Practice Essentials
Blast injuries result from explosions that have the capability to cause multisystem, life-threatening injuries in single or multiple victims simultaneously. These types of events present complex triage, diagnostic, and management challenges for the health care provider. Explosions have the capability to cause multisystem, life-threatening injuries in single or multiple victims simultaneously. These types of events present complex triage, diagnostic, and management challenges for the health care provider. Explosions can produce classic injury patterns from blunt and penetrating mechanisms to several organ systems, but they can also result in unique injury patterns to specific organs, including the lungs and the central nervous system. Understanding these crucial differences is critical to managing these situations. [1, 2, 3, 4, 5, 6]
The extent and pattern of injuries produced by an explosion are a direct result of several factors, including the amount and composition of the explosive material (eg, the presence of shrapnel or loose material that can be propelled; radiologic or biological contamination), the surrounding environment (eg, the presence of intervening protective barriers), the distance between the victim and the blast, the delivery method if a bomb is involved, and any other environmental hazards. No 2 events are identical, and the spectrum and extent of injuries produced vary widely. [1]
Blast injuries are generally categorized as primary to quinary. Primary injuries (PBIs) are caused by the effect of transmitted blast waves on gas-containing structures; secondary injuries, by the impact of airborne debris; tertiary injury, by the transposition of the entire body because of blast wind or structural collapse; quaternary injuries, by exposure to explosive products (heat and light) or toxic substances; and quinary injury, by exposure to environmental contaminants, including chemicals, radiation, viruses, and bacteria. [7] An analysis of data from the American College of Surgeons National Trauma Databank (NTDB) found that the majority of blast injuries (56%) resulted from fireworks, gas, or pressurized container explosions. [8]
Primary blast injury is organ and tissue damage caused solely by the blast wave associated with high-order explosives. (See the image below.)
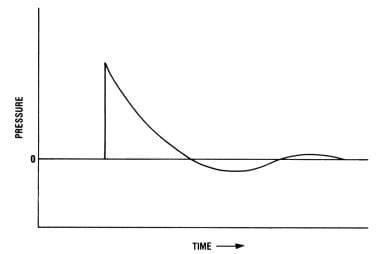 Blast injuries. Idealized graph of a blast pressure wave over time. Courtesy of Bowen TE and Bellamy RF, eds, Emergency War Surgery. Washington, DC: United States Government Printing Office, 1988.
Blast injuries. Idealized graph of a blast pressure wave over time. Courtesy of Bowen TE and Bellamy RF, eds, Emergency War Surgery. Washington, DC: United States Government Printing Office, 1988.
Signs and symptoms
Unique patterns of injury are found in all blast types. The lungs, bowel, and middle ear are most susceptible to primary blast injuries (PBIs).
Pulmonary barotrauma, the most common fatal PBI, may include the following:
-
Pulmonary contusion
-
Systemic air embolism, which most commonly occludes blood vessels in the brain or spinal cord
-
Free radical–associated injuries such as thrombosis, lipoxygenation, and disseminated intravascular coagulation (DIC)
-
Impaired pulmonary performance lasting hours to days
-
Acute respiratory distress syndrome (ARDS) may be a result of direct lung injury or of shock from other body injuries
Acoustic barotrauma consists of the following:
-
Tympanic membrane rupture (most common)
-
Hemotympanum without perforation
-
Ossicle fracture or dislocation may occur with very high energy explosions
Thoracic PBI produces the following unique cardiovascular response:
-
A decrease in heart rate, stroke volume, and cardiac index
-
The normal reflex increase in systemic vascular resistance does not occur, so blood pressure falls
-
If this response is not fatal, recovery usually occurs within 15 minutes to 3 hours
Crush syndrome and acute renal failure may occur in patients rescued from collapsed structures. Increasing extremity pain after an explosion should raise the suspicion of compartment syndrome.
Diagnosis
Lab tests
Lab tests are essential for accurate diagnosis in the mass-casualty situation. Considerations include the following:
-
Do not overwhelm the laboratory with screening or protocol laboratory tests of little clinical benefit
-
Most patients injured by significant explosions should have a screening urinalysis
-
If the explosion occurred in an enclosed space or was accompanied by fire, test carboxyhemoglobin (HbCO) and electrolytes to assess acid/base status
-
Pulse oximetry readings may be misleading in cases of CO poisoning
-
Victims of major trauma should have baseline hemoglobin determinations, crossmatching for potential blood transfusion, and screening for DIC
Imaging studies
Indications for chest radiography are as follows:
-
History of exposure to high overpressure
-
Tympanic membrane rupture
-
Respiratory symptoms
-
Abnormal findings on chest auscultation
-
Visible external signs of thoracic trauma
If significant abdominal pain is present, consider an immediate abdominal radiographic series (flat and upright films) or abdominal CT to detect pneumoperitoneum from enteric rupture. Intestinal barotrauma is more common with underwater injuries than air blast injuries.
