Practice Essentials
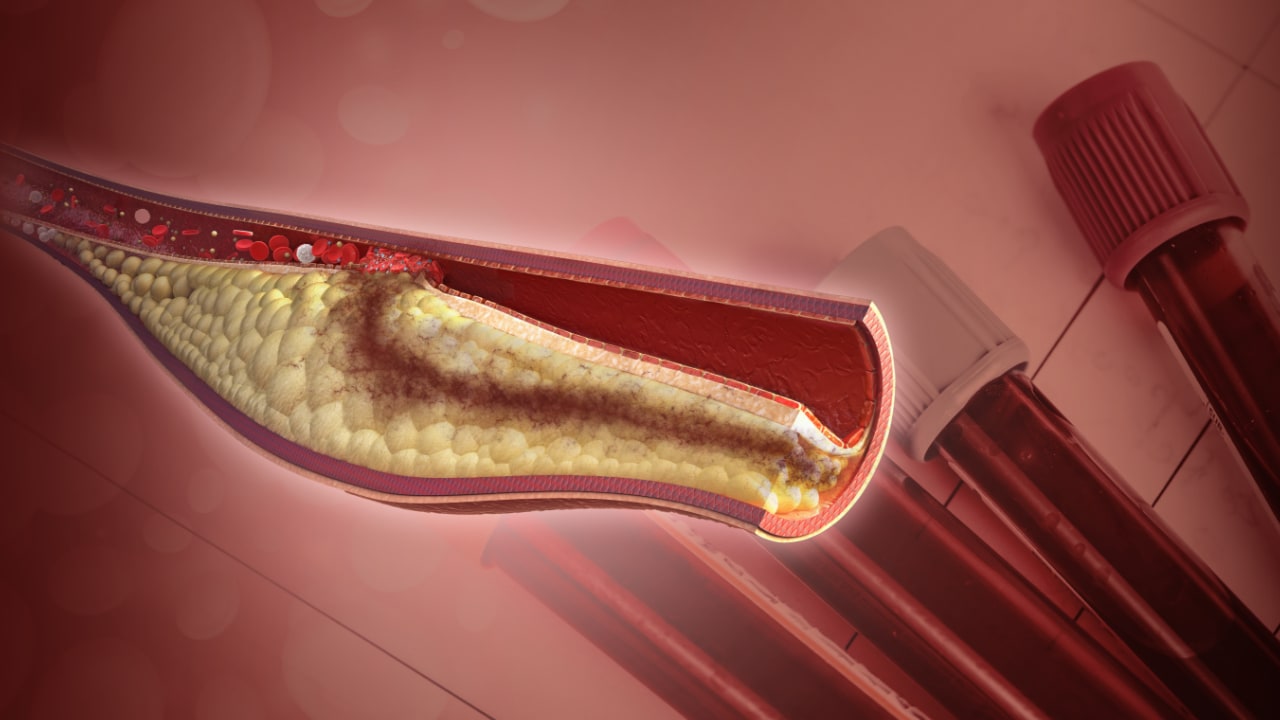
Acute coronary syndrome (ACS) refers to a spectrum of clinical presentations ranging from those for ST-segment elevation myocardial infarction (STEMI) to presentations found in non–ST-segment elevation myocardial infarction (NSTEMI) or in unstable angina. It is almost always associated with rupture of an atherosclerotic plaque and partial or complete thrombosis of the infarct-related artery.
The image below illustrates an algorithm for triaging patients with chest pain.
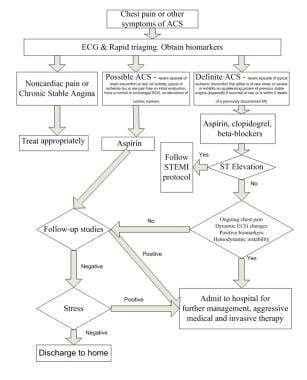 Suggested algorithm for triaging patients with chest pain. ACS = ACS; ASA = aspirin; EKG = ECG; MI = myocardial infarction; Rx = treat; STEMI = ST-elevation myocardial infarction. Courtesy of Wu et al (1999).
