Background
Prostatitis is an infection or inflammation of the prostate gland that presents as several syndromes with varying clinical features. The term prostatitis is defined as microscopic inflammation of the tissue of the prostate gland and is a diagnosis that spans a broad range of clinical conditions.
The National Institutes of Health (NIH) has recognized and defined a classification system for prostatitis in 1999. [1] The 4 syndromes of prostatitis are as follows:
-
I - Acute bacterial prostatitis [2]
-
II - Chronic bacterial prostatitis [2]
-
III - Chronic prostatitis and chronic pelvic pain syndrome (CPPS; further classified as inflammatory or noninflammatory)
-
IV - Asymptomatic inflammatory prostatitis
Acute prostatitis and chronic bacterial prostatitis are defined by documented bacterial infections of the prostate and are treated with antibiotic therapy and supportive care (see Treatment). [2]
CPPS is characterized primarily by urological pain complaints in the absence of urinary tract infection and is the most common form of prostatitis, representing 90% of all cases. [2, 3] This syndrome excludes the presence of active urethritis, urogenital cancer, urinary tract disease, significant urethral stricture, or neurological disease affecting the bladder. It is subdivided into inflammatory and noninflammatory subtypes. Inflammatory CPPS is defined by the presence of white blood cells in the semen, expressed prostatic secretions, or voided bladder urine after prostatic massage, whereas noninflammatory CPPS is defined by the absence of white blood cells. While the etiology of CPPS is poorly understood, it likely is multifactorial and could be influenced by occult infections, autoimmune, psychological, or neuromuscular conditions. [4, 5, 6] This condition can have impacts on sperm quality and fertility. A meta-analysis conducted by Fu et al demonstrated an association between impaired metrics of sperm quality (concentration, motility, and morphology) and CPPS, [7] potentially due to the increase in cytokines associated with impaired sperm quality found in analyses of semen from patients with CPPS. [8, 9, 10]
Asymptomatic inflammatory prostatitis is characterized by elevated white blood cells in the ejaculate (leukocytospermia) and elevated prostate-specific antigen (PSA) levels in the absence of associated infection and genitourinary symptoms. [11, 6] Typically, this condition is diagnosed incidentally during workups for infertility and is associated with benign prostatic hypertrophy. [12] Though some physicians will treat this condition with antibiotics for potential occult infection there is little evidence to support this practice and due to its lack of clinical symptoms treatment is not required. [6, 13] Additionally, while prostate cancer is also associated with elevated levels of PSA, a study by Stancik et. al demonstrated that the two conditions can be differentiated by the ratio of free-to-total PSA. [14] See the following for more information:
Patient education
For patient education information, see the Prostate Health Center, as well as Prostate Infections.
Pathophysiology
In bacterial prostatitis, sexual transmission of bacteria is common, but hematogenous, lymphatic, and contiguous spread of infection from surrounding organs must also be considered. [2]
A history of sexually transmitted diseases is associated with an increased risk for prostatitis symptoms.
Prostatitis is characterized by the presence of acute inflammatory cells in the glandular epithelium and lumens of the prostate, with chronic inflammatory cells in the periglandular tissue (see the image below). However, the presence and quantity of inflammatory cells in urine or prostatic secretions does not correlate with the severity of the clinical symptoms.
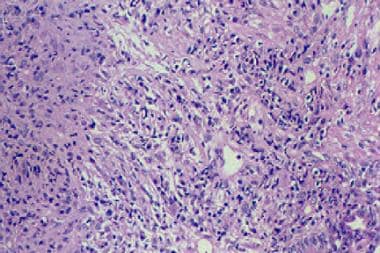 A nonspecific mixed inflammatory infiltrate that consists of lymphocytes, plasma cells, and histiocytes is typical in chronic bacterial prostatitis.
A nonspecific mixed inflammatory infiltrate that consists of lymphocytes, plasma cells, and histiocytes is typical in chronic bacterial prostatitis.
Chronic pelvic pain syndrome is diagnosed based on pain in the setting of negative cultures of urine and prostatic secretions. Neuromuscular dysfunction or congenital reflux of urine into the ejaculatory and prostatic ducts may be a precipitating factor.
Viral and granulomatous prostatitis may be associated with HIV infection and is another cause of culture-negative disease. A common viral pathogen of prostatitis in HIV-infected patients is cytomegalovirus (CMV). [15] Mycobacteria, such as Mycobacterium tuberculosis, and fungi, such as Candida albicans, have also been associated with culture-negative disease in this population. [16]
Etiology
Acute bacterial prostatitis may be caused by ascending infection through the urethra, refluxing urine into prostate ducts, or direct extension or lymphatic spread from the rectum. Approximately 80% of the pathogens are gram-negative organisms (eg, Escherichia coli, Enterobacter, Serratia, Pseudomonas, Enterococcus, and Proteus species). [2, 17, 18] Mixed bacterial infections are uncommon. Though the majority of cases can be attributed to the aforementioned bacteria, there is one case report of prostatitis secondary to Aeromonas hydrophila and A caviae that the patient acquired while cave diving in Florida. [19]
Consider Neisseria gonorrhoeae and Chlamydia trachomatis infection in any male younger than 35 years presenting with urinary tract symptoms.
