Introduction to Ventilator Management
Intubation, with subsequent mechanical ventilation, is a common life-saving intervention in the emergency department (ED). Given the increasing length of stay of ventilated patients in EDs, it is necessary for emergency practitioners to have a good understanding of techniques to optimize mechanical ventilation and minimize complications.
Many different strategies of positive-pressure ventilation are available; these are based on various permutations of triggered volume-cycled and pressure-cycled ventilations and are delivered at a range of rates, volumes, and pressures. Poor ventilatory management can inflict serious pulmonary and extrapulmonary damage that may not be immediately apparent.
Because many of the effects of ventilator-induced lung injury are delayed and not seen while patients are in the ED, much of our understanding of the adverse consequences of volutrauma, air-trapping, barotrauma, and oxygen toxicity has come from the critical care literature. While the fundamental principles underlying mechanical ventilatory support have changed little over the decades, much progress has been made in our understanding of the secondary pathophysiologic changes associated with positive-pressure ventilation.
Ventilatory strategies have been devised for different disease processes to protect pulmonary parenchyma while maintaining adequate gas exchange, and they may be responsible for the increased rates of survival for pathologies such as acute respiratory distress syndrome (ARDS). Several recent clinical trials have demonstrated that optimizing ventilatory parameters reduces overall duration of mechanical ventilation and organ failure. Additionally, an upsurge in utilization of noninvasive ventilation has permitted many patients to avoid the risks and complications of tracheal intubation. [1, 2]
Modes of Mechanical Ventilation
Volume-cycled mode
Inhalation proceeds until a set tidal volume (TV) is delivered and is followed by passive exhalation. A feature of this mode is that gas is delivered with a constant inspiratory flow pattern, resulting in peak pressures applied to the airways higher than that required for lung distension (plateau pressure). Since the volume delivered is constant, applied airway pressures vary with changing pulmonary compliance (plateau pressure) and airway resistance (peak pressure).
Because the volume-cycled mode ensures a constant minute ventilation despite potentially abnormal lung compliance, it is a common choice as an initial ventilatory mode in the ED. A major disadvantage is that high airway pressures may be generated, potentially resulting in barotrauma. Close monitoring and use of pressure limits are helpful in avoiding this problem. Note that ventilators set to volume-cycled mode function well as monitors of patients' pulmonary compliance, which will be decreased in physiological states such as worsening ARDS, pneumothorax, right mainstem intubation, chest-wall rigidity, increased intra-abdominal pressure, and psychomotor agitation ("fighting the vent"). These pathophysiological states increase peak pressure and should be considered whenever pressure alarms are sounded.
In pressure-cycled settings, by contrast, such states result only in reduced delivered volumes and may not trigger alarms. Given that the airway resistance and pulmonary compliance of the critical ED patient is unknown, the authors recommend the volume-cycled mode for initial ventilation of most patients.
Pressure-cycled mode
A set peak inspiratory pressure (PIP) is applied, and the pressure difference between the ventilator and the lungs results in inflation until the peak pressure is attained and passive exhalation follows. The delivered volume with each respiration is dependent on the pulmonary and thoracic compliance.
A theoretical advantage of pressure-cycled modes is a decelerating inspiratory flow pattern, in which inspiratory flow tapers off as the lung inflates. This usually results in a more homogeneous gas distribution throughout the lungs. However, no definite evidence exists that this results in a reduction of the rate of ventilator-induced lung injury or overall mortality. Nevertheless, pressure-cycled ventilation has achieved considerable popularity in the intensive care setting for management of patients with ARDS, whose lungs are most likely to be characterized by a broad range of alveolar dysfunction and are also most vulnerable to the effects of barotrauma and volutrauma.
A major disadvantage is that dynamic changes in pulmonary mechanics may result in varying tidal volumes. This necessitates close monitoring of minute ventilation and limits the usefulness of this mode in many emergency department patients. However, newer ventilators can provide volume-assured pressure-cycled ventilation, which increase peak pressures as needed to deliver a preset minimum tidal volume.
High-frequency oscillatory support
In this ventilatory strategy, ultra-high respiratory rates (180-900 breaths per minute) are coupled with tiny tidal volumes (1-4 mL/kg) and high airway pressures (25-30 mm water). [3] This is a commonly accepted ventilatory setting for premature infants and has now also been used in small critical care unit studies on patients with ARDS, with reports of improving oxygenation and lung recruitment. [4, 5]
While this setting cannot currently be recommended for routine ED use, it may in the future be found appropriate for the management of patients with ARDS.
Types of support
Most ventilators can be set to apply the delivered tidal volume in a control mode or a support mode.
Control mode
In control mode, the ventilator delivers the preset tidal volume once it is triggered regardless of patient effort. If the patient is apneic or possesses limited respiratory drive, control mode can ensure delivery of appropriate minute ventilation.
Support mode
In support mode, the ventilator provides inspiratory assistance through the use of an assist pressure. The ventilator detects inspiration by the patient and supplies an assist pressure during inspiration. It terminates the assist pressure upon detecting onset of the expiratory phase. Support mode requires an adequate respiratory drive. The amount of assist pressure can be dialed in.
Methods of Ventilatory Support
Continuous mandatory ventilation
Breaths are delivered at preset intervals, regardless of patient effort. This mode is used most often in the paralyzed or apneic patient because it can increase the work of breathing if respiratory effort is present. Continuous mandatory ventilation (CMV) has given way to assist-control (A/C) mode because A/C with the apneic patient is tantamount to CMV. Many ventilators do not have a true CMV mode and offer A/C instead.
