Practice Essentials
Elbow fractures are commonly encountered in the acute care setting. Injury patterns for children and adults are quite different. Fractures of the elbow include extra-articular and intra-articular fractures. Extra-articular fractures include intercondylar fractures, supracondylar fractures, epicondylar fractures, and condyle fractures. Intra-articular fractures include trochlea and capitellum, radial head, and proximal ulnar fractures. The examining physician must perform a thorough neurovascular examination with all suspected elbow fractures; recognize subtle fracture patterns; provide adequate immobilization; and assess whether fractures require admission, immediate orthopedic evaluation, or less urgent referral. [1, 2, 3] Mechanism of injury for most elbow fractures is direct elbow trauma or a fall onto an outstretched hand. Patients may experience pain, swelling, and decreased range of motion.
The elbow is a hinge joint composed of 3 bones: the ulna, the radius, and the humerus. The 3 main articulations of the elbow are (1) the humeroradial articulation, which is formed by the radial head and the capitellum of the humerus; (2) the humeroulnar articulation, which is formed by the ulnar notch and the trochlea of the humerus; and (3) the superior radioulnar articulation, which is formed by the proximal part of the ulna and the radius. All articulations are contained in one synovial-lined capsule, which typically encases a hemarthrosis following injury.
Two main movements occur at the elbow: flexion and extension, which occurs primarily at the humeroulnar articulation, and pronation and supination, which occurs primarily at the radioulnar articulation.
Fracture patterns vary widely due to the mechanism of injury as well as the age of the patient. Direct trauma or a fall onto an outstretched hand is responsible for most elbow fractures. Neurovascular injury is a common complication of elbow fractures. The brachial artery is the most commonly injured artery and is seen especially in supracondylar fractures. The median nerve is the most commonly injured nerve, which is often due to a displaced supracondylar humerus fracture.
Fracture patterns vary markedly among different age groups. Supracondylar fractures are the most common elbow fracture in children because of the relative strength of surrounding ligaments in comparison to bone. Radial head fractures are the most common elbow fracture in adults.
Diagnosis
A thorough neurovascular examination is vital in the assessment of elbow fractures because of the high incidence of neurovascular injuries with elbow fractures and the subsequent long-term complications with these injuries.
With supracondylar fractures, the incidence of anterior interosseous nerve injury is high, and specific muscle testing of flexion at the distal interphalangeal joint of the index finger should be performed. [4]
Patients often have decreased range of motion, and pain is present with pronation/supination of the forearm.
Edema and ecchymosis near the elbow may be evident.
Perform careful shoulder and wrist examinations with all elbow injuries.
Anteroposterior (AP), lateral, and oblique radiographs of the elbow adequately visualize most elbow fractures. To detect subtle elbow fractures, it is key to systematically view elbow films looking at certain aspects of the elbow. [3, 5, 6, 7]
In children who present to the ED with a painful arm, it may be difficult to identify a point of tenderness if the child is frightened and unable to identify the exact location of the pain. Common approaches include radiographic studies or empirically attempting reduction of radial head subluxation. Ultrasonography may be helpful in identifying a single fracture, allowing for a more focused area for radiographic study. Children with a normal ultrasound can safely undergo reduction of radial head subluxation. [8, 9, 10, 11, 12, 13]
In a systematic review and meta-analysis of the use of ultrasound for fractures of the upper extremity in children, by Tsou et al, ultrasonography had a sensitivity of 95%; specificity, 95%; positive likelihood ratio, 21.1; and negative likelihood ratio, 0.05. For elbow fracture, ultrasound had a sensitivity of 95%; specificity, 87%; positive likelihood ratio, 7.3; and negative likelihood ratio, 0.06. [9]
In general, an orthopedic consultant best handles decisions regarding reduction of significantly angulated and displaced fractures.
If neurovascular structures are compromised, the emergency physician may need to apply forearm traction to reestablish distal pulses.
