Background
A lung abscess is a subacute infection in which an area of necrosis forms in the lung parenchyma. It usually is in a dependent section of the lung, more often involves the right lung than the left, and is most commonly seen after aspiration of oropharyngeal secretions. Lung abscesses have a slow, insidious presentation and usually develop 1-2 weeks after the initial aspiration event. A lung abscess is shown in the image below.
Empyema is defined as pus in the pleural space. It typically is a complication of pneumonia. However, it can also arise from penetrating chest trauma, esophageal rupture, complication from lung surgery, or inoculation of the pleural cavity after thoracentesis or chest tube placement. An empyema can also occur from extension of a subdiaphragmatic or paravertebral abscess.
Pathophysiology
A lung abscess involves the lung parenchyma, whereas an empyema involves the pleural space. [1] In many patients with pneumonia, a sterile simple parapneumonic effusion develops in the pleural space. If this pleural effusion becomes infected, it is labeled a complicated parapneumonic effusion, whereas the presence of frank pus in the pleural space defines an empyema.
The development stages of an effusion can be divided into three phases: exudative, fibropurulent, and organizational. The initial effusion develops from increased pulmonary interstitial fluid along with progressive capillary vascular permeability. A simple effusion is frequently sterile and resolves with antibiotic treatment of the underlying pulmonary infection.
In 5-10% of the patients with a pleural effusion, the effusion becomes infected and neutrophils buildup. This inflammatory response, shown in the images below, also causes the production of chemokines, cytokines, oxidants, and protease mediators.
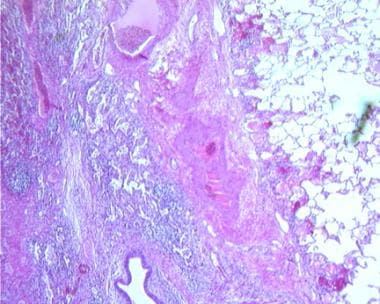 Empyema and Abscess Pneumonia. Histology of a lung abscess shows dense inflammatory reaction (low power).
Empyema and Abscess Pneumonia. Histology of a lung abscess shows dense inflammatory reaction (low power).
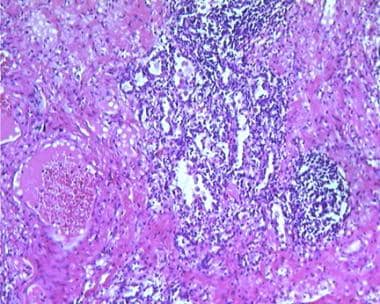 Empyema and Abscess Pneumonia. Histology of a lung abscess shows dense inflammatory reaction (high power).
Empyema and Abscess Pneumonia. Histology of a lung abscess shows dense inflammatory reaction (high power).
This more complicated parapneumonic effusion requires both antibiotics and some form of surgical drainage or alternative treatment modality to remove the purulent effusion. In these more complicated effusions, decreased fibrinolysis and activation of the coagulation cascade leads to the production of fibrin with subsequent adhesions and loculated fluid collections. This process ultimately can cause pleural fibrosis and impairment of lung expansion.
Etiology
The most common cause of lung abscess is aspiration. Risk factors include the following:
-
Poor dentition, periodontal infection [2]
-
Seizure disorder
-
Alcohol and drug abuse
-
Electronic cigarette use [3]
-
Diabetes mellitus
-
COVID-19 [4]
-
Gastroesophageal reflux disease
-
Inability to protect the airway because of an absent gag reflex (eg, patients who are comatose, have a change in mentation or bulbar dysfunction, [5] or who might be undergoing general anesthesia)
-
Primary lung disorders, such as septic emboli, pulmonary vasculitis, cavitating lung malignancy, or pulmonary cystic disease
-
Penetrating chest trauma
-
Immunosuppression
-
Conditions associated with septic emboli, including intravenous drug use, soft tissue infections, valvular heart disease, and individuals with intravascular prosthetic material
Polymicrobial bacteria can be found in over 90% cases of lung abscess. [6] The microbiologic organisms are typically oral flora, including Bacteroides, Fusobacterium, and Peptostreptococcus species. Other organisms include Pseudomonas species, Klebsiella species, Staphylococcus aureus, Streptococcus pneumoniae, Streptococcus milleri, Nocardia species, and less commonly fungi and parasites. Immunosuppressed individuals are at increased risk for more opportunistic pathogens associated with lung abscess, including Mycobacterium tuberculosis (especially in cases of immigration from Africa or Asia), Pseudomonas, Klebsiella, Nocardia, and fungi. [7]
Klebsiella pneumoniae has been shown to have a significant preponderance for severe, necrotizing pneumonia and subsequent development for cavitary lesions and lung abscesses. [7] A Taiwanese study found an increasing incidence of K pneumoniae in community-acquired lung abscesses. [8] However, there is a higher incidence of K pneumoniae related infection found in Taiwan, and this trend may not translate to the US and other parts of the world. [9] Staphylococcus aureus is the most common isolated pathogen of lung abscess in children. [6]
The most common cause of an empyema is from a parapneumonic effusion that becomes infected; these account for about half of all empyemas. Other causes of an empyema include the following:
-
Penetrating chest trauma
-
Undrained hemothoraces, including those secondary to blunt chest trauma
-
Contamination of a wound during procedures such as needle decompression, chest tube placement, thoracentesis, or thoracic surgery
Microbiologic organisms that can cause an empyema include Streptococcus species such as Streptococcus milleri (Streptococcus intermedius, Streptococcus constellatus, and Streptococcus anginosus), S pneumoniae, Staphylococcus aureus and methicillin-resistant Staphylococcus aureus (MRSA), and a variety of gram-negative organisms and anaerobes. [10, 11] Anaerobic involvement, either as sole organism or part of a polymicrobial infection, is common in empyemas but may be difficult to detect on cultures. [11] One should always consider enterobacteria, enterococci, and Mycobacterium tuberculosis as potential pathogens.