Assist-control ventilation
The ventilator delivers preset breaths in coordination with the respiratory effort of the patient. With each inspiratory effort, the ventilator delivers a full assisted tidal volume. Spontaneous breathing independent of the ventilator between A/C breaths is not allowed. As might be expected, this mode is better tolerated than CMV in patients with intact respiratory effort.
Intermittent mandatory ventilation
With intermittent mandatory ventilation (IMV), breaths are delivered at a preset interval, and spontaneous breathing is allowed between ventilator-administered breaths. Spontaneous breathing occurs against the resistance of the airway tubing and ventilator valves, which may be formidable. This mode has given way to synchronous intermittent mandatory ventilation (SIMV).
Synchronous intermittent mandatory ventilation
The ventilator delivers preset breaths in coordination with the respiratory effort of the patient. Spontaneous breathing is allowed between breaths. Synchronization between preset mandatory breaths and the patient's spontaneous breaths attempts to limit barotrauma that may occur with IMV when a preset breath is delivered to a patient who is already maximally inhaled (breath stacking) or is forcefully exhaling. One disadvantage of SIMV is increased work of breathing, though this may be mitigated by adding pressure support on top of spontaneous breaths.
The initial choice of ventilation mode (eg, SIMV, A/C) is institution and practitioner dependent. A/C ventilation, as in CMV, is a full support mode in that the ventilator performs most, if not all, of the work of breathing. These modes are beneficial for patients who require a high minute ventilation. Full support reduces oxygen consumption and carbon dioxide production of the respiratory muscles. A potential drawback of A/C ventilation in the patient with obstructive airway disease is worsening of air trapping and breath stacking.
When full respiratory support is necessary for the paralyzed patient following neuromuscular blockade, no difference exists in minute ventilation or airway pressures with any of the above modes of ventilation. In the apneic patient, A/C with a respiratory rate (RR) of 10 and a TV of 500 mL delivers the same minute ventilation as SIMV with the same parameters.
Pressure support ventilation
For the spontaneously breathing patient, pressure support ventilation (PSV) has been advocated to limit barotrauma and to decrease the work of breathing. Pressure support differs from A/C and IMV in that a level of support pressure is set to assist every spontaneous effort. Airway pressure support is maintained until the patient's inspiratory flow falls below a certain cutoff (eg, 25% of peak flow). The patient determines the tidal volume, respiratory rate, and flow rate. [3] With some ventilators, there is the ability to set a back-up IMV rate should spontaneous respirations cease.
PSV is frequently the mode of choice in patients whose respiratory failure is not severe and who have an adequate respiratory drive. It can result in improved patient comfort, reduced cardiovascular effects, reduced risk of barotrauma, and improved distribution of gas.
Noninvasive ventilation
The application of mechanical ventilatory support through a mask in place of endotracheal intubation is becoming increasingly accepted and used in the emergency department. Considering this modality for patients with mild-to-moderate respiratory failure is appropriate. The patient must be mentally alert enough to follow commands. Clinical situations in which it has proven useful include acute exacerbation of chronic obstructive pulmonary disease (COPD) or asthma, decompensated congestive heart failure (CHF) with mild-to-moderate pulmonary edema, and pulmonary edema from hypervolemia. It is most commonly applied as continuous positive airway pressure (CPAP) and biphasic positive airway pressure (BiPAP). BiPAP is commonly misunderstood to be a form of pressure support ventilation triggered by patient breaths; in actuality, BiPAP is a form of CPAP that alternates between high and low positive airway pressures, permitting inspiration (and expiration) throughout.
Reviews of the literature have shown noninvasive positive-pressure ventilation (NPPV) to be beneficial for COPD, reducing the rate of tracheal intubations and the length of stay. [2] Clinical guidelines recommend that NPPV be considered as an adjunct to standard medical therapy in patients with severe COPD exacerbations (pH < 7.35 and relative hypercarbia), as well as in patients with cardiogenic pulmonary edema and respiratory failure without shock or acute coronary syndrome requiring urgent percutaneous coronary intervention. [6]
The use of NPPV has been less well studied in asthma, though a recent meta-analysis found that NPPV improved secondary outcomes such as number of hospital admissions, length of ICU stay, and length of hospital stay, as well as had a favorable effects on certain lung function parameters such as peak expiratory flow, forced vital capacity, and FEV1. [7] However, the study did not demonstrate a definite benefit ofNPPV for mortality or intubation rates.
Adverse Consequences of Mechanical Ventilation
The deterioration of intubated patients due to multiorgan failure has been observed for decades. In recent years, however, much progress delineating the adverse effects of positive-pressure ventilation has been made. [8] In 1993, Tremblay et al demonstrated increased cytokine and inflammatory mRNA expression in a high-stress ventilatory model, showing that increasing volumes and reducing PEEP resulted in higher tumor necrosis alpha serum concentrations. Further research over the 1990s demonstrated a cascade of systemic inflammatory effects of biochemical pulmonary injury contributing to distal organ dysfunction. [9]
Pulmonary effects
Barotrauma may result in pulmonary interstitial emphysema, pneumomediastinum, pneumoperitoneum, pneumothorax, and/or tension pneumothorax. High peak inflation pressures (>40 cm water) are associated with an increased incidence of barotrauma. However, note that separating barotrauma from volutrauma is difficult, since increasing barometric pressure is usually accompanied by increasing alveolar volume.