If pulse is not restored with traction, emergent operative intervention for brachial artery exploration or fasciotomy is indicated.
Treatment
Emergency physicians need to do a thorough neurovascular examination as well as evaluate for concurrent injuries.
Provide adequate analgesia to achieve patient comfort in the ED. As with all fractures, address adequate outpatient analgesia, especially during the first few days. Acetaminophen, with codeine or hydrocodone, may be appropriate treatment.
Proper immobilization for the various types of elbow fractures is indicated.
Open fractures require extensive irrigation and appropriate prophylactic antibiotics, such as cefazolin and gentamicin. Displaced supracondylar fractures require surgical intervention and continual monitoring of neurovascular status.
Assess whether the patient needs orthopedic evaluation in the ED or admission to the hospital for observation, or determine if discharge and follow-up with an orthopedic surgeon is adequate.
All elbow fractures should be referred for orthopedic follow-up. Urgent orthopedic consultation in the ED is required if an open fracture or an open joint is suspected and if the injury poses a significant risk of neurovascular injury such as a displaced supracondylar fracture.
Supracondylar fracture
Refer patients with nondisplaced fractures to an orthopedist within 24 hours to evaluate and recheck neurovascular status.
In children, the most common type of elbow fracture is supracondylar humerus fracture (60-70% of fractures). Emergent operative management is necessary in those patients who have a pulseless white (dysvascular) hand that is associated with a displaced supracondylar humerus. Vascular compromise has been reported in 3-19% of patients, which can result from complete transection, kinking of the artery with reduced blood flow, thrombosis, intimal tear, arterial contusion or spasm, entrapment of the vessel within the fracture site, or traumatic aneurysm of the brachial artery with subsequent thrombus formation. [14]
In a study of 54,262 children with a distal forearm fracture, only 0.8% had an associated elbow injury, but 48.2% of the elbow injuries were supracondylar fractures of the humerus. [15]
Upon dissipation of edema, apply a long-arm cast that holds the elbow in 90° of flexion for approximately 6 weeks.
Radial head and neck fractures
For uncomplicated fractures, begin range-of-motion exercises within 3-7 days to reduce the risk of permanent loss of motion from elbow joint contracture.
Intra-articular fractures, which may require radial head excision or fixation, should be seen by an orthopedist within 1 week for definitive management.
Radial head fractures have an annual incidence of 2.5-2.8 per 10,000 people, [16, 17, 18] which is approximately a third of all elbow fractures. In a study of 23 patients, by Malahias et al, in whom there was a clinical suspicion of radial head fracture in the ED, ultrasound examination had an 83.3% sensitivity, 60% specificity, 88.2% positive prognostic value, and 50% negative prognostic value. [11]
In children, radial neck fractures may account for 8% of elbow fractures . In a retrospective study of 70 patients with acute radial neck fractures, Kong et al found that circumventing sedation in the ED and, instead, splinting for a planned surgical intervention may be a more efficient treatment method for radial neck fractures in patients who present to the ED more than 24 hours after injury and/or have angulations of 60º or more. [19]
Olecranon fracture
Nonoperative fractures (minimally displaced with an intact extensor mechanism) can be treated with a splint and range-of-motion exercises within a few weeks.
Extra-articular Fracture Patterns
Intercondylar fractures
Intercondylar fractures occur when the condylar fragments are separated. (See the image below.)
They are much more common in adults than in children. Any distal humerus fracture in adults is more likely to be intercondylar than supracondylar.
The mechanism is force directed against the posterior elbow, such as a fall onto a flexed elbow, driving the olecranon against the humeral articular surface separating the condyles.
Fractures are often a T or Y shaped fracture of the distal humerus.
Treatment is often complicated and requires anatomic reduction either open or closed. [20]
Supracondylar fractures
The supracondylar fracture is the most common pediatric elbow fracture (60%), with the average age of 6.7 years and rarely seen after age 15 years. [21] (See the image below.)