Bacteria from the Streptococcus milleri group have become the predominant organism cultured from adults with empyemas, especially in patients with underlying malignancy or diabetes mellitus. Recently, the incidence of staphylococcal-related empyema has increased.
In the pediatric population, S pneumoniae remains the predominant organism associated with empyemas. S aureus and Pneumococcal serotypes 1, 3, and 19A, possibly secondary to the widespread use of the pneumococcal conjugate vaccine, have seen dramatic increases more recently. [12]
Epidemiology
United States data
The rates of lung abscess have dropped significantly since the development of antibiotics. The frequency of lung abscess varies depending on underlying comorbidities and occurs most frequently in individuals with risk factors for aspiration (stroke, dementia, alcoholism, gastric reflux, and poorly controlled epilepsy), immunocompromise, malignancy, intravenous drug use, poor dental hygiene, and diabetes mellitus. [1]
In the 1940s, the rates of empyema had dropped precipitously with the advent of antibiotics, but, from 1996 to 2008, the rate of empyema nearly doubled across all age groups. This increase is partly explained by the rapid increase of antibiotic resistance but, interestingly, is theorized to have occurred secondary to a replacement phenomenon. The heptavalent pneumococcal vaccine had dramatically decreased the overall incidence of pneumococcal infections but had increased the incidence of nonvaccine pneumococcal serotypes 1, 3, and 19A and nonpneumococcal infections, especially Staphylococcus aureus, that are thought to confer a higher conversion from pneumonia to complicated pneumonia and empyema. Since 2010, a 13-valent pneumococcal conjugate vaccine has been available, which includes the 1, 3, and 19A serotypes. [12, 13]
Most empyemas are complications of pneumonia, but up to 20% are secondary to iatrogenic causes, including but not limited to, thoracic surgeries, chest tube insertion, or thoracentesis. Three percent of empyemas are estimated to occur as complications of chest trauma. [14]
Sex- and age-related statistics
A population study revealed that nearly 65% of individuals with parapneumonic empyema are male. [10] No studies have revealed male gender as an independent risk factor for empyema. [15, 16] This disparity may be attributed to gender-related risk factors, including alcohol abuse, drug use, and delay to treatment.
Lung abscesses are more common in individuals with comorbid conditions often found with increasing age, including dementia and malignancy.
There is an increased risk of parapneumonic empyema with extremes of age with rates of 7.6 and 9.9 cases per 100,000 for ages younger than 5 years and older than 64 years, respectively. Rates for empyema between ages of 5 and 64 years range from 1.9-5.4 cases per 100,000. [10, 13]
Prognosis
The prognosis for both lung abscess and empyema generally is good. Ninety percent of lung abscesses are cured with medical management alone.
Morbidity/mortality
The mortality rate for lung abscesses in adults can reach as high as 15-20%, [17] whereas children have mortality rates typically below 5%. Mortality is largely dependent on comorbid conditions. Healthy individuals generally have a very good prognosis while immunosuppression, malignancy, nosocomial infections, reduced level of consciousness, anemia, and low albumin portend a poorer prognosis. Lung abscesses secondary to Pseudomonas aeruginosa, Staphylococcus aureus, and Klebsiella pneumoniae infections have high mortality rates. [17]
The case fatality rate in the United States for parapneumonic empyema is 7.2%, with rates increasing with age. The fatality rate in children is 0.4%, and is 16.1% in adults older than 64 years. [10] Mortality is increased for hospital acquired, S aureus, gram-negative, and mixed aerobic infections.
Complications
Complications of pulmonary abscess include pleural fibrosis, trapped lung, restrictive ventilatory defect, bronchopleural fistula, and pleurocutaneous fistula.
-
Empyema and Abscess Pneumonia. Histology of a lung abscess shows dense inflammatory reaction (low power).
-
Empyema and Abscess Pneumonia. A thick-walled lung abscess.
-
Empyema and Abscess Pneumonia. Pneumococcal pneumonia complicated by lung necrosis and abscess formation.
-
Empyema and Abscess Pneumonia. A lateral chest radiograph shows air-fluid level characteristic of lung abscess.
-
Empyema and Abscess Pneumonia. A 54-year-old patient developed cough with foul-smelling sputum production. A chest radiograph shows lung abscess in the left lower lobe, superior segment.
-
Empyema and Abscess Pneumonia. A 42-year-old man developed fever and production of foul-smelling sputum. He had a history of heavy alcohol use, and poor dentition was obvious on physical examination. Chest radiograph shows lung abscess in the posterior segment of the right upper lobe.
-
Empyema and Abscess Pneumonia. A 42-year-old man developed fever and production of foul-smelling sputum. He had a history of heavy alcohol use, and poor dentition was obvious on physical examination. Lung abscess in the posterior segment of the right upper lobe was demonstrated on chest radiograph. CT scan shows a thin-walled cavity with surrounding consolidation.
-
Empyema and Abscess Pneumonia. Chest radiograph of a patient who had foul-smelling and bad-tasting sputum, an almost diagnostic feature of anaerobic lung abscess.
-
Empyema and Abscess Pneumonia. Histology of a lung abscess shows dense inflammatory reaction (high power).











