Practice Essentials
In phimosis, the prepuce (foreskin) is too tight to be retracted to reveal the glans penis. Often, nonretractable foreskin is the presenting complaint of a patient or the parent/guardian. [1] Physiologic phimosis occurs naturally in newborn males. Pathologic phimosis defines an inability to retract the foreskin after it was previously retractable or after puberty, usually secondary to distal scarring of the foreskin. Paraphimosis is the entrapment of a retracted foreskin behind the coronal sulcus and is a disease of uncircumcised or partially circumcised males. [2, 3, 4, 5]
Physiologic phimosis results from adhesions between the epithelial layers of the inner prepuce and glans. These adhesions spontaneously dissolve with intermittent foreskin retraction and erections, so that as males grow, physiologic phimosis resolves with age. Physiologic phimosis occurs as separation that begins proximally through the process of desquamation forming small spaces that eventually coalesce to form the preputial sac. Treatment of patients with physiologic phimosis is not indicated; reassurance and an explanation of the natural history of healthy nonretractable foreskin should be given to concerned parents. [1]
Pathologic phimosis may be detected in males who report painful erections, hematuria, recurrent urinary tract infections, preputial pain, or a weakened urinary stream.
Paraphimosis is a urologic emergency that occurs in uncircumcised males when the foreskin becomes trapped behind the corona of the glans penis, leading to strangulation of the glans and to painful vascular compromise, distal venous engorgement, edema, and even necrosis. Typical symptoms include erythema, pain, and swelling of the foreskin and glans due to the constricting ring of the phimotic foreskin. This is sometimes described by patients as "penile swelling" and may be relatively painless. [6]
Poor hygiene and recurrent episodes of balanitis or balanoposthitis lead to scarring of preputial orifices, leading to pathologic phimosis. Stenosis scarring can be caused by balanitis xerotica obliterans (BXO), a chronic skin condition histologically identical to lichen sclerosis. BXO is an indication for circumcision at all ages. [7]
Forceful retraction of the foreskin leads to microtears at the preputial orifice that also leads to scarring and phimosis. Elderly persons are at risk of phimosis secondary to loss of skin elasticity and infrequent erections.
Patients with phimosis, both physiologic and pathologic, are at risk for developing paraphimosis when the foreskin is forcibly retracted past the glans and/or the patient or caretaker forgets to replace the foreskin after retraction. The most common cause of paraphimosis is a failure to retract the prepuce after the placement of a Foley catheter. Penile piercings increase the risk of developing paraphimosis if pain and swelling prevent reduction of a retracted foreskin.
With time, impairment of venous and lymphatic flow to the glans leads to venous engorgement and worsening swelling. As the swelling progresses, arterial supply is compromised, leading to penile infarction/necrosis, gangrene, and, eventually, autoamputation.
Diagnosis and treatment
Laboratory tests and radiography are not typically required in the assessment of phimosis, and studies have provided no evidence of obstruction from physiologic phimosis. When pathologic phimosis is treated with surgery, any surgically excised skin should be sent for histology to confirm the diagnosis and exclude evidence of malignancy. [1]
Paraphimosis is a urologic emergency that requires prompt diagnosis to avoid potential morbidity.
Circumcision is the preferred treatment for pathologic phimosis and represents the only absolute indication for this procedure in children. An alternative surgical approach is preputioplasty, which allows preservation of the foreskin. Initially, postoperative appearances are similar to those following a dorsal slit procedure, but regular retraction of the foreskin following the procedure allows resolution to a normal retractile prepuce. [1]
In a prospective study, by Zhou et al, of children with severe phimosis, 0.1% mometasone furoate was found to be effective, with recurrence being related to grade or symptoms of severe phimosis. [8]
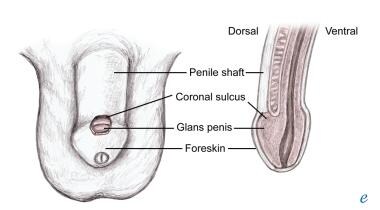
(See the image below.)
The uncircumcised male penis comprises the penile shaft, the glans penis, the coronal sulcus, and the foreskin/prepuce, as shown below.
