Practice Essentials
Non–small cell lung cancer (NSCLC) accounts for approximately 85% of all lung cancers. Histologically, NSCLC is divided into adenocarcinoma, squamous cell carcinoma (SCC) (see the image below), and large cell carcinoma. [1] Patients with NSCLC require a complete staging workup to evaluate the extent of disease, because stage plays a major role in determining the choice of treatment.
Go to Small Cell Lung Cancer for complete information on this topic. Go to Oncology Decision Point for expert commentary on NSCLC treatment decisions and related guidelines.
Signs and symptoms
NSCLC is often insidious, producing no symptoms until the disease is well advanced. Early recognition of symptoms may be beneficial to outcome.
At initial diagnosis, 20% of patients have localized disease, 25% of patients have regional metastasis, and 55% of patients have distant spread of disease. Symptoms depend on the location of cancer. [2]
The most common signs and symptoms of lung cancer include the following:
-
Cough
-
Chest pain
-
Shortness of breath
-
Coughing up blood
-
Wheezing
-
Hoarseness
-
Recurring infections such as bronchitis and pneumonia
-
Weight loss and loss of appetite
-
Fatigue
Metastatic signs and symptoms may include the following:
-
Bone pain
-
Spinal cord impingement
-
Neurologic problems such as headache, weakness or numbness of limbs, dizziness, and seizures
See Presentation for more detail.
Diagnosis
Testing
After physical examination and CBC, chest x-ray is often the first test performed. Chest radiographs may show the following:
-
Pulmonary nodule, mass, or infiltrate
-
Mediastinal widening
-
Atelectasis
-
Hilar enlargement
-
Pleural effusion
There are several methods of confirming diagnosis, with the choice determined partly by lesion location. These methods include the following:
-
Bronchoscopy
-
Sputum cytology
-
Mediastinoscopy
-
Thoracentesis
-
Thoracoscopy
-
Transthoracic needle biopsy (CT- or fluoroscopy-guided)
Staging
The TNM (tumor-node-metastasis) staging system from the American Joint Committee for Cancer Staging and End Results Reporting is used for NSCLC. The standard staging workup for NSCLC includes the following:
-
CT scan of chest and upper abdomen
-
Complete blood cell count with differential
-
Serum chemistry studies, including creatinine, electrolytes, and calcium
-
Alkaline phosphatase
-
Aspartate aminotransferase
-
Pulmonary function testing (if surgical resection is being considered)
-
Mediastinoscopy (if surgical resection is being considered)
See Workup for more detail. See also Lung Cancer Staging -- Radiologic Options, a Critical Images slideshow, to help identify stages of the disease process.
Management
Surgery, systemic therapy, and radiation are the main treatment options for NSCLC. Because most lung cancers cannot be cured with currently available therapeutic modalities, the appropriate application of skilled palliative care is an important part of the treatment of patients with NSCLC.
Surgery
Surgery is the treatment of choice for stage I and stage II NSCLC. Several different types of surgery can be used, as follows:
-
Lobectomy – removing a section of the lung
-
Pneumonectomy – removing the entire lung
-
Wedge resection – removing part of a lobe
Systemic therapy
Approximately 80% of all patients with lung cancer are considered for systemic therapy at some point during the course of their illness. Multiple randomized, controlled trials and large meta-analyses all confirm the superiority of combination chemotherapy regimens up front for advanced NSCLC.
The American Society for Clinical Oncology (ASCO) guidelines recommend that first-line treatment for NSCLC include a platinum combination. In younger patients, with a good performance status or in the adjuvant setting, cisplatin is preferred, but in older patients or those with significant comorbidities, carboplatin may be substituted.
Use of agents targeted to specific molecular features of the tumor has become standard practice. Depending on the molecular features, recommended systemic therapy regimens may include combinations of targeted agents with chemotherapy, or targeted agents alone.
Radiation
In the treatment of stage I and stage II NSCLC, radiation therapy alone is considered only when surgical resection is not possible. [3] Stereotactic radiation is a reasonable option for lung cancer treatment among those who are not candidates for surgery. [4] Beta blockers have been found to improve overall survival, disease-free survival, and distant metastasis–free survival, though not locoregional progession–free survival, in patients with NSCLC undergoing radiotherapy. [5]
See Treatment for more detail.
Background
Lung cancers are generally divided into two main categories: small cell lung cancer (SCLC) and non–small cell lung cancer (NSCLC). NSCLC accounts for approximately 85% of all lung cancers. Histologically, NSCLC is divided further into adenocarcinoma, squamous cell carcinoma (SCC), and large cell carcinoma. (See Pathophysiology.)