Experimental models of high peak inflation pressures in animals with high extrathoracic pressures have not demonstrated direct alveolar damage from increased pressure without increased volume as well. Thus, the statement that high airway pressures result in alveolar overdistention (volutrauma) and accompanying increased microvascular permeability and parenchymal injury may be more accurate. Alveolar cellular dysfunction occurs with high airway pressures. The resultant surfactant depletion leads to atelectasis, which requires further increases in airway pressure to maintain lung volumes.
High-inspired concentrations of oxygen (fraction of inspired oxygen [FiO2] >0.5) result in free-radical formation and secondary cellular damage. These same high concentrations of oxygen can lead to alveolar nitrogen washout and secondary absorption atelectasis.
It has been theorized that pulmonary biophysical and biomechanical injury in the presence of bacterial lung infections contributes to bacterial translocation and bacteremia.
Cardiovascular effects
The heart, great vessels, and pulmonary vasculature lie within the chest cavity and are subject to the increased intrathoracic pressures associated with mechanical ventilation. The result is a decrease in cardiac output due to decreased venous return to the right heart (dominant), right ventricular dysfunction, and altered left ventricular distensibility.
The decrease in cardiac output from reduction of right ventricular preload is more pronounced in the hypovolemic patient and in those with a low ejection fraction.
Exaggerated respiratory variation on the arterial pressure waveform is a clue that positive-pressure ventilation is significantly affecting venous return and cardiac output. In the absence of an arterial line, a good pulse oximetry waveform can be equally instructive. A reduction in the variation after volume loading confirms this effect. These effects will most frequently be seen in patients with preload-dependent cardiac function (that is, operating on the right side of the Starling curve) and in hypovolemic patients or in those with otherwise compromised venous return.
Increased alveolar-capillary permeability secondary to pulmonary inflammatory changes may, alternatively, contribute to increased cardiac output.
For patients with Swan-Ganz catheterization in place for whom cardiac output may be measured (usually in the ICU setting), PEEP studies may be performed. This is performed by adjusting PEEP, monitoring oxygenation by peripheral oxygen saturation or arterial oxygen measurement via blood gas sampling, and measuring the associated cardiac output. The process is repeated at various PEEP settings, and the results are recorded. The practitioner can then review the results and determine the optimal PEEP for that patient at that time. This procedure is not generally performed in the ED but underlies the association of ventilation strategy and cardiac output.
Renal, hepatic, and gastrointestinal effects
Positive-pressure ventilation is responsible for an overall decline in renal function with decreased urine volume and sodium excretion.
Hepatic function is adversely affected by decreased cardiac output, increased hepatic vascular resistance, and elevated bile duct pressure.
The gastric mucosa does not have autoregulatory capability. Thus, mucosal ischemia and secondary bleeding may result from decreased cardiac output and increased gastric venous pressure.
Indications For Mechanical Ventilation
The principal indications for mechanical ventilation are airway protection and respiratory failure. A compromised airway, or an airway at risk of compromise, may be identified by physical examination and ancillary testing.
Respiratory failure in the ED is almost always—and most appropriately—a clinical diagnosis. The decision to intubate and mechanically ventilate or to institute noninvasive ventilation support is generally made purely on clinical grounds without delay for laboratory evaluation.
Respiratory failure may also be easily identified with laboratory or pulmonary function data. Obtaining a PaCO2 is useful to confirm respiratory failure when a broader differential diagnosis exists—for example, obtunded patients who may be hypercarbic but might have a reversible metabolic or toxicological etiology for their conditions—but adequate stabilization and ventilation of these patients should not be delayed to wait for laboratory results.
Mechanical ventilation is indicated for both hypercapnic respiratory failure and hypoxemic respiratory failure. It is also indicated for treatment of certain critical conditions such as correction of life-threatening acidemia in the setting of salicylate intoxication, for intentional hyperventilation in the setting of major head injury with elevated intracranial pressure, for suspicion of clinical brain herniation from any cause, or for a patient in critical condition with cyclic antidepressant toxicity.
Laboratory criteria
Table. Laboratory Criteria for Mechanical Ventilation (Open Table in a new window)
Laboratory Criteria for Mechanical Ventilation |
|
Blood gases |
PaO2< 55 mm Hg |
|
PaCO2 >50 mm Hg and pH < 7.32 |
Pulmonary function tests |
Vital capacity < 10 mL/kg |
|
Negative inspiratory force < 25 cm water |
|
FEV1< 10 mL/kg |
Clinical criteria
See the list below:
-
Apnea or hypopnea
-
Respiratory distress with altered mentation
-
Clinically apparent increasing work of breathing unrelieved by other interventions
-
Obtundation and need for airway protection
Other criteria
See the list below:
-
Controlled hyperventilation (eg, in head injury).
-
Severe circulatory shock
No absolute contraindications exist to mechanical ventilation. The need for mechanical ventilation is best made early on clinical grounds. A good rule of thumb is if the practitioner is thinking that mechanical ventilation is needed, then it probably is. Waiting for return of laboratory values can result in unnecessary morbidity or mortality.
