Practice Essentials
Brain tumors may originate from neural elements within the brain, or they may represent spread of distant cancers. Primary brain tumors arise from CNS tissue and account for roughly half of all cases of intracranial neoplasms. The remainder of brain neoplasms are caused by metastatic lesions.
In adults, two thirds of primary brain tumors arise from structures above the tentorium (supratentorial), whereas in children, two thirds of brain tumors arise from structures below the tentorium (infratentorial). Gliomas, metastases, meningiomas, pituitary adenomas, and acoustic neuromas account for 95% of all brain tumors. See the image below.
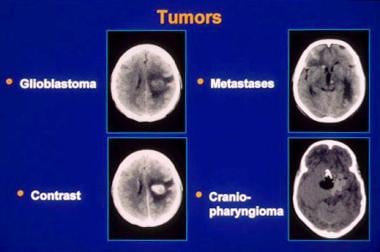 Brain neoplasms. CT images of several tumor types. Slide courtesy of UMASS Continuing Education Office.
Brain neoplasms. CT images of several tumor types. Slide courtesy of UMASS Continuing Education Office.
Signs and Symptoms
Presenting complaints of patients with an intracranial neoplasm tend to be similar for primary brain tumors and intracranial metastases. The onset of symptoms usually is insidious, but an acute episode may occur with bleeding into the tumor, or when an intraventricular tumor suddenly occludes the third ventricle.
Manifestations may be nonspecific and include the following:
-
Headache
-
Altered mental status
-
Ataxia
-
Nausea
-
Vomiting
-
Weakness
-
Gait disturbance
CNS neoplasms also may manifest as follows:
-
Focal seizures
-
Fixed visual changes
-
Speech deficits
-
Focal sensory abnormalities
Headache associated with intracranial neoplasms have the following characteristics:
-
Often is a late complaint
-
Usually not an isolated finding
-
The worst symptom in only one half of patients
-
In patients with established headache, may manifest as a change in the headache pattern
-
New onset of headaches in middle-aged or older patients is worrisome
-
The location of the headache reliably indicates the side of the head affected, but it does not indicate the precise site of the tumor
-
Headaches are more common with posterior fossa tumors
-
Headache is a more frequent symptom of intracranial tumor in pediatric patients
-
Nausea and/or vomitting (40%)
Although often described as characteristic of tumor headaches, the following clincial features are not commonly present [1] :
-
Pain that is worse in the early morning than at other times
-
Exacerbation with Valsalva maneuvers, bending over, or rising from a recumbent position
No physical finding or pattern of findings unmistakably identifies a patient with a CNS neoplasm. Based on their location, intracranial tumors may produce a focal or generalized deficit, but signs may be lacking (especially if the tumor is confined to the frontal lobe) or even falsely localizing. Findings may include the following:
-
Papilledema, which is more prevalent with pediatric brain tumors, reflects an increase in intracranial pressure (ICP) of several days or longer
-
Diplopia may result from displacement or compression of the sixth cranial nerve at the base of the brain
-
Impaired upward gaze, called Parinaud syndrome, may occur with pineal tumors
-
Tumors of the occipital lobe specifically may produce homonymous hemianopia or partial visual field deficits
-
Anosmia may occur with frontal lobe tumors
-
Brainstem and cerebellar tumors induce cranial nerve palsies, ataxia, incoordination, nystagmus, pyramidal signs, and sensory deficits on one or both sides of the body
See Presentation for more detail.
Diagnosis
With clinical suspicion of cancer, obtain routine laboratory studies on admission, including the following:
-
Complete blood cell count (CBC)
-
Coagulation studies
-
Electrolyte levels
-
Comprehensive metabolic panel
Obtain neuroimaging studies in patients with symptoms suggestive of an intracranial neoplasm, such as the following:
-
Acute mental status changes
-
New-onset seizures
-
Focal motor or sensory deficits, including gait disturbance
-
Suspicious headache
-
Signs of elevated ICP (eg, papilledema)
-
Generally, CT is the imaging modality of choice for the ED physician.