Lung cancer was a rare entity in the early 1900s but has since become far more prevalent. The prevalence of lung cancer is second only to that of prostate cancer in men and breast cancer in women. By the end of the 1900s, lung cancer had become the leading cause of preventable death in the United States, [6] and subsequently it surpassed heart disease as the leading cause of smoking-related mortality.
Lung cancer is the leading cause of cancer-related mortality in both men and women not only in the United States but also throughout the world. In 2024, the disease is expected to cause over 125,000 deaths in the United States—almost as much as colorectal, breast, and prostate cancers combined. [7] The types of lung cancer in the United States, as well as in many other countries, have also changed in the past few decades: the frequency of adenocarcinoma has risen, and that of SCC has declined. (See Epidemiology.)
Most lung carcinomas are diagnosed at an advanced stage, conferring a poor prognosis. The need to diagnose lung cancer at an early and potentially curable stage is thus obvious (see Prognosis), and this has inspired the adoption of lung cancer screening in patients at high risk for lung cancer (see Workup/Screening). In addition, most patients who develop lung cancer have been smokers and have smoking-related damage to the heart and lungs, making aggressive surgical or multimodality therapies less viable options.
Lung cancer is often insidious, producing no symptoms until the disease is well advanced. In approximately 7-10% of cases, lung cancers are diagnosed incidentally in asymptomatic patients, when a chest radiograph performed for other reasons reveals the disease. Numerous pulmonary signs may be associated with NSCLC. Systemic findings may include unexplained weight loss and low-grade fever. (See Presentation.)
Because of the importance of stage in the therapeutic decision-making process, all patients with NSCLC must be staged adequately. A complete staging workup for NSCLC should be carried out to evaluate the extent of disease. (See Workup.)
Treatment primarily involves surgery, chemotherapy, or radiation therapy. Because most lung cancers cannot be cured with currently available therapeutic modalities, the appropriate application of skilled palliative care is an important part of the treatment of patients with NSCLC. (See Treatment.)
Go to Small Cell Lung Cancer for complete information on this topic.
Pathophysiology
Both exposure (environmental or occupational) to particular agents and an individual’s susceptibility to these agents are thought to contribute to the risk of developing lung cancer. In the United States, active smoking is responsible for approximately 90% of lung cancer cases. Occupational exposures to carcinogens account for approximately 9-15% of lung cancer cases.
Exposure to carcinogens
Tobacco smoke contains more than 300 harmful substances with at least 40 known potent carcinogens. Polyaromatic hydrocarbons and nicotine-derived nitrosamine ketone (NNK) are known to cause DNA damage by forming DNA adducts in animal models. Benzo-A-pyrine also appears to induce molecular signaling such as AKT, as well as inducing mutations in p53 and other tumor suppressor genes.
The most common occupational risk factor for lung cancer is exposure to asbestos. Studies have shown radon exposure to be associated with 10% of lung cancer cases, while outdoor air pollution accounts for perhaps 1-2%. [8] In addition, preexisting nonmalignant lung diseases, such as chronic obstructive pulmonary disease, idiopathic pulmonary fibrosis, and tuberculosis have all been shown to be associated with increased lung cancer rates.
The current multiple hit theory suggests that a series of toxic cellular insults disrupts orderly genetic reproduction. Symptoms ultimately develop from the uncontrolled disorganized growth that interferes with local or distant anatomy or physiologic processes. [8]
A study by Ito et al assessed the shift in histologic types of lung cancer in Japan and the United States in relation to the shift from nonfiltered to filtered cigarettes. [9] The study determined that the shift in cigarette types only altered the most frequent type of lung cancer, which shifted from SCC to adenocarcinoma.
Genetic susceptibility
Advanced molecular techniques have identified amplification of oncogenes and inactivation of tumor suppressor genes in NSCLC. The most important abnormalities detected are mutations involving the ras family of oncogenes. The ras oncogene family has 3 members: H-ras, K-ras, and N-ras. These genes encode a protein on the inner surface of the cell membrane with guanosine triphosphatase activity and may be involved in signal transduction.
Studies performed on mice suggest the involvement of ras mutations in the molecular pathogenesis of NSCLC. Studies in humans suggest that ras activation contributes to tumor progression in persons with lung cancer. The ras gene mutations occur almost exclusively in adenocarcinoma and are found in 30% of such cases. These mutations were not identified in adenocarcinomas that developed in persons who do not smoke. The K-ras mutation appears to be an independent prognostic factor.