Guidelines for Ventilator Settings
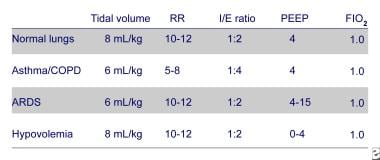
See the image below for suggested initial settings.
Mode of ventilation
The mode of ventilation should be tailored to the needs of the patient. In the emergent situation, the practitioner may need to order initial settings quickly. SIMV and A/C are versatile modes that can be used for initial settings. In patients with a good respiratory drive and mild-to-moderate respiratory failure, PSV is a good initial choice.
Tidal volume
Observations of the adverse effects of barotrauma and volutrauma have led to recommendations of lower tidal volumes than in years past, when tidal volumes of 10-15 mL/kg were routinely used.
An initial TV of 5-8 mL/kg of ideal body weight is generally indicated, with the lowest values recommended in the presence of obstructive airway disease and ARDS. The goal is to adjust the TV so that plateau pressures are less than 35 cm water.
Respiratory rate
A respiratory rate (RR) of 8-12 breaths per minute is recommended for patients not requiring hyperventilation for the treatment of toxic or metabolic acidosis, or intracranial injury. High rates allow less time for exhalation, increase mean airway pressure, and cause air trapping in patients with obstructive airway disease. The initial rate may be as low as 5-6 breaths per minute in asthmatic patients when using a permissive hypercapnic technique.
Supplemental oxygen therapy
The lowest FiO2 that produces an arterial oxygen saturation (SaO2) greater than 90% and a PaO2 greater than 60 mm Hg is recommended. No data indicate that prolonged use of an FiO2 less than 0.4 damages parenchymal cells.
Inspiration/expiration ratio
The normal inspiration/expiration (I/E) ratio to start is 1:2. This is reduced to 1:4 or 1:5 in the presence of obstructive airway disease in order to avoid air-trapping (breath stacking) and auto-PEEP or intrinsic PEEP (iPEEP). Use of inverse I/E may be appropriate in certain patients with complex compliance problems in the setting of ARDS.
Inspiratory flow rates
Inspiratory flow rates are a function of the TV, I/E ratio, and RR and may be controlled internally by the ventilator via these other settings. If flow rates are set explicitly, 60 L/min is typically used. This may be increased to 100 L/min to deliver TVs quickly and allow for prolonged expiration in the presence of obstructive airway disease.
Positive end-expiratory pressure
Positive end-expiratory pressure (PEEP) has several beneficial effects and, when used at optimal levels in combination with low tidal volumes, may reduce the incidence of ventilator-induced lung injury. In particular, there is a significant amount of ongoing research evaluating the use of high levels of PEEP in acute lung injury (ALI) and ARDS. PEEP has been found to reduce the risk of atelectasis trauma by increasing the number of "open" alveoli participating in ventilation, thereby minimizing trauma due to the cyclical collapse and reopening of alveoli. However, note that in disease states such as ARDS, the degree to which alveoli function has been compromised varies tremendously within the lungs and there is no single ideal PEEP appropriate for all alveoli; rather, a compromise PEEP must be selected.
In addition to alveolar recruitment, an additional beneficial effect of PEEP is to shift lung water from the alveoli to the perivascular interstitial space. It does not decrease the total amount of extravascular lung water. This is of clear benefit in cases of cardiogenic as well as noncardiogenic pulmonary edema. An additional benefit of PEEP in cases of CHF is to decrease venous return to the right side of the heart by increasing intrathoracic pressure.
Applying physiologic PEEP of 3-5 cm water is common to prevent decreases in functional residual capacity in those with normal lungs. The reasoning for increasing levels of PEEP in critically ill patients is to provide acceptable oxygenation and to reduce the FiO2 to nontoxic levels (FiO2< 0.5). The level of PEEP must be balanced such that excessive intrathoracic pressure (with a resultant decrease in venous return and risk of barotrauma) does not occur.
Sensitivity
With assisted ventilation, the sensitivity typically is set at -1 to -2 cm water. The development of iPEEP increases the difficulty in generating a negative inspiratory force sufficient to overcome iPEEP and the set sensitivity. Newer ventilators offer the ability to sense by inspiratory flow instead of negative force. Flow sensing, if available, may lower the work of breathing associated with ventilator triggering.
Monitoring During Ventilatory Support
Cardiac monitor, blood pressure, and pulse oximetry (SaO2) are recommended. The authors’ practice with stable patients is to titrate down FiO2 to the minimum value necessary to maintain maximal SaO2. An arterial blood gas (ABG) measurement is frequently obtained 10-15 minutes after the institution of mechanical ventilation. The measured arterial PaO2 should verify the transcutaneous pulse oximetry readings and direct the reduction of FiO2 to a value less than 0.5. The measured PaCO2 can suggest adjustments of minute ventilation but should be interpreted in light of the patient's overall acid-base status. For example, full correction of PaCO2 in a chronically hypercarbic COPD patient will lead to unopposed metabolic alkalosis.
Reasonable alternatives to arterial blood gas measurement in more stable patients include measuring the venous blood gas, which will give values close to arterial pH and PaCO2 or monitoring an end-tidal carbon dioxide. An additional advantage of end-tidal carbon dioxide monitoring is that it can detect acute ventilator dysfunction such as endotracheal tube obstruction or dislodgement. [10]
Peak inspiratory and plateau pressures should be assessed frequently, although it should be recognized that both pressures will be increased by extrapulmonary pressure, for example from stiff chest walls or a distended abdomen, and do not reflect the true risk of barotrauma. In general, however, parameters may be altered to limit pressures to less than 35 cm water. Expiratory volume is checked initially and periodically (continuously if ventilator is capable) to ensure that the set tidal volume is delivered. Any indication of an air leak must prompt a search for underinflated tube cuffs, open tubing ports, or worsening pneumothorax. In patients with airway obstruction, monitor auto-PEEP.
