Background
Hemorrhoids are swollen blood vessels in the lower rectum. They are among the most common causes of anal pathology, and subsequently are blamed for virtually any anorectal complaint by patients and medical professionals alike. Confusion often arises because the term "hemorrhoid" has been used to refer to both normal anatomic structures and pathologic structures. In the context of this article, "hemorrhoids" refers to the pathologic presentation of hemorrhoidal venous cushions.
Hemorrhoidal venous cushions are normal structures of the anorectum and are anatomically present unless a previous intervention has taken place. Because of their rich vascular supply, highly sensitive location, and tendency to engorge and prolapse, hemorrhoidal venous cushions are common causes of anal pathology. [1] Symptoms can range from mildly bothersome, such as pruritus, to quite concerning, such as rectal bleeding.
Although hemorrhoids are a common condition diagnosed in clinical practice, many patients are too embarrassed to seek treatment. Consequently, the true prevalence of pathologic hemorrhoids is not known. [2] In addition, although hemorrhoids are responsible for a large portion of anorectal complaints, it is important to rule out more serious conditions, such as other causes of gastrointestinal (GI) bleeding, before reflexively attributing symptoms to hemorrhoids. [3]
In a study of 198 physicians from different specialties, Grucela et al found the rate of correct identification for seven common, benign anal pathologic conditions (including anal abscess, fissure, and fistula; prolapsed internal hemorrhoid; thrombosed external hemorrhoid; condyloma acuminata; and full-thickness rectal prolapse) was greatest for condylomata and rectal prolapse and was lowest for hemorrhoidal conditions. [4] There was no correlation between diagnostic accuracy and years of physician experience. The investigators found the overall diagnostic accuracy among the physicians to be 53.5%, with the accuracy for surgeons being 70.4% and that for the rest of the doctors being less than 50%. [4]
Historical note
Hemorrhoidal symptoms have historically been treated with dietary modifications, incantations, voodoo, quackery, and application of a hot poker. Molten lead has also been described as a treatment. The adverse effects of these treatments have a direct relationship to whether patients relay persistent or recurrent complaints to the clinician or return for further treatment.
For patient education information, see the Digestive Disorders Center as well as Hemorrhoids, Anal Abscess, Rectal Pain, and Rectal Bleeding.
See also the following:
Anatomy
Hemorrhoids are not varicosities; they are clusters of vascular tissue (eg, arterioles, venules, arteriolar-venular connections), smooth muscle (eg, Treitz muscle), and connective tissue lined by the normal epithelium of the anal canal. Hemorrhoids are present in utero and persist through normal adult life. Evidence indicates that hemorrhoidal bleeding is arterial and not venous. This evidence is supported by the bright red color and arterial pH of the blood.
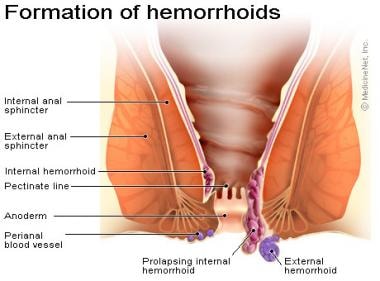
Hemorrhoids are classified by their anatomic origin within the anal canal and by their position relative to the dentate line; thus, they are categorized into internal and external hemorrhoids (see the following image).
External hemorrhoids develop from ectoderm and are covered by squamous epithelium, whereas internal hemorrhoids are derived from embryonic endoderm and lined with the columnar epithelium of anal mucosa. Similarly, external hemorrhoids are innervated by cutaneous nerves that supply the perianal area. These nerves include the pudendal nerve and the sacral plexus. Internal hemorrhoids are not supplied by somatic sensory nerves and therefore cannot cause pain. At the level of the dentate line, internal hemorrhoids are anchored to the underlying muscle by the mucosal suspensory ligament.
Hemorrhoidal venous cushions are a normal part of the human anorectum and arise from subepithelial connective tissue within the anal canal. Internal hemorrhoids have three main cushions, which are situated in the left lateral, right posterior (most common), and right anterior areas of the anal canal. However, this combination is found in only 19% of patients; hemorrhoids can be found at any position within the rectum. Minor tufts can be found between the major cushions.
Present in utero, these cushions surround and support distal anastomoses between the superior rectal arteries and the superior, middle, and inferior rectal veins. They also contain a subepithelial smooth muscle layer, contributing to the bulk of the cushions. Normal hemorrhoidal tissue accounts for approximately 15-20% of resting anal pressure and provides important sensory information, enabling the differentiation between solid, liquid, and gas.