Focused abdominal sonography for trauma (FAST) is a potentially useful tool for rapidly screening patients, especially in the setting of multiple seriously injured victims. A positive FAST examination in an unstable patient is an indication for surgical exploration of the abdomen in the operating room. A negative FAST examination is unreliable in the setting of penetrating trauma to the abdomen, flank, buttocks, or back, and it should be followed up with CT examination of the abdomen and pelvis.
Management
Prehospital care includes the following:
-
Screen for radioactive contamination with a hand-held Geiger counter for any explosion that may involve radioactive material, including any explosion that may have been deliberately set; if radioactive material is detected, decontamination of personnel and equipment, as well as notification of the receiving hospital, is required
-
Rapidly identify patients with life-threatening external hemorrhage and control bleeding; early use of tourniquets may be life-saving, especially in the setting of multiple seriously injured casualties
-
High-flow oxygen should be administered to all patients with respiratory distress, abnormal findings on auscultation, and evidence of significant thoracic trauma
-
Avoid administration of large quantities of IV fluid in patients with a high suspicion of ongoing internal hemorrhage; judicious fluid boluses may be required if patients exhibit signs and symptoms of inadequate perfusion, such as deteriorating mental status
-
Initiate measures to reduce heat loss and prevent hypothermia
Emergency department care includes the following:
-
Penetrating wounds (secondary blast injury), blunt trauma (tertiary/secondary blast injury), and burns receive standard treatment
-
Shrapnel wounds (secondary blast injury) are treated as low-velocity gunshot wounds
-
Hemodynamically unstable patients with significant trauma may benefit from early use of packed red blood cells (PRBC) and fresh frozen plasma (FFP) in a 1:1 ratio, as well as platelets
-
Consider early use of fresh whole blood if available
-
In patients with severe trauma, also consider cryoprecipitate and recombinant factor VIIa
-
In patients with traumatic brain injury, prevention of hypoxia and hypotension is critical
-
Because pulmonary contusion tends to evolve over several hours, a period of observation and repeat radiography may be necessary if indicated; definitive airway management and ventilatory support may be required
-
If abdominal pain persists or vomiting develops, consider admitting the patient for observation, as intestinal hematoma may be difficult to detect in the ED
-
In patients with open wounds from blasts, consider broad-spectrum prophylactic antibiotics and provide tetanus toxoid if immunization is not up to date
Patients with significant burns should be transferred to a burn center if the initial receiving hospital does not have adequate facilities. Consider transfer to a level I trauma center for severely injured patients. Consider transfer to a facility with hyperbaric chamber for patients who develop suspected acute gas embolism (AGE) secondary to PBI of the lung.
Consult a trauma surgeon, otolaryngologist, pulmonary medicine specialist, critical care specialist, orthopedic surgeon, plastic surgeon, urologist, and toxicologist, as required.
Prevention
Garments designed to protect against both primary blast injuries (PBIs) and secondary blast injuries (SBIs) have proven to be very effective in the military setting. However, except for use by bomb squad technicians and tactical law enforcement personnel, these garments have little applicability in the civilian setting.
Prehospital personnel should be cognizant of the possibility of a secondary device designed to target rescuers when responding to the scene of a suspected intentional bombing. Hospitals similarly may be attractive targets to terrorists and should ensure heightened security for the facility in the event of a bombing.
Background
The US Department of Defense characterizes blast injuries into 5 categories based on the mechanism of injury. [7] A patient may be injured by more than one of these mechanisms. [9, 10] A primary blast injury is caused solely by the direct effect of blast overpressure on tissue. Air is easily compressible, unlike water. As a result, a primary blast injury almost always affects air-filled structures, such as the lung, ear, and gastrointestinal (GI) tract. A secondary blast injury is caused by flying objects that strike people. A tertiary blast injury is a feature of high-energy explosions. This type of injury occurs when people fly through the air and strike other objects. A quaternary blast injury results from other explosive products (such as heat and light) and from exposure to toxic substances from fuels, metals, and gases that can cause burns and toxic inhalations. A quinary blast injury is caused by environmental contaiminants released in the explosion, including chemicals (eg, sarin or chlorine), radiation (eg, dirty bombs) or viruses and bacteria.
The crash of 2 jets into the World Trade Center twin towers only created a relatively low-order pressure wave, but the resulting fire (quaternary injuries) and building collapse (tertiary injuries) killed thousands. Secondary blast injuries to pedestrians on the street surrounding the towers resulted from falling glass and other debris.
Between 1991 and 2000, 93 terrorist attacks worldwide produced more than 30 casualties, with 885 of these incidents involving explosions. The 2005 London subway bombings, the 1995 bombing of the Murrah Federal Building in Oklahoma City, and the catastrophic explosions of aircraft into buildings on September 11, 2001, in New York City and Washington, DC, reminded health care workers of the magnitude of injuries and death that can result from a blast mechanism. Internationally, explosive devices directed against both civilian and military targets are frequently used in war or acts of terrorism. [9]
As the risk of terrorist bombings in the United States increases, emergency physicians and Emergency Medical Services (EMS) personnel should be especially concerned about radiation exposure and/or chemical contamination of explosion victims. Careful observation for signs and symptoms of exposure to poisonous chemicals, screening for radiation contamination, and decontamination of patients as needed are important steps in the management of victims of nonaccidental explosions. In addition to deliberately set explosions, incidents occur as a result of industrial accidents (eg, factory and mining operations, fuel transportation and storage, grain elevator explosions).