Initial Ventilator Settings in Various Disease States
In the ED setting, patients frequently require full respiratory support. For most ED patients who are paralyzed as a component of rapid-sequence induction, CMV and A/C are good choices as an initial ventilatory mode. SIMV may be better tolerated in nonparalyzed patients with obstructive airway disease and an intact respiratory effort. PSV can be used when respiratory effort is intact and respiratory failure is not severe. [11]
Noninvasive ventilation (CPAP, BiPAP) can be used effectively in many cases of severe COPD and CHF to avoid tracheal intubation. Initial ventilator settings are guided by the patient's pulmonary pathophysiology and clinical status. Adjustments can then be made to limit barotrauma, volutrauma, and oxygen toxicity. CPAP and BiPAP require alert, cooperative patients capable of independently maintaining their airways and are contraindicated in the presence of facial trauma.
Asthma and COPD
Hypoxia can generally be corrected through a high FiO2, but patients with airway obstruction are at risk of high airway pressures, breath stacking leading to intrinsic PEEP, barotrauma, and volutrauma. To minimize intrinsic PEEP, it is recommended that expiratory flow time be increased as much as possible and that tidal volumes and respiratory rates are set at low values. [12] Permissive hypercapnia enables a low respiratory rate of 6-8 breaths per minute to be used, as well as an increased I:E ratio of 1:1.5 or 1:2.
PEEP may benefit some asthmatic patients by reducing the work of breathing and maintaining open airways during expiration, but its effects are difficult to predict and must be carefully monitored. Patients with asthma and COPD are at particular risk of barotraumatic progression to tension pneumothorax, a complication that can initially appear similar to runaway intrinsic PEEP. These conditions may be distinguished by temporary detachment of the patient from positive-pressure ventilation; if exhalation results in a recovery of pulse or normal blood pressure, the diagnosis is intrinsic PEEP.
CPAP and BiPAP will benefit some asthmatics and many patients with COPD. These patients will require careful monitoring as they can easily deteriorate from hypercarbia, intrinsic PEEP, or respiratory exhaustion. Nevertheless, a CochraneDatabase Systematic Review analysis of trials including patients with severe COPD exacerbations demonstrated that the use of noninvasive positive-pressure ventilation absolutely reduced the rate of endotracheal intubation by 59% (95% confidence interval [CI] of relative risk [RR]: 0.33-0.53), the length of hospital stay by 3.24 days (95% CI: 2.06-4.44 days), and the risk of mortality by 48% (95% CI of RR: 0.35-0.76). [2]
Acute respiratory distress syndrome
ARDS lungs are typically irregularly inflamed and highly vulnerable to atelectasis as well as barotrauma and volutrauma. Their compliance is typically reduced, and their dead space increased. The standard of care for the ventilatory management of patients with ARDS changed dramatically in 2000 with the publication of a large multicenter, randomized trial comparing patients with ARDS initially ventilated with either the traditional tidal volume of 12 mL/kg or a lower TV of 6 mL/kg. This trial was stopped early because the lower tidal volume was found to reduce mortality by an absolute 8.8% (P=.007). Intriguingly, plasma interleukin 6 concentrations decreased in the low TV group relative to the high TV group (P< .001), suggesting a decrease in lung inflammation. [13, 14, 15, 16]
The authors recommend initiating ventilation of patients with ARDS with A/C ventilation at a tidal volume of 6 mL/kg, with a PEEP of 5 and initial ventilatory rate of 12, titrated up to maintain a pH greater than 7.25. There is not yet adequate evidence to routinely recommend PEEP greater than 5 cm water, but, in appropriately monitored circumstances, it may be attempted. [17] Intrinsic PEEP may occur in patients with ARDS at high ventilatory rates and should be watched for and treated by reducing the rate of ventilation under direct observation until plateau pressures decrease. The authors recommend a target plateau pressure of less than 30 cm water. Once a patient has been stabilized with adequate tidal volumes at a plateau pressure of less than 30 cm water, considering a trial of pressure-cycled ventilation is reasonable.
Several recruitment maneuvers have been devised to increase the proportion of alveoli ventilated in ARDS. These techniques typically attempt short-term increased PEEP or volume to open occluded or collapsed alveoli. Gattinoni et al, for example, found that among ARDS patients undergoing whole-lung CT, applying 45 cm water PEEP recruited a mean of 13% new lung tissue. [18]
A recent meta-analysis that compared high versus low levels of PEEP in patients with ALI and ARDS found no difference in mortality before hospital discharge amongst studies that used the same tidal volume in both control and intervention arms. [17] In a subsequent subgroup analysis that assessed lung-protective ventilation (low tidal volume, high PEEP) versus conventional mechanical ventilation, the authors found a decrease in mortality with the use of a lung-protective ventilation strategy. The same review also found that high levels of PEEP do improve oxygenation in patients with ALI and ARDS.
