Background
Infections involving the spinal canal include epidural abscesses (infection in the epidural space), meningitis (infection of the meninges), subdural abscesses (infections of the subdural space), and intramedullary abscesses (infections within the spinal cord). [1] Because the first 3 infections are discussed elsewhere (see Epidural and Subdural Infections, Meningitis), this article addresses only intramedullary abscesses.
Intramedullary spinal cord abscesses are extremely rare lesions. Since the original description in 1830 by Hart, approximately 100 cases have been reported. Their rarity, compared with brain abscesses, has been attributed to the relatively lower volume of the spinal cord and its particular blood supply.
Pathophysiology
Mechanisms of infection include (1) hematogenous spread from an extraspinal focus of infection, (2) contiguous spread from an adjacent focus of infection, (3) direct inoculation (ie, penetrating trauma, postneurosurgery), and (4) cryptogenic mechanisms (ie, no documented extraspinal focus of infection). In a 1998 review of 25 cases, hematogenous spread accounted for 8%, contiguous spread accounted for 24%, direct inoculation accounted for 4%, and 64% were cryptogenic. [2] In children, the abscesses are associated with prior anatomic spinal canal defects, such as dermal sinus tracts, which result from the incomplete partition of epithelial ectoderm and neuroectoderm in early fetal life.
Bacteria, such as staphylococci and streptococci, are the most common organisms responsible for these infections. Infections may also be caused by viral, fungal, or parasitic organisms. A diverse list of pathogens include, but are not limited to, cysticercosis, Mycobacterium tuberculosis, Listeria monocytogenes, Toxoplasma gondii, Nocardia asteroides, Histoplasma capsulatum, brucellosis, and the tapeworm spargana.
Initially, the area of the bacterial nidus is infiltrated with polymorphonuclear cells, leading to a suppurative myelitis. This evolves into central necrosis and liquefaction, which can spread along the long spinal tracts. Although the average extent of the process before 1975 was 6 vertebral levels, the average current length appears to be 3 levels. This change may be due to earlier detection and more effective antibiotics. At the periphery of this infectious process, fibroblasts proliferate and the central purulent area eventually becomes encapsulated by fibrous granulation tissue. The most commonly affected area is the dorsal thoracic spinal cord.
Epidemiology
Frequency
International
Various reviews of the literature describe different numbers, with a range of approximately 80-100 cases since the first description in 1830. In a 2003 review, only 38 pediatric cases were identified in the medical literature since 1830. [3]
Mortality/Morbidity
Although the first reported cases had high mortality rates, prognosis has improved significantly with the advent of antibiotics.
The mortality rate without surgical intervention is practically 100%, and those patients who died despite surgery almost exclusively were affected in the preantibiotic era.
The current mortality rate (cases reported in the last 2 y) is 8-12%, although 70% of survivors had persistent neurologic deficits.
In a review of 38 pediatric cases, 20% died, 60% had residual neurologic deficits, and only 20% recovered without sequelae. [3]
A study of veterans with traumatic spinal cord injury shows the need for preventative strategies, particularly for managing cardiovascular complications, to decrease mortality. [4]
Race-, sex-, and age-related demographics
Ethnic preference does not appear to exist, although some geographic differences are present. All intramedullary paracoccidioidomycosis cases were reported in Brazil.
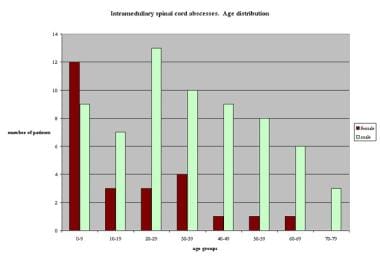
In one study in which sex was reported, spinal cord infections were 2.5 times more common in males than in females.
All ages are affected though children younger than 5 years are more likely affected. [5]
Female patients are affected mainly in the first 4 decades of life, whereas the incidence among male patients is distributed more evenly, with a peak in the third decade of life (see the image below).
-
Graph showing age distribution of 91 patients with intramedullary spinal cord abscess. The age or gender of 14 patients is unknown.