Suggested algorithm for triaging patients with chest pain. ACS = ACS; ASA = aspirin; EKG = ECG; MI = myocardial infarction; Rx = treat; STEMI = ST-elevation myocardial infarction. Courtesy of Wu et al (1999).
See Are You Missing Subtle MI Clues on ECGs? Test Your Skills, a Critical Images slideshow, to help identify a variety of electrocardiographic abnormalities.
Signs and symptoms
Atherosclerosis is the primary cause of ACS, with most cases occurring from the disruption of a previously nonsevere lesion. Complaints reported by patients with ACS include the following:
-
Palpitations
-
Pain, which is usually described as pressure, squeezing, or a burning sensation across the precordium and may radiate to the neck, shoulder, jaw, back, upper abdomen, or either arm
-
Exertional dyspnea that resolves with pain or rest
-
Diaphoresis from sympathetic discharge
-
Nausea from vagal stimulation
-
Decreased exercise tolerance
Physical findings can range from normal to any of the following:
-
Hypotension: Indicates ventricular dysfunction due to myocardial ischemia, myocardial infarction (MI), or acute valvular dysfunction
-
Hypertension: May precipitate angina or reflect elevated catecholamine levels due to anxiety or to exogenous sympathomimetic stimulation
-
Diaphoresis
-
Pulmonary edema and other signs of left heart failure
-
Extracardiac vascular disease
-
Jugular venous distention
-
Cool, clammy skin and diaphoresis in patients with cardiogenic shock
-
A third heart sound (S3) and, frequently, a fourth heart sound (S4)
-
A systolic murmur related to dynamic obstruction of the left ventricular outflow tract
-
Rales on pulmonary examination (suggestive of left ventricular dysfunction or mitral regurgitation)
Potential complications include the following:
-
Ischemia: Pulmonary edema
-
Myocardial infarction: Rupture of the papillary muscle, left ventricular free wall, and ventricular septum
See Presentation for more detail.
Diagnosis
Updated guidelines for the management of non-ST-segment elevation ACS were released in 2020 by the European Society of Cardiology (ESC). [1] The updates place increased reliance on high-sensitivity cardiac troponin testing (hs-cTn) for diagnosis. The guidelines include the use of the CRUSADE risk score (Can Rapid risk stratification of Unstable angina patients Suppress ADverse outcomes with Early implementation) of the ACC/AHA guidelines.
In the emergency setting, electrocardiography (ECG) is the most important diagnostic test for angina. ECG changes that may be seen during anginal episodes include the following:
-
Transient ST-segment elevations
-
Dynamic T-wave changes: Inversions, normalizations, or hyperacute changes
-
ST depressions: These may be junctional, downsloping, or horizontal
Laboratory studies that may be helpful include the following:
-
Creatine kinase isoenzyme MB (CK-MB) levels
-
Cardiac troponin levels
-
Myoglobin levels
-
Complete blood count
-
Basic metabolic panel
Diagnostic imaging modalities that may be useful include the following:
-
Chest radiography
-
Echocardiography
-
Myocardial perfusion imaging
-
Cardiac angiography
-
Computed tomography, including CT coronary angiography and CT coronary artery calcium scoring
See Workup for more detail.