External hemorrhoidal veins are found circumferentially under the anoderm; they can cause trouble anywhere around the circumference of the anus.
Venous drainage of hemorrhoidal tissue mirrors embryologic origin. Internal hemorrhoids drain through the superior rectal vein into the portal system. External hemorrhoids drain through the inferior rectal vein into the inferior vena cava. Rich anastomoses exist between these two and the middle rectal vein, connecting the portal and systemic circulations.
Mixed hemorrhoids are confluent internal and external hemorrhoids.
Etiology and Pathophysiology
The term hemorrhoid is usually related to the symptoms caused by hemorrhoids. Hemorrhoids are present in healthy individuals. In fact, hemorrhoidal columns exist in utero. When these vascular cushions produce symptoms, they are referred to as hemorrhoids. Hemorrhoids generally cause symptoms when they become enlarged, inflamed, thrombosed, or prolapsed.
Most symptoms arise from enlarged internal hemorrhoids. Abnormal swelling of the anal cushions causes dilatation and engorgement of the arteriovenous plexuses. This leads to stretching of the suspensory muscles and eventual prolapse of rectal tissue through the anal canal. The engorged anal mucosa is easily traumatized, leading to rectal bleeding that is typically bright red due to high blood oxygen content within the arteriovenous anastomoses. Prolapse leads to soiling and mucus discharge (triggering pruritus) and predisposes to incarceration and strangulation.
Although many patients and clinicians believe that hemorrhoids are caused by chronic constipation, prolonged sitting, and vigorous straining, little evidence to support a causative link exists. Some of these potential etiologies are briefly discussed below.
Decreased venous return
Most authors agree that low-fiber diets cause small-caliber stools, which result in straining during defecation. This increased pressure causes engorgement of the hemorrhoids, possibly by interfering with venous return. Pregnancy and abnormally high tension of the internal sphincter muscle can also cause hemorrhoidal problems, presumably by means of the same mechanism, which is thought to be decreased venous return. Prolonged sitting on a toilet (eg, while reading) is believed to cause a relative venous return problem in the perianal area (a tourniquet effect), resulting in enlarged hemorrhoids. Aging causes weakening of the support structures, which facilitates prolapse. Weakening of support structures can occur as early as the third decade of life.
Straining and constipation
Straining and constipation have long been thought of as culprits in the formation of hemorrhoids. This may or may not be true. [5, 6, 7] Patients who report hemorrhoids have a canal resting tone that is higher than normal. Of interest, the resting tone is lower after hemorrhoidectomy than it is before the procedure. This change in resting tone is the mechanism of action of Lord dilatation, a surgical procedure for anorectal complaints that is most commonly performed in the United Kingdom.
Pregnancy
Pregnancy clearly predisposes women to symptoms from hemorrhoids, although the etiology is unknown. Notably, most patients revert to their previously asymptomatic state after delivery. The relationship between pregnancy and hemorrhoids lends credence to hormonal changes or direct pressure as the culprit.
Portal hypertension and anorectal varices
Portal hypertension has often been mentioned in conjunction with hemorrhoids. [8, 9, 10] However, hemorrhoidal symptoms do not occur more frequently in patients with portal hypertension than in those without it, and massive bleeding from hemorrhoids in these patients is unusual. Bleeding is very often complicated by coagulopathy. If bleeding is found, direct suture ligation of the offending column is suggested.
Anorectal varices are common in patients with portal hypertension. [11] Varices occur in the midrectum, at connections between the portal system and the middle and inferior rectal veins. Varices occur more frequently in patients who are noncirrhotic, and they rarely bleed. Treatment is usually directed at the underlying portal hypertension. Emergent control of bleeding can be obtained with suture ligation. Portosystemic shunts and transjugular intrahepatic portosystemic shunts (TIPS) have been used to control hypertension and thus, the bleeding. [12]
Other risk factors
Other risk factors historically associated with the development of hemorrhoids include the following:
-
Lack of erect posture
-
Familial tendency
-
Higher socioeconomic status
-
Chronic diarrhea
-
Colon malignancy
-
Hepatic disease
-
Obesity
-
Elevated anal resting pressure
-
Spinal cord injury
-
Loss of rectal muscle tone
-
Rectal surgery
-
Episiotomy
-
Anal intercourse
-
Inflammatory bowel disease, including ulcerative colitis, and Crohn disease
Pathophysiology of symptoms of internal hemorrhoids
Internal hemorrhoids cannot cause cutaneous pain, because they are above the dentate line and are not innervated by cutaneous nerves. However, they can bleed, prolapse, and, as a result of the deposition of an irritant onto the sensitive perianal skin, cause perianal itching and irritation. Internal hemorrhoids can produce perianal pain by prolapsing and causing spasm of the sphincter complex around the hemorrhoids. This spasm results in discomfort while the prolapsed hemorrhoids are exposed. This muscle discomfort is relieved with reduction.
