Practice Essentials
Knee dislocation is a relatively rare injury but an important one to recognize because coexistent vascular injury, if missed, often leads to limb loss. In addition, knee dislocation often presents in the context of multisystem trauma or spontaneous relocation, which makes detection more difficult. [1, 2, 3, 4, 5, 6, 7] The knee is a very stable joint generally requiring high-energy trauma to produce dislocation. At least 3 major ligaments typically rupture for dislocation to occur. Common mechanisms of injury include motor vehicle collisions, auto-pedestrian impact, industrial injuries, falls, and athletic injuries. [8, 9, 10, 11]
Patients with knee dislocation should undergo radiography and MRI, as well as angiography. The American College of Radiology has published the ACR Appropriateness Criteria for knee trauma to rate the appropriateness of imaging and treatment procedures. [12] Plain radiographs are recommended post reduction and prior to any provocative ligamentous stressing. [7, 9]
Although knee dislocations are considered rare injuries, they are considered surgical emergencies because of potential neurovascular complications. The Nationwide Inpatient Sample identified 2175 patients who had a knee dislocation between 2005 and 2013 in the United States, and a diagnosis of popliteal artery injury was documented in 210 (9.7%) patients. [13]
The National Trauma Data Bank identified 6454 knee dislocations between 2010 and 2014. A vascular examination was performed in 29%, with a vascular injury documented in 15% and a a vascular procedure performed in 10.8%. Associated fractures were identified in 41.4%, and open injuries in 13.6%. Neurologic injury was documented in 6.2%, compartment syndrome in 2.7%, and amputation in 3.8% (>50% had vascular injury). Death was noted in 2.8%. [14]
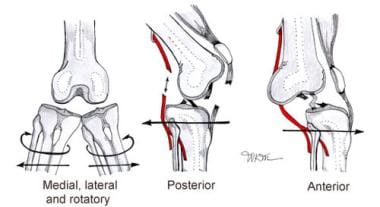
(See the images below.)
The positional classification system was developed by Kennedy and describes 5 major types of positional dislocation: medial, lateral, rotatory, posterior, and anterior. The anatomical classification system was developed by Schenck and modified by Wascher. It describes the injury by its ligamentous/anatomical involvement. [15, 8, 16]
Most often, the affected limb has a gross deformity of the knee with swelling and immobility, but up to 50% of knee dislocations are reduced by the time of ED presentation and may not be obvious.
Immediate and short-term complications include popliteal artery injuries, popliteal vein injury, common peroneal nerve injuries, ligamentous injury, acute compartment syndrome, and deep venous thrombosis. [17, 13]
Diagnosis
it is important to obtain radiographs prior to ligamentous stressing to avoid promoting fracture displacement. [18]
A careful vascular examination is required. For the EM physician, it is important to recognize that vascular examination findings may be normal in the presence of significant popliteal artery injury [19, 20, 13] and that some combination of further investigation/observation is warranted in all knee dislocations. This may be different for each institution and/or each surgeon and should be decided on a case-by-case basis in conjunction with the vascular consult.
Treatment
Prehospital personnel should splint the extremity and provide rapid transport to a medical facility.
Perform field reduction for patients with evidence of vascular compromise.
Do not delay reduction in limbs with obvious vascular impairment.
After adequate sedation, longitudinal traction will relocate the majority of knee dislocations.
All knee dislocations, regardless of emergent revascularization needs, should be admitted for serial perfusion checks.
Always consult both orthopedic and vascular surgeons. Many patients have significant vascular injury requiring surgical revascularization, and all patients will at least require admission for serial vascular checks and further surgical stabilization consideration.
Historically, conventional arteriography was recommended for all cases of knee dislocation, and though it remains the criterion standard for popliteal artery evaluation, there is growing debate over its universal application. Vascular assessment with the ankle-brachial index, duplex sonography, and/or CT angiography is changing this paradigm, with an increasing number of popliteal injuries being managed nonsurgically (generally those that show no significant thrombosis at 48-72 hr). Many surgeons thus argue that arteriography should not be routine and that case-by-case utilization of other imaging modalities combined with vigilant observation is sufficient.
Time is of utmost concern, as vascular repair delayed more than 8 hours after injury carries an amputation rate of greater than 80%. In contrast, operative vascular repair within 8 hours of injury yields a limb-salvage rate of 80%.
The repair of coexistent popliteal vein injury is controversial. Fasciotomy is recommended after vascular repair, as severe swelling and development of compartment syndrome are common in the postoperative phase.
Operative repair of nerve injury remains controversial, as a poor prognosis is common with both operative and nonoperative care.
Operative ligamentous repair is recommended by most authors, as functional results are better than those of nonoperative care, but determining the ideal timing of this intervention is complex and is a decision best left to the orthopedist.
Patients considered for transfer should have undergone emergency reduction of the knee dislocation. Since time is crucial in salvaging the limb after a vascular injury, transfer should be initiated only if vascular consultation and/or evaluation are not available at the transferring institution or if an arteriogram has been performed and results are normal.
Prognosis
When treated expeditiously and appropriately, 60-70% of patients will have a painless, stable knee. Of the remaining patients, one half will eventually have reasonable function, while the other half will have a chronically unstable and painful knee. [8]
A systematic review has demonstrated that some level of sport participation is possible after multiligament knee injuries (MLKIs) for more than half of patients, but returning to preinjury levels of sport after surgical treatment is low, at just 22% to 33%. [21]
A study of 88 traumatic knee dislocations found those who were injured at a higher velocity were more likely to have additional injuries. Dislocations that occurred at a lower velocity were shown to have better overall outcomes, as did dislocations that occurred in isolation. [22]
In a study by Woodmass et al of knee functional outcomes of 62 patients with multiligament knee injuries that occurred in polytrauma or in isolation, patients who sustained injury as a result of polytrauma demonstrated significantly lower functional scores after reconstruction. This was despite restoration of similar knee stability and range of motion. [23]
-
Types of knee dislocation.
-
Posterior knee dislocation.
-
Lateral knee dislocation (before reduction).
-
Open knee dislocation.
-
Lateral knee dislocation after reduction.