Practice Essentials
Maxillofacial fractures result from blunt or penetrating trauma. [1, 2, 3, 4, 5, 6, 7] Blunt injuries are far more common, including vehicular accidents, altercations, sports-related trauma, occupational injuries, and falls. Penetrating injuries include gunshot wounds, stabbings, and explosions. Simple nasal fractures are the most common of all facial fractures and must be distinguished from the more serious nasoethmoidal (NOE) fractures. NOE fractures extend into the nose through the ethmoid bones. Fractures through the ethmoid are prone to cerebrospinal fluid (CSF) leaks from dural tears.
Zygomatic arch fractures generally occur in 2 or 3 locations along the arch. Zygomaticomaxillary, or tripod, fractures occur at articulations of the zygoma with the frontal bone maxillae and zygomatic arch. Alveolar fractures occur just above the level of the teeth through the alveolar portion of the maxilla. [8]
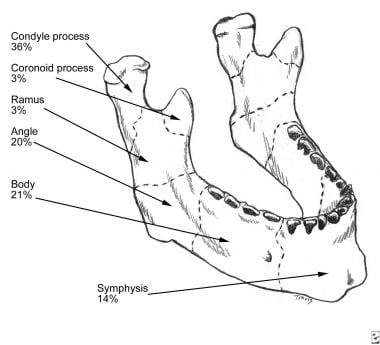
Mandibular fracture is one of the most common maxillofacial fractures observed in the emergency department and are caused primarily by motor vehicle accidents. Clinical features of this injury include malocclusion and loss of mandibular function. Mandibular fractures include fractures of the symphysis/parasymphysis, horizontal branch, angle, ramus, condyle, and coronoid process. [9, 10, 11]
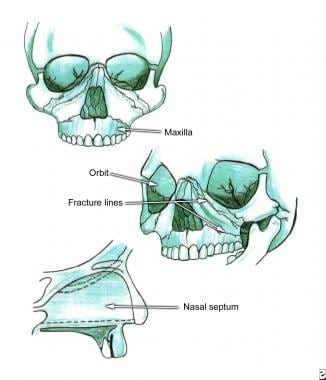
Le Fort or midface fractures are classified as types I, II, and III. Type I fracture extends through the lower third of the septum and involves the maxillary sinus. Type II (pyramidal) fracture extends from the nasal bone, through the lacrimal bone, and down through the zygomaticomaxillary suture.Type III fracture separates facial bones from the cranium, causing the face to appear long and flat. [12]
The first priority is to perform a primary survey and attend to ABCs, as maxillofacial fractures are caused by significant trauma, [4, 5, 6, 7] as well as gross neurologic function and control of the cervical spine.
(See the image below.)
Endotracheal anesthesia and radiography developed during the First World War led to better understanding and treatment of facial fractures. [13] During the Second World War, a multidisciplinary approach to treatment of facial fractures continued to improve the outcomes of severely injured soldiers. The more recent introduction of CT reconstruction, along with new surgical techniques, has improved cosmetic results immensely.
Diagnosis
Nasal bone fractures can be diagnosed clinically by history and physical examination. Plain nasal films consisting of a lateral view coning down on the nose and a Waters view can confirm the diagnosis. [14]
The best film for evaluating zygomatic arch is an underexposed submental view, also known as bucket handle view, because arches appear as bucket handles. Fracture also can be seen on a Waters view, and in some cases on a Towne view, of a facial series. [15, 16, 8]
If tripod fracture is suspected, plain films should include Waters, Caldwell, and underexposed submental views. If tripod fracture is strongly suspected, obtaining a CT scan directly without plain films is probably the most cost-effective approach. [17, 18]
Coronal CT scan of facial bones has replaced plain films in evaluation of Le Fort fractures, especially with use of 3-D reconstruction. Since Le Fort fractures often are mixed from one side to the other, CT scan is superior to plain films and makes visualization of the fracture for repair much easier.
Perform chest films if teeth are missing to rule out tooth aspiration.
Test clear rhinorrhea for glucose. Nasal secretions, unlike CSF, are normally low in glucose. If blood is present, this test is unreliable. Blood-tinged fluid can be placed on filter paper to look for a double ring sign of CSF around blood, but this is not a reliable test.
When CSF rhinorrhea is suspected, fluorescein may be injected into the lumbar subarachnoid space. Observe with a Wood lamp 30 minutes later for fluorescence of nasal discharge; if present, this confirms CSF rhinorrhea. This procedure is not usually performed by emergency physicians.
Management in the ED
ABCs take priority. Reassess airway frequently. Early intubation, before edema occurs, can make airway control much easier than waiting until a problem arises from obstruction. When intubation by oral route is impossible, perform a cricothyroidotomy to secure the airway.
Facial fractures tend to be very painful. Provide adequate analgesia, including oral opioids and NSAIDs. If nasal packing is used, antibiotics are generally used to prevent toxic shock. [19]
Epistaxis may require anterior nasal packing to control bleeding. Posterior packing may occasionally be needed.
Drain septal hematomas to avoid necrosis of septal cartilage.
Refer patients with facial fractures to an oral and maxillofacial surgeon, ear, nose, and throat (ENT) surgeon, or plastic surgeon who is experienced in care of these injuries.
Consult a neurosurgeon if a CSF leak is diagnosed or suspected.
Refer care of patients with multiple injuries to a surgeon with experience in trauma care. If a surgeon with trauma experience is not available, transfer patient to a higher-level trauma center.
The incidence of posttraumatic stress disorder is high in patients with facial injuries, and consultation with a psychiatrist should be considered. [20]
Patient education
If band arch wires are placed, teach patients how to release the crossband in an emergency.