In many parts of the world, undetonated military incendiary devices such as land mines and hand grenades contaminate the sites of abandoned battlefields. Such devices cause a significant number of civilian casualties years and even decades after local hostilities cease. During wartime, injuries arising from explosions frequently outnumber those from gunshots, with many innocent civilians becoming victims.
Much of the challenge facing care providers is the potential for the sudden creation of large numbers of patients who require extensive medical resources. This scenario can overwhelm local EMS and hospital resources. Emergency physicians must remain attentive to the possibility and consequences of blast injuries.
Once notified of a possible bombing or explosion, hospital-based physicians should consider immediately activating hospital disaster and contingency plans, including preparations to care for anywhere from a handful to hundreds of victims.
Frequency
Mortality/Morbidity
Mortality rates vary widely between incidents. An analysis of 29 large terrorist bombing events showed 8,364 casualties, including 903 immediate deaths and 7,461 immediately surviving injured. [11] Immediate death/injury rates were higher for bombings involving structural collapse (25%) than for confined space (8%) and open air detonations (4%).
Unique patterns of injury are found in all bombing types. Injury is caused both by direct blast overpressure (primary blast injury) and by a variety of associated factors. Enclosed-space explosions, including those occurring in buses, and in-water explosions produce more primary blast injury. Blasts in ultra-confined spaces such as buses have the highest associated mortality. [12] Explosions leading to structure collapse produce more orthopedic injuries. Land mine injuries are associated with a high risk of below- and above-the-knee amputations. Fireworks-related injuries prompt an estimated 10,000-12,000 ED visits in the United States annually, with 20-25% involving either the eye or the hand.
In a study of firework-related injuries treated in EDs in the United States, the rate was higher for children, with the highest rates being observed for 10-19 year olds (7.28 per 100,000 persons) and 0-9 year olds (5.45 per 100,000 persons). The injury rate was nearly 3 times higher for males than for females (4.48 vs. 1.57 per 100,000 persons). The most common injuries (26.7%) were burns of the wrist, hand, and finger, followed by contusion or superficial injuries to the eye (10.3%); open wounds of the wrist, hand, and finger (6.5%); and burns of the eye (4.6%). [13, 14]
Presence of tympanic membrane (TM) rupture indicates that a high-pressure wave (at least 40 kilopascal [kPa], 6 psi) was present and may correlate with more dangerous organ injury. Between 2 and 32% of patients injured by a blast will have TM rupture. [10] Theoretically, at an overpressure of 100 kPa (15 psi), the threshold for lung injury, the TM routinely ruptures; however, an Israeli case series of 640 civilian victims of terrorist bombings contradicts traditional beliefs about a clear correlation between the presence of TM injury and coincidence organ damage. Of 137 patients initially diagnosed as having isolated eardrum perforation who were well enough to be discharged, none later developed manifestations of pulmonary or intestinal blast injury. Furthermore, 18 patients with pulmonary blast injuries had no eardrum perforation.
Similarly, in a review of 167 patients who sustained blast exposure in Iraq, TM perforation was noted to be poorly sensitive as a biomarker for more serious primary blast injury. Only 50% of patients with serious PBI demonstrated TM rupture in this review. [15]
In a study of the relationship between tympanic membrane perforation (TMP) and severity of blast injury, TMP was more prevalent in patients with moderate and severe injuries than in mildly injured patients (53.3% vs. 13.6%). Patients with TMP more often needed surgery, ICU hospitalization, and need for transfer to a level I trauma center. [16]
Mild traumatic brain injury (mTBI) from primary blast forces may have greater postconcussive sequelae than mTBI from blunt forces. In a pilot study of 12 veterans with pure blast-force mTBI and 12 with pure blunt-force mTBI, both groups scored significantly lower than normal on the Rivermead Post-Concussion Questionnaire and the SF36-V Health Survey, but the blast-force group had lower scores than the blunt-force group on the Paced Auditory Serial Addition Test. Significant correlations of test scores with hypometabolism in the right superior parietal region on PET scanning were seen only in the blast-force injury group. [17]
Severe head injury was the most common cause of death in a retrospective review of 71 casualties who reached medical treatment facilities alive but subsequently died from injuries sustained during combat operations in Afghanistan and Iraq. Thirty-three casualties (47%) died from isolated head injuries, and another 13 (18%) had unsurvivable head injuries but not in isolation. Hemorrhage following severe lower limb trauma, often in conjunction with abdominal and pelvic injuries, was the cause of a further 15 deaths (21%). [18]
-
Blast injuries. Idealized graph of a blast pressure wave over time. Courtesy of Bowen TE and Bellamy RF, eds, Emergency War Surgery. Washington, DC: United States Government Printing Office, 1988.
-
Blast injuries. Estimated human tolerances for single, sharp, rising blast waves. Courtesy of Bowen TE and Bellamy RF, eds, Emergency War Surgery. Washington, DC: United States Government Printing Office, 1988.