Complications include injuries to nerves (the median, radial, and anterior interosseous nerves are the most commonly injured).
Most deficits are neurapraxias that resolve with conservative management
Motor function usually returns in 7-12 weeks, and sensory function usually in 6 months. [22]
Vascular injuries should always be suspected with supracondylar fractures.
Ten percent of children have temporary loss of the radial pulse because of swelling and not direct arterial injury. [1]
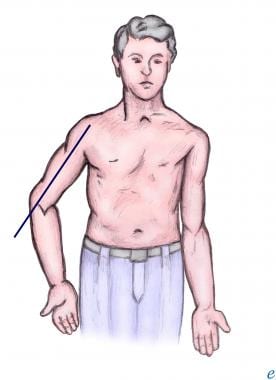
The most common complication for supracondylar fracture is cubitus varus or “gunstock deformity,” which is a loss of the carrying angle and results in more of a cosmetic disability than a functional one (see the image below).
Although rare (< 0.5%), the most serious complication is Volkmann ischemic contracture due to postfracture swelling, producing increased pressure in the forearm compartment and leading to muscle and nerve necrosis and eventual replacement by fibrotic tissue that causes contracture. [23]
In general, an orthopedic consultant best handles decisions regarding reduction of significantly angulated and displaced fractures.
If neurovascular structures are compromised, the emergency physician may need to apply forearm traction to reestablish distal pulses.
If pulse is not restored with traction, emergent operative intervention for brachial artery exploration or fasciotomy is indicated.
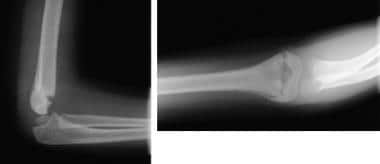
In children, nondisplaced, nonangulated fractures can be splinted (elbow in 90° of flexion); angulated fractures require reduction and splinting; and displaced fractures (see the image below) require reduction and percutaneous pinning on an urgent basis within 12-24 hours. In adults, supracondylar fractures generally require surgery.
Extension-type
Ninety-five percent of supracondylar fractures are of the extension-type and are displaced posteriorly because of an extension force.
-
Type I fractures - Undisplaced
-
Type II fractures - Displaced with posterior cortex still intact
-
Type III fractures - Displaced with both anterior and posterior cortex disrupted
Management of type I fractures consists of immobilization with the elbow in flexion, while type II and III are generally treated by closed reduction followed by pin fixation.
Type III fractures have significant displacement and have a high incidence of neurovascular injury and therefore require urgent orthopedic consultation in the ED.
Open reduction is reserved for vascular insufficiency with a probable entrapped brachial artery in the fracture site or an irreducible fracture.
Flexion-type
Five percent of supracondylar fractures are of the flexion-type and have anterior displacement due to a flexion force.
The mechanism usually involves direct anterior force with anterior displacement of the distal fragment.
Open fractures are relatively common because of the direct force.
-
Type I fractures - Undisplaced
-
Type II fractures - Displaced with anterior cortex still intact
-
Type III fractures - Displaced with both anterior and posterior cortex disrupted and distal fragment migrants anteriorly and proximately
Treatment of type I fractures is simple immobilization in the flexed position.
Treatment of type II and III fractures should be referred to an orthopedist emergently and is often reduced to an extension position and requires surgical management. [1]
Medial epicondyle fracture
Fractures of the epicondyles are considered extra-articular.
Medial epicondyle fractures are usually in children as an avulsion type injury (see the image below).
Mechanisms include posterior elbow dislocation, throwing a baseball (Little League elbow), or a direct blow.
Edema and pain over the medial elbow is common.
Nondisplaced or minimally displaced medial epicondyle fractures are treated nonoperatively.
Fragment displacement greater than 1 cm or valgus instability is often treated with internal fixation.