Nursing home patients with indwelling urethral catheters may also be at increased risk for acute bacterial prostatitis. Sclerotherapy for rectal prolapse may also increase risk. [20]
Chronic bacterial prostatitis may be due to the following [2] :
-
A primary voiding dysfunction problem, either structural or functional
-
E coli is responsible for 75-80% of chronic bacterial prostatitis cases. Enterococci and gram-negative aerobes such as Pseudomonas are usually isolated in the remainder of cases.
-
C trachomatis,Ureaplasma species, Trichomonas vaginalis
-
Uncommon organisms, such as M tuberculosis and Coccidioides, Histoplasma, and Candida species must also be considered. Tuberculous prostatitis may be found in patients with renal tuberculosis
-
Human immunodeficiency virus
-
Cytomegalovirus
-
Inflammatory conditions (eg, sarcoidosis)
The etiology of chronic prostatitis and chronic pelvic pain syndrome is poorly understood but may involve an infectious or inflammatory initiator that results in neurologic injury and pelvic floor dysfunction characterized by increased pelvic tone. [21] The most prevalent site of pain is perineal (63% of patients), followed by testicular, pubic, and penile. Urogenital pain appears to be more bothersome to patients than urinary symptoms. Inflammatory bowel disease is present in 25% of patients with CPPS. [22] About 5-8% of men with this syndrome eventually have a bacterial pathogen isolated from urine or prostatic fluid.
Causes of chronic prostatitis and chronic pelvic pain syndrome may include the following:
-
Functional or structural bladder pathology, such as primary vesical neck obstruction, pseudodyssynergia (failure of the external sphincter to relax during voiding), impaired detrusor contractility, or acontractile detrusor muscle
-
Ejaculatory duct obstruction
-
Increased pelvic side wall tension
-
Nonspecific prostatic inflammation
The causes of asymptomatic inflammatory prostatitis are poorly understood.
Epidemiology
United States statistics
Prostatitis is one of the most common diseases seen in urology practices in the United States, accounting for nearly 2 million outpatient visits per year. [23, 24, 25] The diagnosis is made in approximately 25% of male patients presenting with genitourinary symptoms. Autopsy studies have revealed a histologic prevalence of prostatitis of 64-86%.
Approximately 8.2% of men have prostatitis at some point in their lives. [21] Among the 4 categories of prostatitis, the most common is chronic prostatitis/chronic pelvic pain syndrome, accounting for 90-95% of prostatitis cases. Acute bacterial prostatitis and chronic bacterial prostatitis each make up another 2-5% of cases. Because asymptomatic inflammatory prostatitis is only identified incidentally, its overall prevalence is difficult to estimate.
International statistics
The prevalence of prostatitis amongst men in North America, Europe, and Asia is estimated to be between 2-10% [26]
Age-related demographics
In patients younger than 35 years, the most common variant of the syndrome is acute bacterial prostatitis. HIV-related disease is also predominantly seen in younger patients.
Among older patients, nonbacterial prostatitis (National Institutes of Health [NIH] types II and IV) are the most common. Of importance, rare causes of prostatitis should be sought during evaluation. According to case reports of Wegener granulomatosis in the fourth and fifth decades of life, prostatitis can be a presenting feature of Wegener granulomatosis and a clinical manifestation of relapse. [27, 28, 29] Fungal infection with coccidioidomycosis, blastomycosis, histoplasmosis, cryptococcosis, candidiasis, aspergillus and paracocci-dioidomycosis and mycobacterial infection with M tuberculosis also have been reported. [6]
Prognosis
The prognosis in patients with the first occurrence of acute bacterial prostatitis is good with aggressive antibiotic therapy and good patient compliance. Lack of treatment with antibiotics increases risk for impaired fertility, epididymitis, chronic prostatitis, and prostatic abscess formation. [30] In patients with chronic prostatitis with acute exacerbations, causative underlying factors may affect overall prognosis.
Prostatitis may lead to urosepsis with significant associated mortality in patients with diabetes mellitus, patients on dialysis for chronic renal failure, patients who are immunocompromised, and postsurgical patients who have had urethral instrumentation.
Chronic prostatitis and asymptomatic inflammatory prostatitis have not been definitively linked to the development of prostate cancer.
-
Bacterial prostatitis. Expressed prostatic fluid contains more than 10 white blood cells per high-power field, indicating prostatitis.
-
A nonspecific mixed inflammatory infiltrate that consists of lymphocytes, plasma cells, and histiocytes is typical in chronic bacterial prostatitis.
-
Urine culture with greater than 100,000 colony-forming units (CFU) of Escherichia coli, the most common pathogen in acute and chronic prostatitis. Chronic bacterial prostatitis must be confirmed and diagnosed using a urine culture.
-
Treatment algorithm for chronic bacterial prostatitis. Courtesy of Frontiers Media [Xiong S, Liu X, Deng W, Zhou Z, Li Y, Tu Y, et al. Pharmacological Interventions for Bacterial Prostatitis. Front Pharmacol. 2020. 11:504. Online at https://www.frontiersin.org/articles/10.3389/fphar.2020.00504/full].
-
Treatment algorithm for acute bacterial prostatitis. Courtesy of Frontiers Media [Xiong S, Liu X, Deng W, Zhou Z, Li Y, Tu Y, et al. Pharmacological Interventions for Bacterial Prostatitis. Front Pharmacol. 2020. 11:504. Online at https://www.frontiersin.org/articles/10.3389/fphar.2020.00504/full].