Studies are ongoing to develop management plans according to the presence or absence of ras gene mutations.
Other molecular abnormalities found in NSCLC include mutations in the oncogenes c-myc and c-raf and in the tumor suppressor genes retinoblastoma (Rb) and p53.
Two studies have documented early and extensive mutations in lung cancers that result in pronounced intratumor heterogeneity by the time these cancers manifest clinically—thus helping to explain why these cases so often fail to respond to treatment. A study by Zhang and colleagues identified 20 of 21 known cancer gene mutations in all regions of 11 localized lung adenocarcinomas. On follow-up, patients who had postsurgical relapse had significantly larger fractions of subclonal mutations in their primary tumors. [10]
Similarly, a study by de Bruin and colleagues in seven operable NSCLCs determined that there was a long period of tumor latency between early mutations and clinical symptoms, which appeared after new mutations triggered rapid disease growth. In some former smokers, the initial mutations dated back to when they were smoking cigarettes, two decades earlier. Over time, however, those mutations became less important, with more recent mutations resulting from a new process controlled by a protein called APOBEC. [11]
Classification of lung cancer
Lung cancers are generally divided into 2 main categories: SCLC and NSCLC. NSCLC accounts for approximately 85% of all lung cancers. NSCLC is divided further into adenocarcinoma, SCC, and large cell carcinoma. All share similar treatment approaches and prognoses but have distinct histologic and clinical characteristics.
Adenocarcinoma
Adenocarcinoma, arising from the bronchial mucosal glands, is the most common NSCLC cancer in the United States, representing 35-40% of all lung cancers. It is the subtype observed most commonly in persons who do not smoke. It usually occurs in a peripheral location within the lung, in some cases at the site of pre-existing scars, wounds, or inflammation (ie, a “scar carcinoma”).
Bronchoalveolar carcinoma is a distinct subtype of adenocarcinoma with a classic manifestation as an interstitial lung disease on chest radiograph. Bronchoalveolar carcinoma arises from type II pneumocytes and grows along alveolar septa. This subtype may manifest as a solitary peripheral nodule, multifocal disease, or a rapidly progressing pneumonic form. A characteristic finding in persons with advanced disease is voluminous watery sputum.
Squamous cell carcinoma
SCC accounts for 25-30% of all lung cancers. Whereas adenocarcinoma tumors are peripheral in origin, SCC is found in the central parts of the lung (see the image below). The classic manifestation is a cavitary lesion in a proximal bronchus. This type is characterized histologically by the presence of keratin pearls and can be detected with cytologic studies because it has a tendency to exfoliate. It is the type most often associated with hypercalcemia.
View Media Gallery
Large-cell carcinoma
Large-cell carcinoma accounts for 10-15% of lung cancers, typically manifesting as a large peripheral mass on chest radiograph. Histologically, this type has sheets of highly atypical cells with focal necrosis, with no evidence of keratinization (as is typical of SCC) or gland formation (as is typical of adenocarcinomas).
With improved histopathologic procedures and the use of electron microscopy, most NSCLCs that would previously have been classified as large-cell carcinomas are identified as undifferentiated adenocarcinomas or, less frequently, as SCCs. [12] Large-cell undifferentiated cancers carry the same prognosis as do adenocarcinomas and are combined with them in clinical trials.
Etiology
Causes of lung cancer include the following:
-
Smoking (78% in men, 90% in women)
-
Radon exposure
-
Asbestos exposure
-
Halogen ether exposure
-
Chronic interstitial pneumonitis
-
Inorganic arsenic exposure
-
Radioisotope exposure, ionizing radiation
-
Atmospheric pollution
-
Chromium, nickel exposure
-
Vinyl chloride exposure
Unlike many other malignancies, whose causes are largely unknown, lung cancer is known to be caused by tobacco smoking in as many as 90% of patients. However, NSCLC rates have been rising in persons who have never smoked: In a United States study, rates increased from 8.0% in 1990–1995 to 14.9% in 2011–2013. [13] Globally, from 10% to 25% of lung cancer occur in never-smokers. [14]
Because only about 15% of smokers develop lung cancer and not all lung cancer patients have a history of smoking, other factors play a causative role, either independently or in conjunction with smoking. In addition to genetic susceptibility, major contributors in never-smokers include second-hand smoke, occupational carcinogen exposure, outdoor pollution, x-ray radiation, and radon exposure. [14] (See Pathophysiology.) Genetic factors probably contribute in all populations, but the contribution of other factors is population-specific.