Management
Initial therapy focuses on the following:
-
Stabilizing the patient’s condition
-
Relieving ischemic pain
-
Providing antithrombotic therapy
Pharmacologic anti-ischemic therapy includes the following:
-
Nitrates (for symptomatic relief)
-
Beta blockers (eg, metoprolol): These are indicated in all patients unless contraindicated
Pharmacologic antithrombotic therapy includes the following:
-
Aspirin
-
Clopidogrel
-
Prasugrel
-
Ticagrelor
-
Glycoprotein IIb/IIIa receptor antagonists (abciximab, eptifibatide, tirofiban)
Pharmacologic anticoagulant therapy includes the following:
-
Unfractionated heparin (UFH)
-
Low-molecular-weight heparin (LMWH; dalteparin, nadroparin, enoxaparin)
-
Factor Xa inhibitors (rivaroxaban, fondaparinux)
Additional therapeutic measures that may be indicated include the following:
-
Thrombolysis
-
Percutaneous coronary intervention (preferred treatment for ST-elevation MI)
Current guidelines for patients with moderate- or high-risk ACS include the following:
-
Early invasive approach
-
Concomitant antithrombotic therapy, including aspirin and clopidogrel, as well as UFH or LMWH
See Treatment and Medication for more detail.
The image below depicts a 62-year-old woman with a history of chronic stable angina and a "valve problem."
 A 62-year-old woman with a history of chronic stable angina and a "valve problem" presents with new chest pain. She is symptomatic on arrival, complaining of shortness of breath and precordial chest tightness. Her initial vital signs are blood pressure = 140/90 mm Hg and heart rate = 98. Her electrocardiogram (ECG) is as shown. She is given nitroglycerin sublingually, and her pressure decreases to 80/palpation. Right ventricular ischemia should be considered in this patient.
A 62-year-old woman with a history of chronic stable angina and a "valve problem" presents with new chest pain. She is symptomatic on arrival, complaining of shortness of breath and precordial chest tightness. Her initial vital signs are blood pressure = 140/90 mm Hg and heart rate = 98. Her electrocardiogram (ECG) is as shown. She is given nitroglycerin sublingually, and her pressure decreases to 80/palpation. Right ventricular ischemia should be considered in this patient.
Background
Acute coronary syndrome (ACS) refers to a spectrum of clinical presentations ranging from those for ST-segment elevation myocardial infarction (STEMI) to presentations found in non–ST-segment elevation myocardial infarction (NSTEMI) or in unstable angina. In terms of pathology, ACS is almost always associated with rupture of an atherosclerotic plaque and partial or complete thrombosis of the infarct-related artery. (See Etiology.)
In some instances, however, stable coronary artery disease (CAD) may result in ACS in the absence of plaque rupture and thrombosis, when physiologic stress (eg, trauma, blood loss, anemia, infection, tachyarrhythmia) increases demands on the heart. The diagnosis of acute myocardial infarction in this setting requires a finding of the typical rise and fall of biochemical markers of myocardial necrosis in addition to at least 1 of the following [2] (See Workup.):
-
Ischemic symptoms
-
Development of pathologic Q waves on electrocardiogram (ECG)
-
Significant ST-segment-T wave (ST-T) changes or new left bundle branch block (LBBB)
-
Imaging evidence of new loss of viable myocardium or new regional wall motion abnormality
-
Introcoronary thrombus identified by angiography or autopsy
The terms transmural and nontransmural (subendocardial) myocardial infarction are no longer used because ECG findings in patients with this condition are not closely correlated with pathologic changes in the myocardium. Therefore, a transmural infarct may occur in the absence of Q waves on ECGs, and many Q-wave myocardial infarctions may be subendocardial, as noted on pathologic examination. Because elevation of the ST segment during ACS is correlated with coronary occlusion and because it affects the choice of therapy (urgent reperfusion therapy), ACS-related myocardial infarction should be designated STEMI or NSTEMI. (See Workup.)
Attention to the underlying mechanisms of ischemia is important when managing ACS. A simple predictor of demand is rate-pressure product, which can be lowered by beta blockers (eg, metoprolol or atenolol) and pain/stress relievers (eg, morphine), while supply may be improved by oxygen, adequate hematocrit, blood thinners (eg, heparin, IIb/IIIa agents such as abciximab, eptifibatide, tirofiban, or thrombolytics), and/or vasodilators (eg, nitrates, amlodipine). (See Medication.)