In a recent prospective, randomized, controlled trial, Guerin et al examined whether early prone positioning during mechanical ventilation can improve outcomes in patients with severe ARDS. The authors found that both the 28-day and unadjusted 90-day mortalities in the prone group were significantly lower (16% and 23.6%, respectively) than in the supine group (32.8% and 41%, respectively). [19] Although they found no difference between the groups with regard to duration of invasive mechanical ventilation or length of stay in the ICU, they found a higher incidence of cardiac arrest in the supine group (31% vs 16% in the prone group).
Permissive hypercapnia is a ventilatory strategy that has won particular favor in the management of patients with ARDS and COPD/asthma who would otherwise require dangerously high tidal volumes and airway pressures. In patients without contraindications such as head injury, cerebrovascular accident (CVA), elevated intracranial pressure, or cardiovascular instability, permissive hypercapnia has permitted much decreased tidal volumes, airway pressures, and respiratory rates, though evidence for a decrease in mortality rates is incomplete. [20] The typically recommended target pH is 7.25.
Noninvasive ventilatory strategies have met with little success in the treatment of patients with ARDS. The authors recommend great caution and close monitoring if noninvasive positive pressure ventilation (NIPPV) is attempted among patients with ARDS.
In trials of NIPPV among patients with undifferentiated hypoxemia, the presence of pneumonia or ARDS was associated with significantly increased risk of failure. Some subgroups of patients with ARDS may benefit from NIPPV; however, Antonelli et al demonstrated greater success in applying noninvasive positive pressure ventilation to patients with lower simplified acute physiology scores and higher PaO2/FiO2 ratios. [21]
Congestive heart failure
CHF responds very well to positive-pressure ventilation, which serves the dual role of opening alveoli and reducing preload. Many patients with CHF benefit from a trial of noninvasive CPAP or BiPAP. Some of these patients will clinically improve so rapidly that admitting services may request discontinuation of noninvasive ventilatory support, but great caution must be maintained if this is attempted, as fluid may unpredictably reaccumulate, resulting in hypoxia and respiratory failure.
Intubated patients usually manage to adequately oxygenate. PEEP can be increased as tolerated to improve oxygenation and reduce preload. However, in some patients, cardiac output can be particularly dependent on preload and such patients may easily develop postintubation hypotension. Management of this common complication includes a combination of fluid therapy, discontinuation of nitroglycerin or other medical therapies, and, if necessary, medical or mechanical hemodynamic support interventions. [22]
Traumatic brain injury
Hyperventilation was traditionally recommended in the management of severe traumatic brain injury, but recent studies have demonstrated poor outcomes thought to be secondary to excessive cerebral vasoconstriction and reduced cerebral perfusion. However, retrospective data have demonstrated decreased mortality among traumatic brain injury ventilated to PCO2 between 30 and 39 mm Hg, though this has not been prospectively validated. [23, 24]
Ventilation-related recommendations and suggestions for adults with COVID-19
Ventilation clinical practice guidelines in adults with COVID-19 were released by the European Society of Intensive Care Medicine and the Society of Critical Care Medicine. [25]
It is suggested to start supplemental oxygen if the peripheral oxygen saturation (SPO2) is less than 92%. It is recommended to start supplemental oxygen if the SPO2 is less than 90%.
In the event of acute hypoxemic respiratory failure on oxygen, it is recommended that the SPO2 be maintained at no higher than 96%.
In patients with acute hypoxemic respiratory failure despite conventional oxygen therapy, it is suggested that a high-flow nasal cannula be used rather than conventional oxygen therapy.
In patients with acute hypoxemic respiratory failure, it is also suggested that a high-flow nasal cannula be used over noninvasive positive-pressure ventilation.
In these patients with acute hypoxemic respiratory failure, in the event a high-flow nasal cannula is not available and the patient has no urgent indication for endotracheal intubation, it is suggested that a trial of noninvasive positive-pressure ventilation be conducted, with close monitoring and short-interval assessment for worsening of respiratory failure.
While considered an option, no recommendation was made regarding helmet noninvasive positive-pressure ventilation versus mask noninvasive positive-pressure ventilation.
In patients receiving either noninvasive positive-pressure ventilation or high-flow nasal cannula, it is recommended they be closely monitored for worsening respiratory status; early intubation in a controlled setting is recommended if worsening occurs.
In patients with acute respiratory distress syndrome (ARDS) who are on mechanical ventilation, it is recommended to use low-tidal-volume ventilation (4-8 mL/kg of predicted body weight) versus higher tidal volumes (>8 mL/kg).
In patients with ARDS who are on mechanical ventilation, it is recommended to target plateau pressures at less than 30 cm water.
In patients with moderate-to-severe ARDS who are on mechanical ventilation, it is suggested to use a higher positive end-expiratory pressure (PEEP) strategy versus a lower PEEP strategy. When using a higher PEEP strategy (ie, PEEP >10 cm water), monitor patients for barotrauma.
In patients with ARDS who are on mechanical ventilation, it is suggested to use a conservative fluid strategy versus a liberal fluid strategy.
In patients with moderate-to-severe ARDS who are on mechanical ventilation, it is suggested to use prone ventilation for 12-16 hours versus no prone ventilation.
In patients with moderate-to-severe ARDS who are on mechanical ventilation, it is suggested to use, as needed, intermittent boluses of neuromuscular blocking agents versus a continuous infusion, to facilitate protective lung ventilation.
