Practice Essentials
Pelvic ultrasonography is one of the best imaging modalities used to evaluate nonspecific pelvic pain, pregnancy complications, anatomy of pelvic organs, and various ovarian pathologies. [1, 2, 3, 4, 5] Ultrasound is the key modality for evaluation of contents of the female pelvis. It allows ready (and portable) imaging of the uterus, ovaries, and other structures at a reasonable cost and without ionizing radiation. Lack of irradiation is important because the ovary in young patients and in those of reproductive age is particularly sensitive to radiation. [6]
Pelvic ultrasonography is performed via a transabdominal (TA) or transvaginal (TV) approach. A urine-filled bladder helps lift the small bowel superiorly out of the pelvis, creating an optimal acoustic window and preventing bowel air from refracting or degrading the ultrasound beam. Ultrasound traverses the pelvis unimpeded through bladder fluid, insonating pelvic contents and returning to the transducer to be processed by the machine. [6]
In transabdominal ultrasonography, a low-frequency transducer and a full bladder are used to displace bowel gas and provide an acoustic window to improve image resolution while allowing a large viewing field of the pelvis. The transvaginal approach, also known as endovaginal scanning, is a painless procedure that resembles a pelvic exam. A thin, covered wand or probe is placed into the vagina, and the examiner directs the probe toward the uterus and ovaries. This type of ultrasound produces a better image than is attained by a scan through the abdominal wall because the probe can be positioned closer to the ovaries. This is the best test for diagnosing an ovarian cyst.
Endovaginal scanning, using a high-frequency transducer, is the preferred technique for evaluation of ovarian pathologies; a full bladder is not necessary. [2] Endovaginal scanning is preferred over computed tomography because of improved visualization of pelvic organs, the absence of radiation exposure with ultrasonography, decreased length of hospital stay, and reduced cost for the patient. [3]
According to practice parameters of the American Institute of Ultrasound in Medicine (AIUM), indications for pelvic ultrasonography of the female pelvis include, but are not limited to, the following [7] :
-
Evaluation of pelvic pain; pelvic masses; endocrine abnormalities, including polycystic ovaries; dysmenorrhea (painful menses); amenorrhea; abnormal uterine bleeding; postmenopausal bleeding; delayed menses; signs or symptoms of pelvic infection; congenital uterine, gonadal, and lower genital tract anomalies; excessive bleeding, pain, or signs of infection after pelvic surgery, delivery, or abortion; and incontinence of pelvic organ prolapse.
-
Follow-up of a previously detected abnormality.
-
Evaluation, monitoring, and/or treatment of patients with infertility.
-
Evaluation when clinical examination of the pelvis is limited.
-
Further characterization of a pelvic abnormality noted on another imaging study.
-
Localization of an intrauterine device (IUD).
-
Screening for malignancy in high-risk patients.
-
Guidance for interventional or surgical procedures.
-
Preoperative and postoperative evaluation of pelvic structures.
Use of ultrasound for the male pelvis is limited. The presence of free abdominal fluid can be assessed. Undescended testes in the groin and hernias can be seen with the use of high-frequency linear array transducers. Transabdominal ultrasound can allow visualization of the dilated urethra in posterior urethral valves. and,occasionally a valve itself can be seen in real time. Inferiorly angled midline views are most helpful. Transperineal ultrasonography can be utilized for diagnosis of posterior urethral valves. [6]
(The video below depicts a demonstration of transvaginal ultrasonography.)
-
Transabdominal longitudinal view of the female pelvis.
-
Transabdominal transverse view of the female pelvis: The bladder is rectangular. The ovaries are seen bilaterally in the adnexa.
-
Endovaginal longitudinal view of the uterus: The endometrial stripe (st) is thickened. The arcuate vessels (arc) can be seen within the uterus and should not be confused with free fluid in the cul-de-sac.