A study by Bagnardi et al determined that alcohol use is not an independent factor in the etiology of lung cancer. [15]
Smoking
Smoking prevalence in the United States has gradually declined over last 4 decades. In 2021, there were an estimated 28.3 million active adult smokers in the United States. Overall smoking prevalence declined from 20.9% in 2005 to 11.5% in 2021. [16]
Worldwide, there were an estimated 1.14 billion current smokers in 2019. Although the prevalence of smoking in persons aged 15 years and older decreased significantly from 1990 to 2019 (by 27.5% in males and by 37.7% in females), population growth led to a significant increase in the total number of smokers, from 0.99 billion in 1990. [17]
The development of lung cancer is directly related to number of cigarettes smoked, length of smoking history, and the tar and nicotine content of the cigarettes. Risk is highest among current smokers and lowest among nonsmokers. A large trial showed that persistent smokers had a 16-fold elevated lung cancer risk, which was further doubled in those who started smoking when younger than 16 years. [18] The age-adjusted incidence rates range from 4.8-20.8 per 100,000 among nonsmokers to 140-362 per 100,000 among active smokers.
Although tobacco smoking is the major cause of lung cancer, it is now believed that males and females may differ in their susceptibility to the carcinogenic effects of tobacco smoke. This difference may be due to differences in DNA repair mechanisms. Although still considered controversial, it is well known that women are more likely to develop adenocarcinomas and that, stage for stage, women survive longer. In addition, differences in response to certain biologic therapies (eg, epidermal growth factor receptor [EGFR] inhibitors) and antiangiogenic agents have been observed between sexes.
The risk of lung cancer declines slowly after smoking cessation. Long-term follow-up studies show that the relative risk remains high in the first 10 years after cessation and gradually declines to 2-fold approximately 30 years after cessation. This long-term risk explains the development of almost 50% of United States lung cancer cases in past smokers.
Strong cardiorespiratory fitness might help reduce lung cancer risk in men who smoke or used to smoke, accordng to the findings from a study that assessed 1602 former smokers (40 pack-years) and 1377 current smokers (43 pack-years). All were men, aged 42 to 76 years, who were free from lung cancer at baseline. Over a follow-up period of 4.6 to 18.6 years, 46 former smokers and 53 current smokers developed lung cancer. Of this group, 40 former smokers and 39 current smokers died. Men who had higher fitness levels at baseline, measured with a maximal treadmill exercise test, had a lower incidence of lung cancer during follow-up and had better survival if they did get lung cancer. [19]
Secondhand smoking
Cigarette smoke containing the carcinogenic N-nitrosamines and aromatic polycyclic hydrocarbons can be inhaled passively by nonsmokers (secondhand smoke); urinary levels of these carcinogens in nonsmokers are 1-5% of those found in active smokers. As many as 25% of the lung cancers in persons who do not smoke are believed to be caused by secondhand smoke. [20]
The US Environmental Protection Agency has recognized passive smoking as a potential carcinogen. About 3000 cases of lung cancer appear to be related to passive exposure. This awareness has led to local ordinances restricting smoking in enclosed public places, including restaurants and government buildings.
Lung cancer in never-smokers
A minority of lung cancers develop in persons who have never smoked. These lung cancers are genetically distinct from smoking-related NSCLC, and this distinction may have therapeutic implications. The observed genetic differences include a lower frequency of K-ras and a higher frequency of mutations in the EGF receptor and likely are responsible for the higher efficacy of EGF receptor inhibitors in this patient population.
Asbestos exposure
The silicate type of asbestos fiber is an important carcinogen. Asbestos exposure has been shown to be strongly associated with the causation of lung cancer, malignant pleural mesothelioma, and pulmonary fibrosis. Asbestos exposure increases the risk of developing lung cancer by as much as 5 times.
Tobacco smoke and asbestos exposure act synergistically, and the risk of developing lung cancer for persons who currently smoke tobacco and have a history of asbestos exposure approaches 80-90 times that of control populations.
Radon exposure
Radon is an inert gas produced as a result of uranium decay. Radon exposure is a well-established risk factor for lung cancer in uranium miners. Approximately 2-3% of lung cancers annually are estimated to be caused by radon exposure. Household exposure to radon, however, has never been clearly shown to cause lung cancer.
