Practice Essentials
Placenta previa is an obstetric complication that classically presents as painless vaginal bleeding in the third trimester secondary to an abnormal placentation near or covering the internal cervical os. However, with the technologic advances in ultrasonography, the diagnosis of placenta previa is commonly made earlier in pregnancy. Historically, there have been three defined types of placenta previa: complete, partial, and marginal. More recently, these definitions have been consolidated into two definitions: complete and marginal previa.
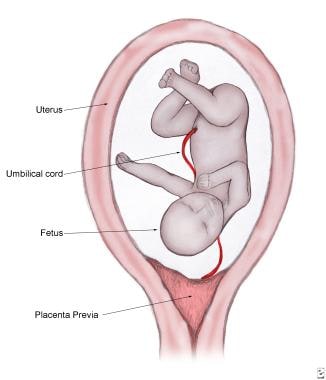
A complete previa is defined as complete coverage of the cervical os by the placenta. If the leading edge of the placenta is less than 2 cm from the internal os, but not fully covering, it is considered a marginal previa (see the following image). Because of the inherent risk of hemorrhage, placenta previa may cause serious morbidity and mortality to both the fetus and the mother.
Pathophysiology
Placental implantation is initiated by the embryo (embryonic plate) adhering in the lower (caudad) uterus. With placental attachment and growth, the developing placenta may cover the cervical os. However, it is thought that a defective decidual vascularization occurs over the cervix, possibly secondary to inflammatory or atrophic changes. As such, sections of the placenta having undergone atrophic changes could persist as a vasa previa.
A leading cause of third-trimester hemorrhage, placenta previa presents classically as painless bleeding. Bleeding is thought to occur in association with the development of the lower uterine segment in the third trimester. Placental attachment is disrupted as this area gradually thins in preparation for the onset of labor; this leads to bleeding at the implantation site, because the uterus is unable to contract adequately and stop the flow of blood from the open vessels. Thrombin release from the bleeding sites promotes uterine contractions and leads to a vicious cycle of bleeding–contractions–placental separation–bleeding.
Etiology
The exact etiology of placenta previa is unknown. The condition may be multifactorial and is postulated to be related to the following risk factors:
-
Advancing maternal age (>35 y)
-
Infertility treatment
-
Multiparity (5% in grand multiparous patients)
-
Multiple gestation
-
Short interpregnancy interval
-
Previous uterine surgery, uterine insult or injury
-
Previous or recurrent abortions
-
Previous placenta previa (4-8%)
-
Smoking
-
Cocaine use
Unlike first-trimester bleeding, second- and third-trimester bleeding is usually due to abnormal placental implantation.
Hemorrhaging, if associated with labor, would be secondary to cervical dilatation and disruption of the placental implantation from the cervix and lower uterine segment. As noted previously, the lower uterine segment is inefficient in contracting and thus cannot constrict vessels as in the uterine corpus, resulting in continued bleeding (see Pathophysiology).
Epidemiology
United States statistics
Placenta previa is frequently reported to occur in 0.5% of all US pregnancies. A large, US population-based, 1989-1997 study indicated an incidence of 2.8 per 1000 live births. [3] The risks increase 1.5- to 5-fold with a history of cesarean delivery. A meta-analysis showed that the rate of placenta previa increases with increasing numbers of cesarean deliveries, with a rate of 1% after 1 cesarean delivery, 2.8% after 3 cesarean deliveries, and as high as 3.7% after 5 cesarean deliveries. [1]
Racial and age-related differences in incidence
The significance of race in having a role in placenta previa is somewhat controversial. Some studies suggest an increased risk among Black and Asian women, whereas other studies cite no difference. [4, 5]
Advanced maternal age has also been strongly associated with an increasing incidence of placenta previa. The incidence of placenta previa after age 35 years reported to be 2%. A further increase to 5% is seen after age 40 years, which is a 9-fold increase when compared to females younger than 20 years. [6, 7]
Prognosis
Placenta previa complicates approximately 0.5% of all pregnancies. [4] Technologic advances in ultrasonography have increased the early diagnosis of placenta previa, and several studies have shown that a significant portion of these early diagnoses do not persist until delivery. [8, 9] In fact, 90% of all placentas designated as “low lying” on an early sonogram are no longer present on repeat examination in the third trimester. [10]
However, maternal and fetal complications of placenta previa are well documented. Preterm birth is highly associated with placenta previa, with 16.9% of women delivering at less than 34 weeks and 27.5% delivering between 34 and 37 weeks in a population-based study from 1989 to 1997. [3] A meta-analysis by Jansen et al showed that pooled proportions for the risk of preterm birth before 37, 34, 32 and 28 weeks of gestation in pregnant persons with placenta previa were 46%, 17%, 10%, and 2%, respectively. [11] There is a significant increase in the risk of postpartum hemorrhage and need for emergency hysterectomy in women with placenta previa. [12]
Maternal complications of placenta previa are summarized as follows:
-
Hemorrhage, [13] including rebleeding (Planning delivery and control of hemorrhage is critical in cases of placenta previa as well as placenta accreta, increta, and percreta.)
-
Placental abruption
-
Preterm delivery
-
Increased incidence of postpartum endometritis [14]
-
Mortality rate (2-3%); in the US, the maternal mortality rate is 0.03%, the great majority of which is related to uterine bleeding and the complication of disseminated intravascular coagulopathy
The Table, below, summarizes the relative risk of some morbidities in women with placenta previa.
Table. Relative Risk of Morbidities in Patients With Placenta Previa (Open Table in a new window)
Morbidities |
Relative Risk |
Antepartum bleeding |
10 |
Need for hysterectomy |
33 |
Blood transfusion |
10 |
Septicemia |
5.5 |
Thrombophlebitis |
5 |
Endometritis |
6.6 [14] |
Complications of placenta previa in the neonate/infant are summarized as follows:
-
Congenital malformations
-
Fetal intrauterine growth retardation (IUGR)
-
Fetal anemia and Rh isoimmunization
-
Abnormal fetal presentation
-
Low birth weight (< 2500 g) [14]
-
Neonatal respiratory distress syndrome [14]
-
Jaundice [14]
-
Admission to the neonatal intensive care unit (NICU) [14]
-
Longer hospital stay [14]
-
Increased risk for infant neurodevelopmental delay and sudden infant death syndrome (SIDS) [15]
-
Neonatal mortality rate: As high as 1.2% in the United States [16]
Patient Education
Patients with placenta previa should decrease activity to avoid rebleeding. In addition, pelvic examinations and intercourse should be avoided.
Counsel patients with placenta previa about the risk of recurrence. Instruct them to notify the obstetrician caring for their next pregnancy about their history of placenta previa.
Encourage patients with known placenta previa to maintain intake of iron and folate as a safety margin in the event of bleeding.
-
Placenta previa.
-
Complete or total placenta previa. The entire cervical os is covered.
-
Low-lying placenta previa. The placenta partially separated from the lower uterine segment.
-
Placenta previa invading the lower uterine segment and covering the cervical os.
-
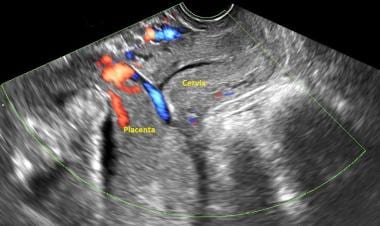
Complete placenta previa noted on ultrasound.
-
Another ultrasound image clearly depicting complete placenta previa.