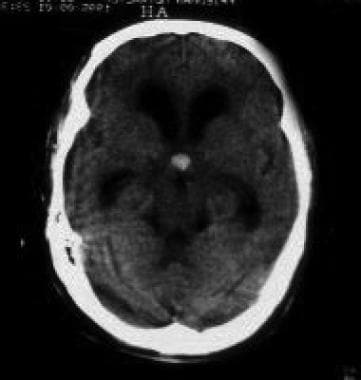
Although some tumors exhibit a characteristic appearance, do not make an unequivocal diagnosis based solely on radiologic findings. Generally, computed tomography (CT) is the imaging modality of choice for the emergency department physician. CT findings are as follows:
-
Most tumors demonstrate enhancement with contrast material administration
-
Tumors may appear hypodense, isodense, or hyperdense or have mixed density
-
Metastases to the brain tend to be multiple, but certain tumors (eg, renal cell carcinomas) tend to produce solitary metastatic brain lesions
As magnetic resonance imaging (MRI) becomes increasingly available, it may supplant CT as the imaging procedure of choice. Features of MRI for imaging intracranial neoplasms are as follows:
-
MRI is most helpful for identifying tumors in the posterior fossa (including acoustic neuromas) and hemorrhagic lesions
-
MRI is useful in patients with an allergy to iodinated contrast material or renal insufficiency
-
Drawbacks to MRI include incompatibility with certain medical equipment, longer imaging times (increased risk of motion artifact), and poor visualization of the subarachnoid space
-
Neither CT nor MRI can be used to differentiate tumor recurrence from radionecrosis
See Workup for more detail.
Management
Acute treatment for cerebral edema from intracranial neoplasms is as follows:
-
Corticosteroids may dramatically reduce signs and symptoms, bringing relief within a few hours
-
Dexamethasone is the agent of choice
-
Recommended doses generally range from 4-24 mg daily
Definitive treatment is as follows:
-
Generally, care of patients with a brain tumor is multidisciplinary, requiring assistance from a neurosurgeon, an oncologist, a radiologist, and an expert in radiation therapy
-
Management varies greatly depending on tumor location, tissue type, and comorbid conditions
-
Surgical treatment options may include tumor removal or debulking, installation of a ventricular shunt, and placement of radioactive implants
See Treatment and Medication for more detail.
For patient education resources, see Brain Cancer.
Pathophysiology
Tumors of the brain produce neurologic manifestations through a number of mechanisms. Small, critically located tumors may damage specific neural pathways traversing the brain. Tumors can invade, infiltrate, or supplant normal parenchymal tissue, disrupting normal function. Because the brain dwells in the limited volume of the cranial vault, growth of intracranial tumors with accompanying edema may cause increased intracranial pressure. Tumors adjacent to the third and fourth ventricles may impede the flow of cerebrospinal fluid, leading to obstructive hydrocephalus. In addition, tumors generate new blood vessels (ie, angiogenesis), disrupting the normal blood-brain barrier and promoting edema.
 Brain neoplasms. Colloid cyst of the third ventricle with obstructive hydrocephalus. Image courtesy of Peter Ferrera, MD.
Brain neoplasms. Colloid cyst of the third ventricle with obstructive hydrocephalus. Image courtesy of Peter Ferrera, MD.
The cumulative effects of tumor invasion, edema, and hydrocephalus may elevate the intracranial pressure (ICP) and impair cerebral perfusion. Intracranial compartmental rise in ICP may provoke shifting or herniation of tissue under the falx cerebri, through the tentorium cerebelli, or through the foramen magnum.
Slow-growing tumors, particularly tumors expanding in the so-called silent areas of the brain, such as the frontal lobe, may be associated with a more insidious clinical course. These tumors tend to be larger at detection.
Most primary brain tumors do not metastasize, but if they do metastasize, intracranial spread generally precedes distant dissemination.
Metastatic brain tumors from non-CNS primary tumors may be the first sign of malignancy, or they may herald a relapse. Nonetheless, the signs and symptoms of brain metastases simulate those of primary brain tumors.
Leptomeningeal infiltration may present with dysfunction of multiple cranial nerves.