The US National Research Council’s report of the Sixth Committee on Biological Effects of Ionizing Radiation has estimated that radon exposure causes 2100 new lung cancers each year, while it contributes to lung cancer causation in approximately 9100 persons who smoke.
HIV infection
Persons with HIV infection have a higher lung cancer risk than those without HIV infection, with relative risk estimates ranging from 2 to 11. In persons with HIV infection, lung cancer is the most common and most fatal non-AIDS-associated malignancy, accounting for about 16% of deaths. [21] A majority of these cases are adenocarcinomas. In most, but not all, studies the incidence and risk of lung cancer in HIV-infected persons did not change significantly with the advent of highly active antiretroviral therapy. [22]
Lung cancer in HIV-infected persons develops almost exclusively in smokers, but HIV infection appears to increase lung cancer risk independent of smoking status, by a factor of at least 2.5-fold. Compared with lung cancer patients in the general population, HIV-infected patients with lung cancer are significantly younger. Most patients with HIV infection and lung cancer present with advanced-stage disease and have significantly shorter median survival. [21]
Other environmental agents
Beryllium, nickel, copper, chromium, and cadmium have all been implicated in causing lung cancer.
Dietary fiber and vegetables have been suggested as protective from lung cancer. Although diets rich in fruits and vegetables appear to be associated with lower rates of lung cancer, trials of supplemental beta-carotene, alone or in combination with vitamin E or retinyl palmitate, in persons at high risk for lung cancer found that this supplementation actually increased the incidence of lung cancers. [23]
Epidemiology
United States statistics
In the United States, lung cancer is the second most common cancer, after prostate cancer in men and breast cancer in women, but the most common cause of cancer deaths. The American Cancer Society projects that 234,580 cancers of the lung and bronchus will be diagnosed in the United States in 2024, with 125,070 deaths. Approximately 80% of those cases are expected to be NSCLC. [7]
Incidence rates of lung cancer follow those of tobacco smoking, with a lag of several decades. Since the mid-2000s, the incidence rate of lung cancer has decreased 2.5% per year in men and 1% per year in women. Because women took up cigarette smoking in large numbers later and were slower to quit, declines began later and have been slower in women than in men. This has resulted in a narrowing of the sex gap in lung cancer incidence, from more than 3-fold higher rates in men in the 1970s to just 24% higher in 2018. [24]
Lung cancer death rates for US women are among the highest in the world. Although in the United States, death rates are higher in men than in women, rates for US men are still lower than rates for men in several other countries. [25] These trends in US death rates parallel trends in smoking prevalence over the past 50 years. [24]
However, lung cancer death rates in the US have been decreasing at an accelerated rate. In men, lung cancer death rates fell 3% per year during 2005-2014 and 5% per year during 2014-2020; in women, the decreases during those periods were 2% and 4% per year, respectively. This reduction outpaces declines in incidence and likely reflects advances in treatment, as well as earlier detection, facilitated by lung cancer screening, which has been recommended for persons at high risk for lung cancer since 2013. [24]
International statistics
Lung cancer is the second most commonly diagnosed cancer worldwide, after breast cancer, and its incidence continues to grow. In 2022, an estimated 2.5 million new cases of lung cancer were diagnosed globally, accounting for approximately 12.4% of the global cancer burden. An estimated 1.8 million lung cancer deaths occurred in 2022. [26] Among all cancers, lung cancer is currently the most common cause of cancer deaths in most countries, with industrialized regions such as Eastern Asia, North America, and Europe having the highest rates.
Several differences exist in lung cancer incidence according to geographic area. The highest incidence occurs in Eastern Asia (39.4 cases per 100,000 population per year). The lowest incidence rate is in western Africa (approximately 2.1 cases per 100,000 population per year). [26] With increased smoking in developing countries, the incidence is expected to increase in the next few years, notably in China and India.
Generally, global lung cancer trends have followed the trends in smoking, with a lag time of several decades. Lung cancer incidence has been declining in several countries, including the United States, Canada, the United Kingdom, and Australia, following the decreasing rate of smoking. Lung cancer incidence among women, however, continues to increase in several parts of the globe, although it has begun to plateau in the United States. Notably, despite a very low rate of smoking, Chinese women have a higher incidence of lung cancer than European women.
Age and sex distribution
Lung cancer occurs predominately in persons aged 50-70 years. The probability of developing lung cancer remains very low until age 39 years in both sexes. It then slowly starts to rise and peaks among those older than 70 years. The risk of developing lung cancer remains higher among men in all age groups after age 40 years.