Etiology
Acute coronary syndrome (ACS) is caused primarily by atherosclerosis. Most cases of ACS occur from disruption of a previously nonsevere lesion (an atherosclerotic lesion that was previously hemodynamically insignificant yet vulnerable to rupture). The vulnerable plaque is typified by a large lipid pool, numerous inflammatory cells, and a thin, fibrous cap.
Elevated demand can produce ACS in the presence of a high-grade fixed coronary obstruction, due to increased myocardial oxygen and nutrition requirements, such as those resulting from exertion, emotional stress, or physiologic stress (eg, from dehydration, blood loss, hypotension, infection, thyrotoxicosis, or surgery).
ACS without elevation in demand requires a new impairment in supply, typically due to thrombosis and/or plaque hemorrhage.
The major trigger for coronary thrombosis is considered to be plaque rupture caused by the dissolution of the fibrous cap, the dissolution itself being the result of the release of metalloproteinases (collagenases) from activated inflammatory cells. This event is followed by platelet activation and aggregation, activation of the coagulation pathway, and vasoconstriction. This process culminates in coronary intraluminal thrombosis and variable degrees of vascular occlusion. Distal embolization may occur. The severity and duration of coronary arterial obstruction, the volume of myocardium affected, the level of demand on the heart, and the ability of the rest of the heart to compensate are major determinants of a patient's clinical presentation and outcome. (Anemia and hypoxemia can precipitate myocardial ischemia in the absence of severe reduction in coronary artery blood flow.)
A syndrome consisting of chest pain, ischemic ST-segment and T-wave changes, elevated levels of biomarkers of myocyte injury, and transient left ventricular apical ballooning (takotsubo syndrome) has been shown to occur in the absence of clinical CAD, after emotional or physical stress. The etiology of this syndrome is not well understood but is thought to relate to a surge of catechol stress hormones and/or high sensitivity to those hormones.
Baseline blood glucose levels appear to be an independent risk factor for a major adverse cardiac event (MACE) in emergency department (ED) patients with suspected ACS. [3, 4] In an analysis of data from 1708 Australian and New Zealand patients in a prospective observational study, investigators noted a MACE occurred within 30 days of presentation in 15.3% of patients whose ED admission blood glucose levels were below 7 mmol/L (about 126 mg/dL); however, in the same time period, a MACE occurred in twice as many patients (30.9%) whose blood glucose levels were above 7 mmol/L. [4] After controlling for various factors, patients who had admission blood glucose levels of 7 mmol/L or higher were at 51% higher risk of experiencing a MACE compared with patients who had lower baseline blood glucose levels. [4] Other significant predictors of MACE included male sex, older age, family history, hypertension, dyslipidemia, ischemic findings on ECG, and positive troponintests. [3, 4]
Prognosis
Six-month mortality rates in the Global Registry of Acute Coronary Events (GRACE) were 13% for patients with NSTEMI ACS and 8% for those with unstable angina.
An elevated level of troponin (a type of regulatory protein found in skeletal and cardiac muscle) permits risk stratification of patients with ACS and identifies patients at high risk for adverse cardiac events (ie, myocardial infarction, death) up to 6 months after the index event. [5, 6] (See Workup.)
The PROVE IT-TIMI trial found that after ACS, a J-shaped or U-shaped curve association is observed between BP and the risk of future cardiovascular events. [7]
LeLeiko et al determined that serum choline and free F(2)-isoprostane are also predictors of cardiac events in ACS. The authors evaluated the prognostic value of vascular inflammation and oxidative stress biomarkers in patients with ACS to determine their role in predicting 30-day clinical outcomes. Serum F(2)-isoprostane had an optimal cutoff level of 124.5 pg/mL, and serum choline had a cutoff level of 30.5 µmol/L. Choline and F(2)-isoprostane had a positive predictive value of 44% and 57% and a negative predictive value of 89% and 90%, respectively. [8]
Testosterone deficiency is common in patients with coronary disease and has a significant negative impact on mortality. Further study is needed to assess the effect of treatment on survival. [9]
A study by Sanchis et al suggests renal dysfunction, dementia, peripheral artery disease, previous heart failure, and previous myocardial infarction are the comorbid conditions that predict mortality in NSTEMI ACS. [10] In patients with comorbid conditions, the highest risk period was in the first weeks after NSTEMI ACS. In-hospital management of patients with comorbid conditions merits further investigation.