Etiology
Although few factors are unequivocally associated with an increased risk of brain cancer, most CNS neoplasms are thought to arise from individual cell mutations. A few inherited diseases, such as neurofibromatosis, tuberous sclerosis, multiple endocrine neoplasia (type 1), and retinoblastoma, increase the predilection to develop CNS tumors. Primary CNS lymphoma is a relatively frequent occurrence in HIV patients. A prior history of irradiation to the head for reasons other than treatment of the present tumor may increase the chance of primary brain tumor.
The most common tumors originating from the cerebellopontine angle are acoustic neuroma and meningioma.
Metastatic tumors reach the brain via hematogenous dissemination through the arterial system. Lung cancer—especially small cell lung cancer—is by far the most common solid tumor disseminating to the brain, followed by breast cancer, melanoma, and colon cancer. Less common sources of metastasis are testicular cancer and renal cell cancer. Prostate, uterine, and ovarian cancers are unlikely sources of brain metastasis.
Epidemiology
The American Cancer Society estimates that 24,530 brain and other nervous system cancers will be diagnosed in 2021. [3] Estimates of the annual incidence rate of primary brain tumors range from 7-19.1 cases per 100,000 population. Metastatic tumors to the brain are more common, with more than 200,000 patients per year in the United States with a new diagnosis of intracranial metastases. Pituitary adenomas are exceptionally common, and they are frequent incidental findings on autopsy. Autopsy series of patients with systemic cancer show that intracranial metastases are present in 18-24% of patients.
The International Agency for Research on Cancer of the World Health Organization estimates that in 2020, brain and nervous system cancers occurred in 168,346 men and 139,756 women worldwide. [4] Differences are seen between ethnic groups within the same country, and a 3-fold difference in incidence has been reported between countries worldwide. Developed countries appear to have the highest rates, but this may reflect better registration systems.
Meningiomas and pituitary adenomas are slightly more common in women than in men. Males are more likely to be diagnosed with brain tumors than females, with a male-to-female ratio of 1.5:1.
In children, brain tumors are the most prevalent solid tumor, second only to leukemia as a cause of pediatric cancer. The incidence rate of primary CNS neoplasms is 3.6 cases per 100,000 children each year. Tumors in the posterior fossa predominate in preadolescent children, with the incidence of supratentorial tumors increasing from adolescence to adulthood. Low-grade gliomas, such as astrocytomas, are more common in younger people than in older people. High-grade gliomas, such as anaplastic astrocytoma and glioblastoma multiforme, tend to originate in the fourth or fifth decade or beyond.
Prognosis
Prognostic features include the following:
-
Tumor resectability, tumor location, age of the patient, and tumor histology are the primary determinants of survival.
-
Without radiation therapy, the mean life expectancy of a patient with brain metastases is 1 month. Radiation therapy may extend survival to 4-6 months.
-
Patients with seizures secondary to a brain tumor generally experience obvious neurologic deterioration over a 6-month course.
-
Most patients with brain metastases die from progression of their primary malignancy rather than from brain damage.
In a study of 69 pediatric brain tumor survivors, the patients showed deficits in executive function, memory, and attention. Whole-brain radiation therapy, tumor size, young age at diagnosis, and male gender were risk factors for late cognitive sequelae. [5] Adult survivors of pediatric brain tumors have an increased risk of psychiatric illnesses, including depression, anxiety, suicidal ideation, schizophrenia and related psychoses, and behavioral problems. [6]
In the United States, brain and other nervous system cancers are expected to cause approximately 16,830 deaths in 2018. [3] Brain tumors are the second most common cancer in children, comprising 15-25% of all pediatric malignancies. Perhaps no other cancer is as feared as brain tumor, since severe disability, including paralysis, seizures, gait disturbances, and impairment of intellectual capacity may occur.
-
Brain neoplasms. CT images of several tumor types. Slide courtesy of UMASS Continuing Education Office.
-
Brain neoplasms. Colloid cyst of the third ventricle with obstructive hydrocephalus. Image courtesy of Peter Ferrera, MD.
-
Brain neoplasms. Occipital lobe glioblastoma with surrounding edema.
-
Brain neoplasms. Noncontrast CT scan of a tumor in the region of the posterior corpus callosum.
-
Brain neoplasms. Contrast CT scan of the same patient as in media file4. Notice that contrast enhancement brings out detail.