Overall, lung cancer is more common in men than in women. In the United States, Northern Europe, and Western Europe, the prevalence of lung cancer has been decreasing in men. In Eastern and Southern European countries, the incidence of lung cancer has been rapidly increasing. Most Western countries have encountered a disturbing trend of increasing prevalence in women and younger patients. Women have a higher incidence of localized disease at presentation and of adenocarcinoma and typically are younger when they present with symptoms.
Over the past two decades, the incidence of lung cancer has generally decreased in both men and women 30 to 54 years of age in all races and ethnic groups. However, the incidence has declined more steeply in men. As a result, lung cancer rates in younger women have become higher than those in younger men. In non-Hispanic whites and Hispanics ages 44 to 49 years, for example, the female-to-male rate ratio for lung cancer incidence rose from 0.88 during 1995-1999 to 1.17 during 2010-2014. [27]
This reversal can be explained in part by increased rates of cigarette smoking in women born since 1965. However, while the difference in smoking rates in that age group has narrowed, rates in women have generally not exceeded the rates in men, so other factors may be playing a role. For example, women may be more susceptible to the oncogenic effects of smoking. [27]
Incidence and survival by race
Whereas lung cancer incidence rates are similar among Black and White women, lung cancer occurrence is approximately 45% higher in Black men than in White men. [25] This increased incidence has been attributed to differences in smoking habits; however, recent evidence suggests a slight difference in susceptibility.
From 1995-2001, the 5-year relative survival rate was 13% lower in Blacks than in Whites. [25] This racial gap persisted within each stage at diagnosis for both men and women.
Trends in 5-year survival rates in lung cancer from 1975-2003 revealed that while modest gains occurred in 5-year survival rates among Whites, survival rates remained unchanged in the Black population. Current 5-year survival rates are estimated to be 16% among Whites and 13% among non-Whites.
Prognosis
Lung cancer is highly lethal. In the European Union, the 5-year overall survival rate in 2010-14 was 15% on average, ranging from 10% or less to 20% in different countries. [25] The highest recorded 5-year patient survival rates are observed in the United States. US data collected from 2013–2019 indicate that the 5-year relative survival rate for lung cancer was 25.4%, reflecting a steady but slow improvement from 11.7% in 1975. [28] However, the 5-year relative survival rate varies markedly, depending on how advanced the disease is at diagnosis, as follows [28] :
-
61.8% for localized disease
-
34.8% for regional disease
-
8.2% for distant-metastasis disease
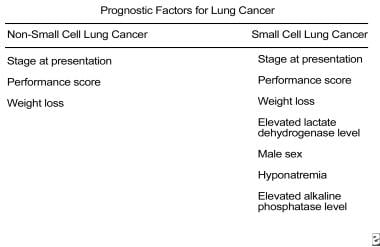
Prognostic factors for NSCLC are summarized in the image below.
A retrospective Surveillance, Epidemiology, and End Results (SEER) data analysis suggests that the number of lymph nodes with cancer may be predictive of survival. Mean lung cancer-specific survival decreased from 8.8 years for patients with one positive lymph node to 3.9 years for patients with more than eight positive lymph nodes. [29]
Patients with in situ and stage I lung cancer may respond to surgery. Their prognosis is far better than that of patients with more advanced disease. In patients with radiologically occult lung neoplasms, the 5-year survival rate is 24-26%; in those with abnormal chest radiographic findings, the rate is 12%. If the cancer is nonresectable, the prognosis is poor, with a mean survival rate of 8-14 months.
Mostertz et al found that in some patient populations, the oncogenic pathway activation profile of the tumor can have prognostic significance. [30] Retrospective analysis of 787 patients with predominantly early-stage NSCLC, using gene expression profiling, showed the following:
-
In patients younger than 70 years, high-risk patients, with the shortest recurrence-free survival, demonstrated increased activation of the Src and tumor necrosis factor (TNF) pathways.
-
In women, high-risk patients demonstrated increased activation of the invasiveness and signal transducer and activator of transcription 3 (STAT3) pathways.
-
Multivariate analyses confirmed the independent clinical relevance of the pathway-based subphenotypes in women and patients younger than 70 years.