Internal hemorrhoids can also cause acute pain when incarcerated and strangulated. Again, the pain is related to the sphincter complex spasm. Strangulation with necrosis may cause more deep discomfort. When these catastrophic events occur, the sphincter spasm often causes concomitant external thrombosis. External thrombosis causes acute cutaneous pain. This constellation of symptoms is referred to as acute hemorrhoidal crisis and usually requires emergent treatment.
Internal hemorrhoids most commonly cause painless bleeding with bowel movements. The covering epithelium is damaged by the hard bowel movement, and the underlying veins bleed. With spasm of the sphincter complex elevating pressure, the internal hemorrhoidal veins can spurt.
Internal hemorrhoids can deposit mucus onto the perianal tissue with prolapse. This mucus with microscopic stool contents can cause a localized dermatitis, which is called pruritus ani. Generally, hemorrhoids are merely the vehicle by which the offending elements reach the perianal tissue. Hemorrhoids are not the primary offenders.
Pathophysiology of symptoms of external hemorrhoids
External hemorrhoids cause symptoms in two ways. First, acute thrombosis of the underlying external hemorrhoidal vein can occur. Acute thrombosis is usually related to a specific event, such as physical exertion, straining with constipation, a bout of diarrhea, or a change in diet. These are acute, painful events.
Pain results from rapid distention of innervated skin by the clot and surrounding edema. The pain lasts 7-14 days and resolves with resolution of the thrombosis. With this resolution, the stretched anoderm persists as excess skin or skin tags. External thromboses occasionally erode the overlying skin and cause bleeding. Recurrence occurs approximately 40-50% of the time, at the same site (because the underlying damaged vein remains there). Simply removing the blood clot and leaving the weakened vein in place, rather than excising the offending vein with the clot, will predispose the patient to recurrence.
External hemorrhoids can also cause hygiene difficulties, with the excess, redundant skin left after an acute thrombosis (skin tags) being accountable for these problems. External hemorrhoidal veins found under the perianal skin obviously cannot cause hygiene problems; however, excess skin in the perianal area can mechanically interfere with cleansing.
Epidemiology
Worldwide, the prevalence of symptomatic hemorrhoids is estimated at 4.4% in the general population. In the United States, up to one third of the 10 million people with hemorrhoids seek medical treatment, resulting in 1.5 million related prescriptions per year.
The number of hemorrhoidectomies performed in US hospitals is declining. A peak of 117 hemorrhoidectomies per 100,000 people was reached in 1974; this rate declined to 37 hemorrhoidectomies per 100,000 people in 1987. Outpatient and office treatment of hemorrhoids account for some of this decline.
Patients presenting with hemorrhoidal disease are more frequently white, from higher socioeconomic status, and from rural areas. There is no known sex predilection, although men are more likely to seek treatment. However, pregnancy causes physiologic changes that predispose women to developing symptomatic hemorrhoids. As the gravid uterus expands, it compresses the inferior vena cava, causing decreased venous return and distal engorgement.
External hemorrhoids occur more commonly in young and middle-aged adults than in older adults. The prevalence of hemorrhoids increases with age, with a peak in persons aged 45-65 years.
Prognosis
Most hemorrhoids resolve spontaneously or with conservative medical therapy alone. However, complications can include thrombosis, secondary infection, ulceration, abscess, and incontinence. The recurrence rate with nonsurgical techniques is 10-50% over a 5-year period, whereas that of surgical hemorrhoidectomy is less than 5%.
Regarding complications from surgery, well-trained surgeons should experience complications in fewer than 5% of cases. Complications include stenosis, bleeding, infection, recurrence, nonhealing wounds, and fistula formation. Urinary retention is directly related to the anesthetic technique used and to the perioperative fluids administered. Limiting fluids and the routine use of local anesthesia can reduce urinary retention to less than 5%.
-
Hemorrhoids. Anatomy of external hemorrhoid. Image courtesy of MedicineNet, Inc.
-
Hemorrhoids. Thrombosed hemorrhoid. This hemorrhoid was treated by incision and removal of a clot.