Use of a continuous infusion of neuromuscular blocking agents is suggested in the event of persistent ventilator dyssynchrony, a need for ongoing deep sedation, prone ventilation, or persistently high plateau pressures.
In patients with ARDS who are on mechanical ventilation, routine use of inhaled nitric oxide is not recommended.
In mechanically ventilated patients with severe ARDS and hypoxemia despite optimization of ventilation and other rescue strategies, a trial of inhaled pulmonary vasodilator is suggested as rescue therapy; if rapid improvement in oxygenation is not observed, taper off treatment.
In mechanically ventilated patients with severe ARDS and hypoxemia despite optimization of ventilation, use of recruitment maneuvers is suggested over not using recruitment maneuvers. If recruitment maneuvers are used, staircase (incremental PEEP) recruitment maneuvers are not recommended.
In those patients on mechanical ventilation who have refractory hypoxemia despite optimization of ventilation and who have undergone rescue therapies and proning, it is suggested to use venovenous extracorporeal membrane oxygenation (EMCO) if available; alternatively, refer the patient to center that has ECMO. However, because EMCO is resource-intensive and it requires experienced centers/healthcare workers and infrastructure, it should only be considered in carefully selected patients with severe ARDS.
For more information go to Coronavirus Disease 2019 (COVID-19) and Treatment of Coronavirus Disease 2019 (COVID-19) Investigational Drugs and Other Therapies.
Ventilator Troubleshooting - Managing Complications in the ED
The differential diagnosis of the clinically deteriorating, mechanically ventilated patient is wide and includes endotracheal tube or ventilator dysfunction, improper ventilator settings, pain, anxiety, and pulmonary or extrapulmonary disease processes. [10] The complications most commonly encountered in the ED include hypoxia, hypotension, high-pressure alarms, and low exhaled–volume alarms.
Intubated patients who develop hemodynamic instability with respiratory compromise should immediately be disconnected from the ventilator and manually ventilated with 100% FiO2.
One of the first diagnoses that should be considered in any hemodynamically unstable patient undergoing positive-pressure ventilation is tension pneumothorax. This is a clinical diagnosis and should be detected and treated with needle decompression prior to obtaining a chest radiograph.
A second diagnosis to exclude, particularly in patients with asthma or COPD, is intrinsic PEEP. As discussed, intrinsic PEEP occurs as a result of incomplete exhalation, which subsequently leads to hyperinflation, increased intrathoracic pressure, decreased venous return, and decreased preload. The diagnosis of intrinsic PEEP may be made by performing an end-expiratory hold or by detecting a non-zero end-expiratory flow on the ventilator. The treatment for intrinsic PEEP is to allow for lung deflation, then to alter mechanical ventilation settings to allow for longer expiratory times by decreasing the respiratory rate, decreasing the tidal volume, or changing the inspiratory-to-expiratory ratio.
Other diagnoses to consider are an obstructed endotracheal tube and an endotracheal tube cuff leak. In the case of endotracheal tube obstruction, attempts to manually ventilate the patient are met with a significant amount of resistance and high-pressure alarms may sound. Endotracheal tube obstruction may be caused by extrinsic compression; tube plugs with mucus, blood, or foreign bodies; tube kinks; or tube biting. Tube suctioning and adequate patient sedation are recommended after other causes of obstruction are ruled out.
Measurement of peak pressures and plateau pressures may be helpful in identifying the location of resistance, especially if graphical representation of airway pressures is available. Peak pressure, which reflects resistance to airflow, is measured by the ventilator during inspiration. Plateau pressure is thought to reflect pulmonary compliance and can be measured by applying a brief inspiratory pause after ventilation. High peak pressure with normal plateau pressures indicates increased resistance to flow, such as endotracheal tube obstruction or bronchospasm. An increase in both peak and plateau pressures suggest decreased lung compliance, which may be seen in disease states such as pneumonia, ARDS, pulmonary edema, and abdominal distention.
Low exhaled volume alarms are triggered by air leaks. These are most frequently secondary to ventilatory tubing disconnect from the patient's tracheal tube but will also occur in the event of balloon deflation or tracheal tube dislodgement. Tube placement, balloon inflation, and connection to the ventilator should be carefully verified.
Hypoxia after intubation may occur secondary to hypoventilation, worsening cardiac shunting, inadequate FiO2, mainstem intubation, aspiration, tube dislodgement, or pulmonary edema. The causes of high airway pressures and low exhaled volumes described above can result in hypoxia if they cause hypoventilation. Despite the use of numerous safety precautions, cases are occasionally documented of ventilators being connected to compressed air or nitrous oxide rather than oxygen. Increasing FiO2 and adjusting ventilatory settings to increase PEEP or respiratory rate are useful first steps after excluding equipment failure and mechanical causes of hypoxia.
Hypotension after intubation is usually attributable to diminished central venous blood return to the heart secondary to elevated intrathoracic pressures. This can be treated with fluid infusions and/or adjustment of ventilatory settings to lower intrathoracic pressure (reducing PEEP, tidal volume, and, if air trapping is suspected, respiratory rate). Hypotension may also be secondary to vasovagal reaction to intubation, rapid sequence induction, sedation, and tension pneumothorax.
Supportive Care
While the role of the emergency physician has traditionally been limited to intubation and initiation of mechanical ventilation, intubated patients are spending a greater portion of their hospital stay in the ED secondary to decreased availability of ICU beds. In this setting, it becomes important to initiate preventative measures to decrease the incidence of the secondary complications of mechanical ventilation, such as ventilator-associated pneumonia (VAP), venous thromboembolism (VTE), and stress-related mucosal injury.