A meta-analysis by Parsons et al suggests that smoking cessation after diagnosis of early-stage lung cancer may improve prognosis, probably by reducing cancer progression. Life table modelling on the basis of data from 9 studies gave an estimated 5-year survival rate of 33% in 65-year-old patients with early-stage NSCLC who continued to smoke compared with 70% in those who quit smoking. [31]
In an analysis of data on 4200 patients who participated in the National Comprehensive Cancer Network's NSCLC Database Project, patients who were current smokers at the time of diagnosis had worse survival compared with patients who never smoked, and among younger patients with stage IV disease, current smokers had worse survival compared with former smokers who quit smoking more than 12 months before being diagnosed. [32]
Secondary analyses of the Women’s Health Initiative (WHI) randomized, placebo-controlled trial demonstrated an association between the use of daily conjugated equine estrogen (CEE, 0.625 mg) plus medroxyprogesterone acetate (MPA, 2.5 mg) and NSCLC. Women who used CEE plus MPA for more than 5 years were at increased risk for NSCLC, and women using CEE plus MPA who were diagnosed with NSCLC had higher mortality than women with NSCLC who do not take hormone therapy. [33]
The WHI analyses included 16,608 multiethnic postmenopausal women aged 50-79 years. Confirmation of lung cancers was completed by medical record review. This area deserves more attention and study to determine the risks and benefits of hormone therapy for postmenopausal women who smoke.
In contrast, a study by Bouchardy et al found that patients who had received antiestrogen treatment for breast cancer had a lower lung cancer mortality rate. However, use of antiestrogens did not significantly lower standardized incidence ratios for lung cancer. [34]
A review of eight trials by Rothwell et al found that allocation to daily aspirin reduced death caused by a variety of cancers, including adenocarcinoma of the lung (but no other form of lung cancer). A latent period of 5 years was observed before risk of death was decreased for lung cancer, but 20-year risk of cancer death remained lower in the aspirin groups. Benefit was unrelated to aspirin dose (75 mg or higher), sex, or smoking, but increased with age, with the absolute reduction in 20-year risk of cancer death reaching 7.08% at age 65 years and older. [35]
Although tumor-node-metastasis (TNM) staging is the best prognostic factor for NSCLC, a study by Hofman et al concluded that preoperative detection of circulating tumor cells (CTCs) has prognostic significance. [36] The results showed that the presence and level of 50 or more circulating nonhematologic cells (CNHC) were associated with worse survival among patients with resectable NSCLC. Although CTCs are potentially interesting, the significance of their presence is still being debated. [37]
Risk of recurrence
In a 2012 retrospective review of 1402 consecutive stage I-III (N0-N1) NSCLC patients who underwent complete resection without adjuvant radiation therapy, significant risk factors for local recurrence included surgical procedure (single/multiple wedges + segmentectomy versus lobectomy + bilobectomy + pneumonectomy), visceral pleural invasion, and tumor size > 2.7 cm. Significant risk factors for regional recurrence included pathologic N1 stage, lymphovascular space invasion, and visceral pleural invasion. [38]
In a study of 452 cases of stage I lung adenocarcinoma, thyroid transcription factor–1 (TTF-1) expression independently predicted the risk of disease recurrence. The 5-year cumulative incidence of recurrence was 40% for patients with negative TTF-1 expression, versus 15% for those with positive TTF-1 expression (P < 0.001. [39]
According to a 2013 retrospective analysis of 734 patients with stage I adenocarcinoma no larger than 2 cm, recurrence of small, early-stage adenocarcinoma after limited lung resection is three times more likely when the micropapillary component of the tumor is 5% or greater. In the 258 study patients who underwent wedge resection or segmentectomy, after adjustment for both vascular and lymphatic invasion, the presence of a micropapillary component of 5% or greater was independently associated with a 5-year cumulative incidence of recurrence (hazard ratio = 3.11). Micropapillary status was not significantly associated with recurrence in the 476 patients who underwent lobectomy. [40]
Patient Education
Advise patients that smoking cessation is the most important measure for preventing lung cancer; it may also improve prognosis in patients with early-stage lung cancer. [31] Smoking cessation by others who share the patient’s home, car, or both is also important. According to published data, the use of nicotine alternatives (eg, gum, patch, spray) instead of cigarettes reduces the incidence of lung cancer, although it does not affect the incidence of ischemic heart disease.
Advise the patient to avoid asbestos exposure. Consider prophylactic administration of retinoids, such as beta-carotene.