-
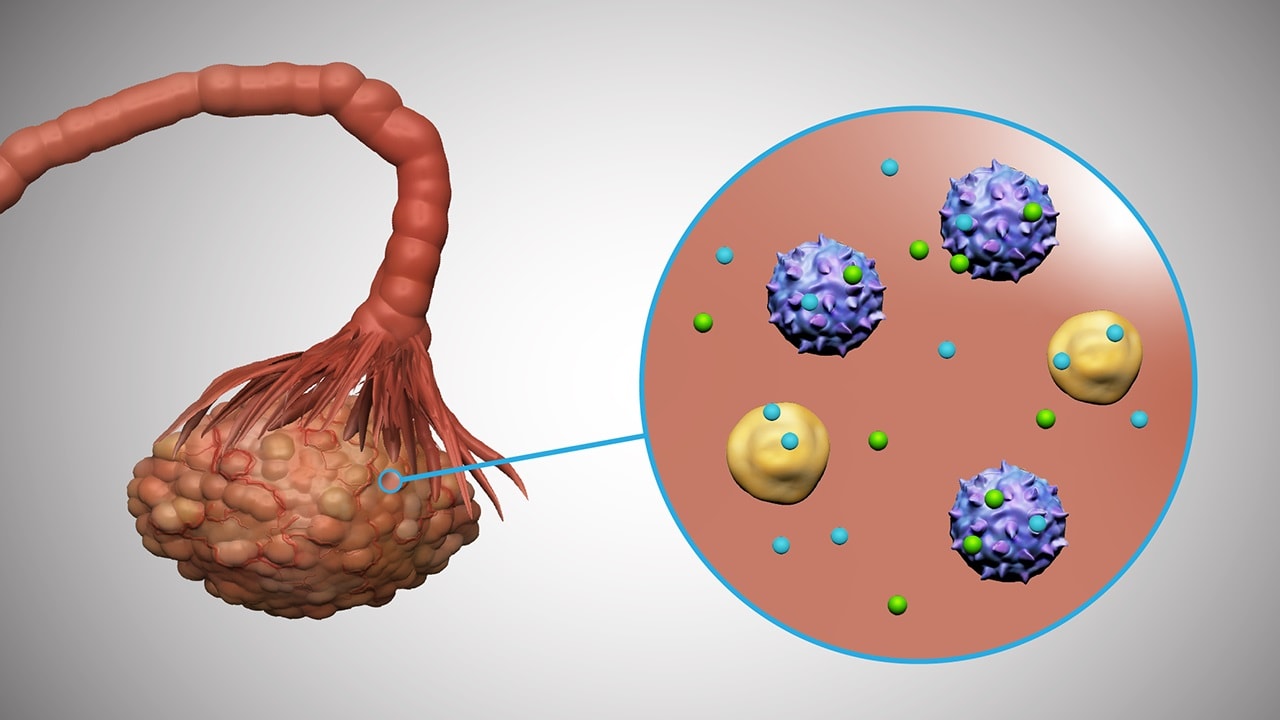
Endovaginal view of the ovary: Note its location adjacent to an iliac vessel.
-
Endovaginal ultrasound scan. Endometritis with air in the endometrial cavity and bilateral tubo-ovarian abscesses are shown.
-
Video depicts 2 findings: first, it shows an enlarged hypovascular left ovary; second, it shows flow in the healthy right ovary. A small amount of intraperitoneal fluid surrounds the left ovary.
-
Demonstration of a transvaginal ultrasonographic pelvic evaluation. Video courtesy of Meghan Kelly Herbst, MD. Also courtesy of Yale School of Medicine, Emergency Medicine.
-
Cine loop depicting transvaginal ultrasonography with free fluid in the uterus and right ovary. Video courtesy of Meghan Kelly Herbst, MD. Also courtesy of Yale School of Medicine, Emergency Medicine.
-
Cine loop of transvaginal ultrasonography showing free fluid in the uterus. Video courtesy of Meghan Kelly Herbst, MD. Also courtesy of Yale School of Medicine, Emergency Medicine.