Give instructions for epistaxis if this has occurred.
Discuss the risk of posttraumatic stress disorder. [20]
Pathophysiology
Mass, density, and shape of the striking object, as well as speed of impact, directly affect type and severity of facial injury. The force required to fracture various facial bones may be classified as high impact (greater than 50 times force of gravity [g]) or low impact (less than 50 g). High impact includes the following: supraorbital rim, 200 g; symphysis mandible, 100 g; frontal-glabellar:,100 g; angle of mandible, 70 g. Low impact inlcudes zygoma (50 g) and nasal bone (30 g).
Simple nasal fractures are the most common facial fractures and must be distinguished from the more serious nasoethmoidal (NOE) fractures. NOE fractures extend into the nose through the ethmoid bones. Fractures through the ethmoid are prone to cerebrospinal fluid (CSF) leaks from dural tears.
Zygomatic arch fractures tend to occur in 2-3 places along the arch. Often, 3 breaks occur, 1 at each end of the arch and a third in the middle, forming a V-shaped fracture; this often impinges on the temporalis muscle below, causing trismus.
Zygomaticomaxillary (tripod) fractures result from a direct blow to the cheek. Fracture occurs at articulations of the zygoma with the frontal bone maxillae and zygomatic arch and often extends through the orbital floor. Because the infraorbital nerve passes through the orbital floor, hypesthesia often occurs in its sensory distribution.
Alveolar fractures occur just above the level of the teeth through the alveolar portion of the maxilla. Usually a group of teeth is loose, and blood is noted at the gingival line.
Le Fort fractures
Le Fort or midface fractures are classified into 3 types and occasionally are mixed from one side of the face to the other.
-
Le Fort I: Horizontal maxillary fracture separates the maxillary process (hard palate) from the rest of the maxilla. Fracture extends through the lower third of the septum and involves the maxillary sinus. This is below the level of the infraorbital nerve and thus does not cause hypesthesia.
-
Le Fort II: Pyramidal fracture starts at the nasal bone, extends through the lacrimal bone, and courses downward through the zygomaticomaxillary suture. It courses posteriorly through the maxilla and below the zygoma into the upper pterygoid plates. The inner canthus of the nasal bridge is widened. Because the fracture extends through the zygoma, near the exit of the infraorbital nerve, hypesthesia often is present. Bilateral subcutaneous hematomas often are present.
-
Le Fort III: Craniofacial dysjunction also starts at the nasal bridge. It extends posteriorly through the ethmoid bones and laterally through the orbits below the optic foramen, through the pterygomaxillary suture into the sphenopalatine fossa. This fracture separates facial bones from cranium, causing the face to appear long and flat (ie, dish face).
Epidemiology
Approximately 3 million facial injuries occur annually, but most do not involve maxillofacial fractures. [13, 4, 5, 6, 7, 21, 1] One study placed the incidence of severe maxillofacial injury (fractures and lacerations) at 0.04-0.09% for motor vehicle collisions. Motor vehicle-related injuries are more common in rural areas, and altercation-related injuries are more frequent in inner cities.
Mortality/Morbidity
Incidence of other major injuries is as high as 50% in high-impact facial fractures, compared with 21% for low-impact fractures. Motor vehicle collision-related fractures are more likely to have associated injuries than violence-related fractures. Mortality is as high as 12% in high-impact fractures but is rarely due to maxillofacial injury. The incidence of associated cervical spine injuries has been reported in the 0.2-6% range.
In a 10-year retrospective study of the incidence and etiology of maxillofacial trauma associated with brain injury, frontal sinus fractures were the most common maxillofacial fractures (21.9%) associated with neurosurgical input, followed by mandibular fractures and zygomatic complex fractures. In the general maxillofacial trauma population, frontal sinus fractures were only found in 2.2% of the cases. The main cause of injury was automobile accidents, followed by falls. [22]
A study of complications in patients with maxillofacial trauma found that patients in car collisions were most likely to develop complications (92.3%), followed by falls (66.7%). Patients aged 60-69 years experienced the highest complication rate, followed by patients aged 20-29 years and then 30-39 years. The majority of complications were infection and inflammation (36.4%), followed by neurologic deficit (24.0%), physiologic dysregulation (11.6%), and facial bone deformity (8.3%). The most common treatment was pharmacologic, followed by antibiotic treatment, conservative treatment, and decompression therapy. [23]
According to the Global Burden of Disease Study (GBD) data on injury and disability due to facial fractures for 2017, there were 7,538,663 new cases; 1,819,732 prevalent cases; and 117,402 years lived with disability (YLD). [24]
Age and Sex
Adult male-to-female ratio is 3:1. Suspect domestic violence or sexual assault in women, as this may coexist in 30% of cases.
Male predominance is reduced to 3:2 in children. Child abuse should be suspected, particularly in nonmotor vehicular injuries. The incidence of maxillofacial fractures has increased in older patients. [25]
In a study of facial fractures in the elderly (>64 yr) compared with those in younger patients, elderly patients tended to experience less severe facial fractures and were more likely to have experienced injury from a fall. Compared to younger patients, the older patients sustained a higher incidence of maxillary, nasal, and orbital floor fractures and a lower incidence of mandible fractures. [26]
A study of 336,124 ED visits for facial fractures in patients 21 years of age or younger found that the most common facial fractures were those of the nasal bones and mandible. Younger children were more likely to have falls, pedal cycle accidents, pedestrian accidents, and transport accidents, whereas older groups were more likely to have firearm injuries, motor vehicle traffic accidents, and assaults. [3]
-
The bony walls of the orbit.
-
Le Fort fractures.
-
Mandibular fractures.
-
3D CT scan of right displaced zygomaticomaxillary complex fracture.