Where appropriate, patient education should include a discussion of lung cancer screening. Current American Cancer Society guidelines recommend annual lung cancer screening with a low-dose computed tomography (LDCT) scan for asymptomatic individuals at higher risk for lung cancer who meet all of the following conditions [41] :
-
Aged 50 to 80 years and in fairly good health
-
Currently smoke or previously smoked
-
Have at least a 20-pack-year smoking history
In addition, individuals who are going to be screened should:
-
Receive smoking cessation counseling if they are current smokers
-
Have been involved in informed/shared decision making about the benefits, limitations, and harms of screening with LDCT scans,
-
Have access to a high-volume, high-quality lung cancer screening and treatment center
See also Workup/Screening. For patient education information, see Lung Cancer.
-
Non–small cell lung cancer. Symptoms and signs of lung cancer.
-
Non–small cell lung cancer. Diagnostic approach for possible lung cancer.
-
Staging workup for non–small cell lung cancer.
-
Treatment recommendations and future research directions in the management of non–small cell lung cancer.
-
Non–small cell lung cancer. Performance status scales for patients with cancer.
-
Non–small cell lung cancer. Prognostic factors for lung cancer.
-
Non–small cell lung cancer. Bronchoscopy. A large central lesion was diagnosed as non–small cell carcinoma.
-
Non–small cell lung cancer. Left pleural effusion and volume loss secondary to non–small cell carcinoma of the left lower lobe. The pleural effusion was sampled and found to be malignant; therefore, the lesion is inoperable.
-
Non–small cell lung cancer. Left upper collapse is almost always secondary to endobronchial bronchogenic carcinoma.
-
Non–small cell lung cancer. Complete left lung collapse secondary to bronchogenic carcinoma of left mainstem bronchus.
-
Non–small cell lung cancer. A cavitating right lower lobe squamous cell carcinoma.
-
Non–small cell lung cancer. CT scan shows cavitation and air-fluid level.
-
Non–small cell lung cancer. Patient has right lower lobe opacity. This is not well circumscribed and was found to be a squamous cell carcinoma.
-
Lung cancer, small cell. Contrast-enhanced CT scan of the chest shows a large left lung and a hilar mass, with invasion of the left pulmonary artery.
-
Lung cancer, small cell. Coronal positron emission tomogram shows abnormal areas of increased metabolic activity in the left hilar and left adrenal regions consistent with a hilar tumor with left adrenal metastasis.
-
Lung cancer, small cell. Whole-body nuclear medicine bone scanning with anterior and posterior images reveal multiple abnormal areas of increased radiotracer activity in the pelvis, spine, ribs, and left scapula. These findings are consistent with bony metastatic disease. The bones are commonly affected in patients with small-cell lung cancer.
-
Lung squamous carcinoma 4x: low power magnification of moderately differentiated squamous cell carcinoma showing irregular nests of tumor cells with focal areas of keratinization (pink-orange areas).
-
Lung squamous carcinoma 20x: higher power magnification of moderately differentiated squamous cell carcinoma showing focal areas of keratinization (pink-orange areas) just to the right of center.
-
Lung adenocarcinoma 4x: low power magnification of moderately differentiated adenocarcinoma showing rounded nests of pale staining tumor cells with gland lumina within some of the clusters.
Tables
What would you like to print?
- Overview
- Presentation
- DDx
- Workup
- Approach Considerations
- Laboratory Studies
- Chest Radiography
- Computed Tomography
- Magnetic Resonance Imaging
- Bone Scintigraphy
- Positron Emission Tomography
- Sputum Cytologic Studies
- Bronchoscopy
- Biopsy
- Needle Thoracentesis (Ultrasound Guided)
- Thoracoscopy and Mediastinoscopy
- Molecular Testing
- Histologic Findings
- Staging
- Workup for Special Populations
- Screening
- Show All
- Treatment
- Guidelines
- Medication
- Medication Summary
- Antineoplastic Agents
- Antineoplastics, Anaplastic Lymphoma Kinase Inhibitors
- PD-1/PD-L1 Inhibitors
- Anti-CLTA4 Antibodies
- Antineoplastics, EGFR Inhibitors
- Antineoplastics, Anti-HER2
- Antineoplastics, BRAF Kinase Inhibitors
- Antineoplastics, Tyrosine Kinase Inhibitors
- RET Kinase Inhibitors
- MET Tyrosine Kinase Inhibitors
- Antineoplastics, KRAS Inhibitors
- Antineoplastics, Monoclonal Antibodies
- Antiemetic Agents
- Show All
- Questions & Answers
- Media Gallery
- Tables
- References