sympathetic fibers and the lower cranial nerves. [1, 2] The dilatation resulting from an internal carotid artery dissection may be termed a true rather than a false aneurysm because the wall is composed of blood vessel elements.
Etiology
Causes of carotid artery dissection include the following:
-
Heritable connective-tissue disorders
-
Ehlers-Danlos syndrome type IV
-
Cystic medial necrosis
-
Autosomal dominant polycystic kidney disease
-
Oral contraceptives
-
Hypertension
-
Neck manipulation or strain - This can result from intentional manipulation or from other strain that may occur during sports activities, yoga, or even apparently minimal activity (eg, overhead painting)
-
Blunt trauma from high impact and seemingly minor mechanisms of injury
-
Penetrating trauma
-
Wearing a three-point restraint seat belt during a motor vehicle crash
-
Smoking
-
Respiratory tract infection
Epidemiology
The annual incidence of symptomatic spontaneous internal carotid artery dissection is 2.5-3 per 100,000. [1] The incidence of carotid artery dissection as a result of blunt injuries (mainly high-speed motor vehicle accidents) ranges from less than 1% to 3%. [8] The actual incidence may be higher; some dissections are asymptomatic or cause only minor transient symptoms and remain undiagnosed.
Age- and sex-related demographics
Internal carotid artery dissection is a common cause of ischemic stroke in patients younger than 50 years and accounts for as many as 25% of ischemic strokes in young and middle-aged patients. [1] The mean age for ischemic stroke secondary to internal carotid artery dissection from blunt traumatic injury is even younger: 35-38 years. Dissection of the intracranial part of the internal carotid artery is rare at any age, because the intracranial carotid artery is less mobile and the skull absorbs most of the force of trauma.
No significant gender-based difference in frequency exists for spontaneous internal carotid artery dissection, though there may be a slight male preponderance when traumatic causes of carotid artery dissection are taken into account.
Prognosis
In general, the prognosis depends on the severity of the initial ischemic injury and the extent of collateral circulation. Overall, the prognosis for spontaneous internal carotid artery dissection is favorable, with about 75% of patients making a good recovery. [1, 9] The reported mortality is less than 5%. Patients who have a dissection secondary to trauma have a much higher mortality on discharge.
Morbidity from carotid artery dissection ranges in severity from transient focal deficits to permanent cerebral or retinal ischemic injury. More than one half of patients with spontaneous carotid artery dissection develop stroke, [1] though this may be delayed by hours or days. Rates of delayed stroke due to blunt-traumatic causes of carotid artery injury range from 3% in grade I injuries to 44% in grade IV injuries. [2]
In the setting of blunt trauma, 37-58% of patients have permanent neurologic deficits on discharge, [8] though early use of antithrombotic therapy has essentially eliminated ischemic events in asymptomatic patients with carotid artery dissection. [5, 10]
As with other causes of stroke in young adults, the functional outcome is generally good, and recurrence of cerebral ischemia and carotid artery dissection is rare. [7] The risk of recurrence is highest in the first month and then remains in the area of 1% per year for about a decade. Headache may persist, in some cases for years after the dissection.
-
Arterial dissection. (A) Tear and elevation of intima from wall of artery, resulting in luminal stenosis. Illustration shows stasis of flow in false lumen beneath elevated intima. This condition creates blind pouch that predisposes patient to thrombus formation. (B) Subadventitial dissection represents hemorrhage between media and adventitia. Artery may become dilated as result of thickening of arterial wall, with some degree of luminal narrowing. Elevation of intimal flap is not commonly associated with this type of dissection. Hemorrhage may extravasate through adventitia, resulting in pseudoaneurysm or fistula formation.









