Background
Salmonella are gram-negative facultative intracellular anaerobes that cause a wide spectrum of disease. This spectrum can range from a gastroenteritis, enteric fever (caused by typhoid and paratyphoid serotypes), bacteremia, focal infections, to a convalescent lifetime carrier state. The type of infection depends on the serotype of Salmonella and host factors. It maintains a broad host range and, for unknown reasons, results in different diseases in different hosts.
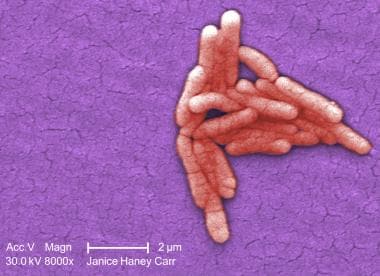 Under a moderately high magnification of 8000X, this colorized scanning electron micrograph (SEM) revealed the presence of a small grouping of gram-negative Salmonella typhimurium bacteria that had been isolated from a pure culture. Image courtesy of the Centers for Disease Control and Prevention, Bette Jensen, and Janice Haney Carr.
Under a moderately high magnification of 8000X, this colorized scanning electron micrograph (SEM) revealed the presence of a small grouping of gram-negative Salmonella typhimurium bacteria that had been isolated from a pure culture. Image courtesy of the Centers for Disease Control and Prevention, Bette Jensen, and Janice Haney Carr.
Although the taxonomy of Salmonella can be confusing, all salmonella serotypes are members of a single species, Salmonella enterica. More than 2500 serovars [1, 2] have been described, of which humans are almost exclusively infected by Salmonella enterica subspecies enterica serotypes Typhi, Typhimurium, and Choleraesuis worldwide. [3] The name generally refers to where the serotype was isolated. In the United States, Salmonella serotype Enteritidis (2.6 per 100,000 population), Salmonella serotype Newport (1.4) and Typhimurium (1.3) account for nearly half of the human isolates. [4, 5]
Salmonellosis caused by Salmonella Enteritidis is the most common bacterial infectious cause of food-borne disease in the United States second to norovirus as the most common overall cause of foodborne disease outbreaks. [6, 7] Ninety-five percent of cases of Salmonella infection are food-borne; however, the incidence of direct contact exposure with animal carriers is on the rise. [6] Once infected, salmonellosis harbors a significant morbidity and mortality. One third of untreated patients experience complications and account for three fourths of deaths associated with salmonellosis. [3] Campylobacter and Salmonella are the most common bacterial pathogens found in stool cultures recovered from patients presenting with gastroenteritis or severe diarrhea. [1, 5]
Salmonella has a widespread distribution in the environment and certain host factors make humans particularly susceptible to infection. Its increasing antimicrobial resistance, prevalence, virulence, and adaptability are a challenge worldwide.
Pathophysiology
Salmonella infections most commonly begin with ingestion of bacteria in contaminated food or water. However, direct contact with animal and human carriers has also been implicated. Reptile and amphibian carriers are the most commonly recognized sources of direct contact. [6] Transmission may also occur from mother to fetus transplacentally. [8] Studies involving healthy human volunteers required a median dose of 1 million bacteria to produce disease. However, point outbreaks suggest as few as 200 bacteria may produce nontyphoid gastroenteritis. [1]
Once the bacteria survive the acidic stomach, they colonize the intestine and translocate across the intestinal epithelium via 3 routes: (1) invasion of the enterocytes, (2) invasion of epithelial cells called M cells, and (3) through dendritic cells that intercalate epithelial cells. Interaction with the epithelium and resident cells promote a proinflammatory response to include cytokines, chemokines, neutrophils, macrophages, dendritic cells, and T and B cells. This inflammatory host response can actually benefit the intestinal pathogens and contribute to the nature and severity of the infection by establishing a competitive advantage against the native flora. [9] Animal studies reveal that prolonged antibiotic use may disrupt this host susceptibility as well. [10]
After crossing this epithelial layer, the bacteria replicate in macrophages in Peyer’s patches, mesenteric lymph nodes, and the spleen. Once colonized, the bacteria may then potentially disseminate to the lungs, gallbladder, kidneys, or central nervous system. When transferring to a new host cell every 1-7 days, it is unknown how and why Salmonella escapes extracellular fluid containing antibodies. [11] The nontyphoid species of Salmonella tend to produce a more localized response because they are believed to lack the human-specific virulence factors. However, the typhi serotype can develop the more invasive disease resulting in bacteremia. The severity of disease is related to the serotype, number of organisms, and host factors.
Eggs and poultry are the most common sources of infection. [6, 12] Ingestion of contaminated water, milk, milk products, beef, fruit, vegetables, and dairy products are also common sources. Potential sources of infection for infants with Salmonella are exposure to reptiles, riding in a shopping cart next to meat or poultry, or consuming liquid infant formula. [13] Outbreaks have been associated with contaminated frozen potpies, puffed vegetable snacks, and exposure to turtles. [2] More recently, multistate human outbreaks have been seen in contaminated dry dog food and peanut butter products. [14, 15]
Reservoirs of the bacteria include humans, poultry, swine, cattle, rodents, and pets such as iguanas, tortoises, turtles, terrapins, chicks, dogs, and cats. Up to 90% of reptiles and amphibians harbor Salmonella in their gastrointestinal tracts and 6% of nontyphoid disease is related to direct contact with these animals. [6]
Fecal-oral transmission from person to person in areas with poor sanitation and contaminated or nonchlorinated water is the route for enteric or typhoid fever. Humans are the only known carriers of Salmonella typhi. [6]
Individual susceptibility to Salmonella infection increases with extremes of age, immunodeficiency states, prior antibiotic use, neoplastic disease, achlorhydria or antacid use, recent bowel surgery, and malnutrition.