There are many techniques of paraphimosis reduction, including manual reduction and the osmotic method, puncture method, and hyaluronidase method. Mild, uncomplicated paraphimosis may be reduced manually, usually without the need for sedation or analgesia. More difficult or complicated cases may require local anesthesia with a dorsal penile block, systemic analgesia, or procedural sedation. [6] The main goal of each method is to reduce the foreskin to its naturally occurring position over the glans penis by manipulating the edematous glans and/or the distal prepuce. Sterile technique should be used for all invasive procedures. [9, 10, 11, 12, 13, 14, 15, 16, 17, 18, 19]
Epidemiology
Up to 10% of males will have physiologic phimosis at 3 years of age, and a larger percentage of children will have only partially retractible foreskins. One to five percent of males will have nonretractible foreskins by age 16 years. [2, 5]
Research shows that in all but a small proportion of boys, the foreskin is retractile by the time boys mature through their teenage years. Studies have revealed that phimosis is present in 8% of 6- to 7-year-olds, 6% of 10- to 11-year-olds, and 1% of 16- to 17-year-olds. In contrast, preputial adhesions remain much more common throughout childhood and adolescence, but by 17 years of age, only 3% of these boys have persisting adhesions. [1]
True pathologic phimosis caused by BXO has a relatively stable incidence across all decades of life, with a spike in the third decade of life. It is relatively rare in children under the age of 5, and peak childhood incidence has been noted between 9 and 11 years of age. [1]
In uncircumcised children 4 months to 12 years of age with foreskin problems, paraphimosis (0.2%) is less common than other penile disorders, such as balanitis (5.9%), irritation (3.6%), penile adhesions (1.5%), or phimosis (2.6%). In adults, paraphimosis is most commonly found during adolescence. It occurs in about 1% of all adult males older than 16 years. [6]
In a Danish study, phimosis was the most frequently reported indication (95.0%) for foreskin surgery in boys younger than 18 years. The remaining 5% underwent surgery because of frenulum breve causing problems during erection. Nine patients needed a second surgery because of recurrent phimosis. [3]
A study of adult patients who underwent circumcision found that the most common indications were phimosis (46.5%), dyspareunia (17.8%), balanitis (14.4%), and concurrent phimosis and balanitis (8.9%). In most older patnts, the reason for adult circumcision was concurrent phimosis and balanitis or cancer, whereas in younger patients, dyspareunia was the most common cause. The complication rate was 3.5%, and there was no significant difference in complication rates between the older patient group and the younger patient group. [20]
Prognosis
Early selection of appropriate treatment for children with phimosis is beneficial for the development of their reproductive organs and significantly improves their prognosis. [21]
The use of steroid cream for physiologic phimosis is associated with decreased risk of recurrent urinary tract infection (UTI) in uncircumcised male infants with normal findings on renal ultrasound. [22]
Circumcision has traditionally been the treatment of choice, but its popularity in cases of non-scarred phimosis has been superseded by more conservative methods such as preputioplasty. Foreskin-conserving methods such as this are a valid option in the treatment of non-scarred pathologic phimosis. [23]
The prognosis with paraphimosis is excellent if it is diagnosed and treated promptly. An alternative to circumcision, especially in an older or sicker patient, is a dorsal slit. Either technique is satisfactory in preventing recurrence of paraphimosis. [6]
Patients with paraphimosis should receive instruction on hygiene, should be sure to return their foreskin to its normal position if it has been retracted, and should avoid wearing penile jewelry if this has contributed to the condition. The patient may wish to consider circumcision to preclude future episodes, particularly with recurrence. [6]
Patient Education
Parents should be educated about the normalcy of congenital phimosis and the time course of its resolution. The dangers of forcibly retracting the foreskin for hygienic purposes should be stressed. If the prepuce does not readily retract, parents should not attempt to clean under it.
Patients and parents of children should be educated on the importance of reduction of the foreskin after each cleaning.
All providers of adult care should be made aware of the risk of paraphimosis associated with bladder catheterization. They should be reminded to always reduce the foreskin after cleaning and catheterization.
-
Anatomy of the penis.
-
Physiologic phimosis versus pathologic phimosis.
-
Paraphimosis.
-
Dorsal slit procedure.