Rarely, entrapment of the medial epicondyle can occur between the trochlea and the coronoid process of the ulna; this can be mistaken for the ossification center of the trochlea.
ED management consists of immobilization of the forearm in flexion and pronation and the wrist in flexion.
Lateral epicondyle fracture
Lateral epicondyle fracture is very rare and is usually due to an avulsion fracture.
Fracture of the lateral humeral epicondyle can be mistaken for the radiolucency of the epiphysis. [24]
Treatment is immobilization with the elbow flexed to 90º and the forearm in supination. [24]
Medial condyle fracture
Medial condyle fracture is rare and is usually found in children.
The mechanism is a fall on outstretched hand or excessive valgus stress.
This injury is often confused with medial epicondyle fractures.
Minimally displaced fractures are usually casted, whereas fractures with greater displacement usually require open or closed reduction with pin fixation. [24]
Lateral condyle fracture
Lateral condyle fracture is usually found in children and is the second most common pediatric elbow fracture. [25] (See the image below.)
The mechanism is a blow to the lateral elbow or from varus stress.
Minimally displaced fractures are usually casted, whereas fractures with greater displacement usually require open or closed reduction with pin fixation. [25]
Intra-articular Fracture Patterns
Trochlea fracture
Isolated trochlea fractures are rare and are usually associated with other elbow injuries.
Nondisplaced fractures are usually managed with a posterior splint, whereas displaced fractures require surgical management. [24]
Capitellum fracture
Isolated capitellum fractures are rare as they often occur in posterior elbow dislocations or with radial head fractures.
They are usually due to a fall on an outstretched hand.
Surgical repair is often indicated.
Radial head fractures
Radial head fracture is the most common of all fractures of the elbow and associated injuries are common. See the image below.
The mechanism is usually a fall onto an outstretched hand.
Radial head fracture is characterized by point tenderness at the radial head (located along the lateral aspect of the elbow) and pain with pronation/supination.
A specific associated injury, the Essex-Lopresti lesion occurs when the radial-ulnar interosseous membrane is disrupted, causing distal radioulnar joint dissociation.
Careful examination of radiographs is important because fractures may be subtle.
For nondisplaced fractures, a sling with the elbow in flexion is usually adequate.
With displaced radial head fractures, patients can be placed in a posterior long-arm splint with the elbow in 90° of flexion and the forearm in full supination and placed in a sling for comfort.
Bipolar radial fractures have been reported involving simultaneous fracture of the distal radius and the radial head. This fracture pattern can lead to radial shortening and treating the wrist before the elbow may be advisable. [26]
Olecranon fractures
The mechanism is usually a direct blow or a fall onto an outstretched hand. See the image below.
The fracture line is usually transverse, passing into the trochlear notch. [24]
Patients demonstrate an inability to extend the elbow actively, along with point tenderness at the olecranon.
Ulnar nerve injury is common.
Patients can be placed in a well-padded, long-arm posterior splint with the elbow in 70° of flexion and the forearm neutral with respect to pronation/supination.
Nondisplaced fractures are usually managed conservatively, whereas all others often require surgical repair.
Prognosis
Supracondylar fracture
Children: Undisplaced fractures and properly managed displaced/angulated fractures result in no long-term functional deficits.
Adults: Usually, range of motion decreases somewhat but without functional deficit.
Radial head fracture
Usually, no functional loss occurs with nonoperative treatment.
Olecranon fracture
This fracture may result in loss of full extension but usually restores strength.
Olecranon fracture can be associated with post-traumatic arthritis of the elbow.
Most operative and nonoperative cases of olecranon fracture have a good outcome with no long-term deficits.
-
Intercondylar fracture.
-
Supracondylar fracture.
-
Displaced supracondylar fracture.
-
Medial epicondyle fracture.
-
Lateral condyle fracture.
-
Radial head fracture.
-
Olecranon fracture.
-
Anterior and posterior fat pads with radial head fracture.
-
Cubitus varus.