Epidemiology
Frequency
United States
Prevalence estimates vary secondary to inconsistent diagnosis and reporting techniques. It is estimated that only 3% of Salmonella infections are laboratory confirmed and reported to the Centers for Disease Control and Prevention (CDC). However, an estimated 1.4 million people in the United States are infected with nontyphoid Salmonella annually at a cost of $365 million in direct medical costs. [16]
The overall incidence of Salmonella infection has not changed much compared to 2016-2018 due to a decreased incidence for Typhimurium (13%) with an increase in Infantis (69%). [4, 5] The true burden of nontyphoid Salmonella in the United States is calculated to be 520 cases per 100,000 compared with 17.1 cases per 100,000 of laboratory-confirmed cases annually, taking into account approximately 38.6 cases of nontyphoid Salmonella for each culture-confirmed case. [17, 18] The reported 2019 culture-confirmed incidence is 17.1 cases per 100,000. [4, 5]
Additionally, an estimated 500 people are infected with typhoid Salmonella annually. [6] Most cases of documented typhoid disease in the United States are related to foreign travel to developing nations such as India (30%), Pakistan (13%), Mexico (12%), Bangladesh (8%), Philippines (8%), and Haiti (5%). [6]
International
Fully industrialized nations report frequencies of gastroenteritis similar to that of the United States. However, worldwide estimates of nontyphoid Salmonella range from 200 million to 1.3 billion, with an estimated death toll of 3 million each year. [19]
The serovars responsible for typhoid or enteric fever, typhi and paratyphi, that cause systemic illness lead to an estimated 21.7 million cases and 217,000 deaths worldwide, of which paratyphoid fever accounts for 5.4 million cases. [20] Salmonella Typhi is estimated to outweigh Salmonella Paratyphi by a ratio of about 4:1 in endemic countries. [21] Compared with tourists, travelers visiting friends or relatives in developing nations exhibit a much higher incidence of typhoid or enteric fever. [6] Eighty percent of the total typhoid fever cases and deaths occur in Asia; the rest mainly occur in Africa and Latin America. [22]
Salmonella is identified as a major cause of invasive bacterial febrile illness across sub-Saharan Africa, with a high prevalence of resistance against first-line antimicrobials in both S typhi and invasive nontyphoidal Salmonella. [23]
Mortality/Morbidity
Twenty percent of patients require hospitalization, with an estimated death rate of 0.6%. [18] Infection with drug-resistant nontyphoid Salmonella and Salmonella typhi increase the likelihood of hospitalization and death. [18]
Invasive nontyphoid Salmonella infection occurs in about 5% of cases in Israel [18] and is responsible for 400-600 deaths in the United States each year. [6] Mortality for nontyphoid Salmonella is reported to be as high as 60% in African patients with HIV. [24] Mycotic abdominal aortic aneurysms are more common in immunocompromised and HIV patients.
The case fatality rate (CFR) in immunocompetent individuals for nontyphoid Salmonella is estimated to be 0.0003-0.003%. However, recent studies have shown that the invasive CFR is estimated to be as high as 37% in Kenyan adults, 47% in Malawian adults, and 12% in African children. [25]
Treated typhoid cases have a 2% mortality rate with a 15% relapse rate. [3] A significant number of typhoid patients become chronic asymptomatic carriers and can shed high numbers of bacteria in the stool for a lifetime without obvious symptoms. [24] Depending on the serotype, roughly 1% of adults and 5% of children excrete organisms for greater than a year. [26]
Age
Attack rates are highest in persons younger than 20 years or older than 70 years. The highest rate is found in infants (130 isolates/100,000). One quarter to one third of pediatric typhoid patients are younger than 5 years, of which 6-21% are younger than 2 years. [22]
The clinical appearance of the disease varies in children, especially among very young children. [27]
Neonates are at a greater risk to fecal-oral transmission secondary to relative decreased stomach acidity and buffering of ingested breastmilk and formula.
Invasive Salmonella infection is most prevalent among infants in the United States. [28]
Additional links to nontyphoid Salmonella infection in children identified include powdered formula, pet ownership, and recent antibiotic use. [29]
Elderly persons are at a relative greater risk to infection secondary to chronic underlying illness and weakened immunity. Nursing home residents have a particularly higher risk. The case-fatality rate (CFR) is estimated at 1.3% for nontyphoid Salmonella among those aged 50 years or older.
Prognosis
Nontyphoid Salmonella is generally self-limiting. Most patients are treated on an outpatient basis. Extremes of age and an immunocompromised state increases morbidity and mortality.
Typhoid Salmonella generally requires treatment. Mortality rate for treated cases is 2%, while complications occur in 30% of untreated cases. [3] Morbidity and mortality increases with drug-resistant S typhi. [18]
Patient Education
Emphasize good hand-washing, thorough cleaning of cooking utensils, appropriate food preparation techniques, and adequate cooking temperature for killing the bacteria.
-
Under a moderately high magnification of 8000X, this colorized scanning electron micrograph (SEM) revealed the presence of a small grouping of gram-negative Salmonella typhimurium bacteria that had been isolated from a pure culture. Image courtesy of the Centers for Disease Control and Prevention, Bette Jensen, and Janice Haney Carr.