Patients with end-stage renal disease often develop ACS, and little is known about the natural history of ACS in patients receiving dialysis. Gurm et al examined the presentation, management, and outcomes of patients with ACS who received dialysis before presentation for an ACS. These patients were enrolled in the Global Registry of Acute Coronary Events (GRACE) at 123 hospitals in 14 countries from 1999-2007.
NSTEMI ACS was the most common in patients receiving dialysis, occurring in 50% of patients (290 of 579) versus 33% (17,955 of 54,610) of those not receiving dialysis The in-hospital mortality rates were higher among patients receiving dialysis (12% vs 4.8%; p < 0.0001). Higher 6-month mortality rates (13% vs 4.2%; p < 0.0001), recurrent myocardial infarction incidence (7.6% vs 2.9%; p < 0.0001), and unplanned rehospitalizations (31% vs 18%; p < 0.0001) were found among those who survived to discharge. Outcomes in patients who received dialysis was worse than was predicted by the calculated GRACE risk score for in-hospital mortality (7.8% predicted vs 12% observed; p < 0.05). This suggests that the GRACE risk score underestimated the risk of major events in these patients. [11]
In a study that assessed the impact of prehospital time on STEMI outcome, Chughatai et al suggest that "total time to treatment" should be used as a core measure instead of "door-to-balloon time." [12] This is because on-scene time was the biggest fraction of "pre-hospital time." The study compared groups with total time to treatment of more than 120 minutes compared with 120 minutes or less and found mortalities were 4 compared with 0 and transfers to a tertiary care facility were 3 compared with 1, respectively.
STEMI mechanisms and stenting outcome similar in women and men
Despite their smaller coronary vessels and higher risk profile, women with STEMI appear to respond just as well as men to primary PCI and stenting, according to the Optical Coherence Tomography Assessment of Gender Diversity in Primary Angioplasty (OCTAVIA) study. [13] OCTAVIA, which was designed to examine gender differences at the time of primary PCI, included 140 STEMI patients at 14 Italian centers, matched by age and risk factors, who received an everolimus-eluting stent. [13]
On initial OCT, no differences by gender were found in the proportion of ruptured or eroded plaques, thus suggesting that the pathophysiology of STEMI is nearly identical in men and women. [13] On repeat OCT at nine months, intended to assess stent healing, more than 90% of both men and women had fully covered stent struts. Although OCTAVIA was not powered for clinical end points, no significant differences in death, reinfarction, stroke, stent thrombosis, or target vessel reintervention were evident at one year. [13]
Complications
Complications of ischemia include pulmonary edema, whereas those of myocardial infarction include rupture of the papillary muscle, left ventricular free wall, and ventricular septum.
Patient Education
Patient education of risk factors is important, but more attention is needed regarding delays in door-to-balloon time, and one major barrier to improving this delay is patient education regarding his or her symptoms. Lack of recognition of symptoms may cause tremendous delays in seeking medical attention.
Educate patients about the dangers of cigarette smoking, a major risk factor for coronary artery disease (CAD). The risk of recurrent coronary events decreases 50% at 1 year after smoking cessation. Provide all patients who smoke with guidance, education, and support to avoid smoking. Smoking-cessation classes should be offered to help patients avoid smoking after a myocardial infarction. Bupropion increases the likelihood of successful smoking cessation.
Diet plays an important role in the development of CAD. Therefore, prior to hospital discharge, a patient who has had a myocardial infarction should be evaluated by a dietitian. Patients should be informed about the benefits of a low-cholesterol, low-salt diet. In addition, educate patients about AHA dietary guidelines regarding a low-fat, low-cholesterol diet.