VAP is defined as pneumonia in a mechanically ventilated patient that is not clinically present at the time of intubation. [26] The time frame for development of VAP is typically 48 hours or more after intubation, as this is when the disease typically manifests itself clinically. VAP has been implicated as the most common infectious complication occurring in ICU patients and results in prolonged ICU and hospital lengths of stay, prolonged duration of mechanical ventilation, and overall increased cost of care. [10]
Evidence suggests that prehospital and ED intubation, in addition to ED length of stay, are independent risk factors for the development of VAP. [10, 27] These findings, when combined with the significant morbidity and mortality associated with VAP, confer upon the ED physician a responsibility to implement measures to reduce the risk of VAP in the ED. These interventions are aimed at reducing the risk of aspiration and decreasing bacterial colonization.
The Centers for Disease Control and Prevention published Guidelines for Preventing Health-Care Associated Pneumonia in 2003, in which they recommend placing the patient in a semiupright position, with the head of the bed elevated 30-45o, in order to reduce the risk of aspiration. [28] Other measures such as early placement of a nasogastric tube and oral care with a soft toothbrush and chlorhexidine rinses may also be considered. [26] Lastly, endotracheal cuff pressures should be monitored initially after intubation and every 4 hours thereafter, with goal pressures of 20-30 cm water, as increased risk of pneumonia has been associated with cuff pressures less than 20 cm water.
In addition to VAP, mechanically ventilated ICU patients are also at high risk for development of VTE and stress-related injury of the gastrointestinal mucosa. In patients without contraindications, unfractionated or low-molecular-weight heparin should be considered in these patients for VTE prophylaxis. As the incidence of gastric mucosal erosions has been found to be greater than 75% in ICU patients within 24 hours of admission, gastrointestinal prophylaxis with a proton pump inhibitor, sucralfate, or histamine receptor antagonist should be considered in patients who are at high risk of gastrointestinal hemorrhage. [10] These high-risk patients have been identified as those with coagulopathy, history of gastrointestinal bleeding, history of gastritis or peptic ulcer, or mechanical ventilation for more than 48 hours.
Questions & Answers
Overview
What is the importance of ventilator management in the emergency department (ED)?
What are the different strategies of ventilator management based on?
What are the effects of ventilator-induced lung injury?
How does effective ventilator management minimize iatrogenic conditions and improve survival rates?
What is the volume-cycled mode of mechanical ventilation?
What is the pressure-cycled mode of mechanical ventilation?
What is high-frequency oscillatory support in mechanical ventilation?
How is continuous mandatory ventilation delivered?
How is assist-control ventilation delivered?
How is intermittent mandatory ventilation delivered?
How is synchronous intermittent mandatory ventilation delivered?
How is a ventilation mode selected?
What is pressure support ventilation (PSV)?
What are the indications and advantages of noninvasive ventilation?
How effective is noninvasive positive-pressure ventilation (NPPV) in COPD and asthma?
What are the adverse effects of mechanical ventilation?
What are the pulmonary adverse effects of mechanical ventilation?
What are the cardiovascular adverse effects of mechanical ventilation?
What are the renal adverse effects of mechanical ventilation?
What are the hepatic adverse effects of mechanical ventilation?
What are the GI adverse effects of mechanical ventilation?
What are the principal indications for mechanical ventilation?
What are the lab criteria for mechanical ventilation?
What are the clinical criteria for mechanical ventilation?
What are other criteria for mechanical ventilation?
What are the contraindications to mechanical ventilation?
What are the guidelines for ventilator settings?
How is the mode of ventilation determined?
What is the ventilator setting for tidal volume?
What respiratory rate (RR) is recommended in mechanical ventilation?
What is the recommended supplemental oxygen therapy in mechanical ventilation?
What is the normal inspiration and expiration ratio in mechanical ventilation?
What is the setting for inspiratory flow rates in mechanical ventilation?
What is the sensitivity setting in mechanical ventilation?
What monitoring is recommended during ventilatory support?
How do initial ventilator settings vary according to patient condition?
What are the initial ventilator settings in asthma and COPD?
What are the initial ventilation strategies in congestive heart failure?
What are the initial ventilator settings in traumatic brain injury?
What are ventilation-related recommendations and suggestions for adults with COVID-19?
What are the potential complications in mechanically ventilated patient and which are common?
Which diagnoses should be considered and excluded in patients undergoing mechanical ventilation?
What triggers a low exhaled volume alarm in mechanical ventilation?
What causes hypoxia after intubation in mechanical ventilation?
What causes hypotension after intubation in mechanical ventilation?
What is ventilator-associated pneumonia (VAP) and what are the risk factors for its development?
-
Initial ventilator settings in various disease states.
Tables
What would you like to print?
- Introduction to Ventilator Management
- Modes of Mechanical Ventilation
- Methods of Ventilatory Support
- Adverse Consequences of Mechanical Ventilation
- Indications For Mechanical Ventilation
- Guidelines for Ventilator Settings
- Monitoring During Ventilatory Support
- Initial Ventilator Settings in Various Disease States
- Ventilator Troubleshooting - Managing Complications in the ED
- Supportive Care
- Questions & Answers
- Show All
- Tables
- References