A cardiac rehabilitation program after discharge may reinforce education and enhance compliance.
The following mnemonic may useful in educating patients with CAD regarding treatments and lifestyle changes necessitated by their condition:
-
A = Aspirin and antianginals
-
B = Beta blockers and blood pressure (BP)
-
C = Cholesterol and cigarettes
-
D = Diet and diabetes
-
E = Exercise and education
For patients being discharged home, emphasize the following:
-
Timely follow-up with primary care provider
-
Compliance with discharge medications, specifically aspirin and other medications used to control symptoms
-
Need to return to the ED for any change in frequency or severity of symptoms
For patient education resources, see the Heart Health Center and Cholesterol Center, as well as High Cholesterol, Cholesterol Charts (What the Numbers Mean), Lifestyle Cholesterol Management, Chest Pain, Coronary Heart Disease, Heart Attack, Angina Pectoris, Cholesterol-Lowering Medications, and Statins (Cholesterol Drugs).
-
A 50-year-old man with type 1 diabetes mellitus and hypertension presents after experiencing 1 hour of midsternal chest pain that began after eating a large meal. Pain is now present but is minimal. Aspirin is the single drug that will have the greatest potential impact on subsequent morbidity. In the setting of ongoing symptoms and electrocardiogram (ECG) changes, nitrates titrated to 10% reduction in blood pressure and symptoms, beta blockers, and heparin are all indicated. If the patient continues to have persistent signs and/or symptoms of ischemia, addition of a glycoprotein IIb/IIIa inhibitor should be considered.
-
A 62-year-old woman with a history of chronic stable angina and a "valve problem" presents with new chest pain. She is symptomatic on arrival, complaining of shortness of breath and precordial chest tightness. Her initial vital signs are blood pressure = 140/90 mm Hg and heart rate = 98. Her electrocardiogram (ECG) is as shown. She is given nitroglycerin sublingually, and her pressure decreases to 80/palpation. Right ventricular ischemia should be considered in this patient.
-
This plot shows changes in cardiac markers over time after the onset of symptoms. Peak A is the early release of myoglobin or creatine kinase isoenzyme MB (CK-MB) after acute myocardial infarction (AMI). Peak B is the cardiac troponin level after infarction. Peak C is the CK-MB level after infarction. Peak D is the cardiac troponin level after unstable angina. Data are plotted on a relative scale, where 1.0 is set at the myocardial-infarction cutoff concentration. Courtesy of Wu et al (1999). ROC = receiver operating characteristic.
-
Suggested algorithm for triaging patients with chest pain. ACS = ACS; ASA = aspirin; EKG = ECG; MI = myocardial infarction; Rx = treat; STEMI = ST-elevation myocardial infarction. Courtesy of Wu et al (1999).
-
Use of cardiac markers in the ED. Studies on troponins in ACS.
-
Use of cardiac markers in the ED. Troponin I levels and cardiac mortality in ACS.
-
Use of cardiac markers in the ED. Cardiac event rates in the platelet receptor inhibition for ischemic syndrome (PRISM) study based on troponin I results.
-
Use of cardiac markers in the ED. Effect of time to treatment in patients with acute coronary syndrome (ACS) who are treated with the GIIb/IIIa inhibitor eptifibatide.
Tables
What would you like to print?
- Overview
- Presentation
- DDx
- Workup
- Approach Considerations
- Electrocardiography
- Measurement of CK-MB Levels
- Measurement of Troponin levels
- Measurement of Myoglobin Levels
- Complete Blood Count Determination
- Basic Metabolic Panel
- New Biomarkers
- Chest Radiography
- Echocardiography
- Myocardial Perfusion Imaging
- Cardiac Angiography
- Computed Tomography Coronary Angiography and CT Coronary Artery Calcium Scoring
- Other Techniques
- Show All
- Treatment
- Guidelines
- Medication
- Questions & Answers
- Media Gallery
- Tables
- References