Practice Essentials
The human body has the ability to adjust to increases in ambient pressure, to a limit. However, the increased pressure increases the partial pressures of the gases that are inspired. A number of effects can occur. Toxicity to oxygen or nitrogen, or contaminants, have deleterious effects. A scuba (self-contained underwater breathing apparatus) diver can mitigate these effects by staying within established time parameters to avoid these toxicities. Those with advanced technical training use specialized mixtures to avoid these toxicities. Even when staying within the parameters, or perhaps using the specialized gases, issues can still occur and cause injury. In addition, the sudden or too rapid decrease in pressure (ie, decompression) can have a number of ill effects. Some relate to the gross expansion of gas in the usual gas-containing cavities and organs in the body. The result can be dysbarism. Other effects are due to the expansion of microscopic gas particles within the tissues of the body. This is decompression sickness (DCS). Also see Dysbarism.
Healthcare professionals worldwide, regardless of specialty, need to be aware of the ill effects of exposure to increased pressure. The ability to travel great distances relatively quickly, the increasingly unusual areas being dived, along with the delay in onset of symptoms can find a person suffering from DCS showing up in a medical setting seemingly quite far from bodies of water. DCS symptoms can be of rapid onset, straightforward, or insidiously mild and delayed. Healthcare practitioners need to consider activity in the days prior to any medical visit, and be aware of the issues and nuances of diving injuries, every time they encounter a patient so that they do not miss the opportunity to properly treat these patients. The encounters may not even be an official medical visit. It could be while traveling or on vacation.
If a patient has DCS, immediate 100% fraction of inspired oxygen (FIO2) along with hydration, either oral or intravenous isotonic crystalloids, is an important first step in mitigating the effects. The patient needs referral to a hyperbaric oxygen (HBO) facility experienced in treating DCS. When in doubt, consult a diving medicine specialist, or the Divers Alert Network worldwide emergency number (+1-919-684-9111) for advice and referral. Proper timely management of these injuries yields high rates of success. Missing them can be catastrophic.
Background
Although decompression sickness (DCS), a complex resulting from changed barometric pressure, includes high-altitude–related and aerospace-related events, [1] this article focuses on decompression associated with the sudden decrease in pressures during underwater ascent, usually occurring during free or assisted dives. People involved with tunneling projects, in submarines during emergencies, and in breath-hold free diving may also experience the physiologic effects of decreased pressure brought on by such ascents.
Since 4,500 BCE, humans have engaged in free (breath-hold) diving to obtain food and substances from shallow ocean floors at depths of 100 ft or more. The 2007 record-setting breath-hold unlimited dive of Herbert Nitsch to 702 ft (214 m) attests to this human feat. [2] However, as a testament to physical limitations, in 2012, when he tried to break his own record by diving to 819 ft (250 m), he suffered a narcosis blackout on ascent, causing a violation of his safety and decompression plan. As a result, he suffered a severe type II neurologic DCS that ended his record-breaking career. [3] Humans began experimenting with crude diving bells as early as 330 BCE. These bells submerged containing only air. In 1690, the first diving bell with a replenishing air supply was tested. The first crude underwater suit dates back to 1837, and helium was first used in place of nitrogen in 1939.
All these early diving methods required a physical connection to a support platform or boat. The Aqua-Lung, developed by Cousteau and Gagnon, and the submarine escape appliances, developed by Momsen and Davis, in the 1930s, were forerunners of the self-contained underwater breathing apparatus (scuba), which frees divers from the limitations of tethering.
The increasing popularity of scuba diving and the growth of commercial diving have increased the frequency of deep-pressure injuries. Even in regions far from coasts, individuals are diving in quarries, lakes, rivers, and caves. In addition, the ability to travel rapidly between areas of disparate altitudes in a matter of hours (including the exacerbation caused by decreased pressures in flight) increases the chance of experiencing decompression injuries, and of physicians far from water bodies encountering them. Emergency physicians, all physicians, and other advanced healthcare providers worldwide should know the physiologic effects and management of DCS.
In summary, acute DCS is a purely clinical diagnosis that requires a fair amount of clinical suspicion to avoid missing cases. Most of the time the diagnostic yield is improvement with hyperbaric oxygen (HBO) therapy. No specific tests exist for DCS. When diving is involved, consider determining whether the patient has any pressure-related injuries. Obtain baseline diagnostic studies, but these have no bearing on initial management. They may be useful in the differential diagnosis while undergoing HBO therapy, especially if there is no improvement with HBO. They may also be useful in expanding the knowledge base about this disorder.
Special concerns
Diving while pregnant is not recommended because of unknown effects of nitrogen diffusion across the maternal-placental membrane. The fetus is not believed to be protected from decompression problems and is at risk of malformation and gas embolism. However, normal pregnancies have been reported even after repetitive dives. [4]
While there is no absolute lower age limit, children younger than 12 years should not dive. Although one limited study found no venous bubble formation after a routine, single, shallow dive, [5] another, in persons aged 12-14 years, documented bubbling after 25-minute dives to 10 m (32 ft). [6] Diving can be a dangerous activity that requires respect, common sense, and absolute adherence to safety rules. The inherent nature of children to be distracted and have no sense of mortality or time makes it difficult for them to dive safely without close supervision.
Advanced age brings increased medical problems. As with any physical activity, one should seek the advice and recommendations of a physician familiar with diving medicine.
Most divers use a compressed air source. Dive shops usually refill dive tanks. The equipment is typically a gasoline-powered air compressor that uses filtered ambient air. An improper setup or malfunctioning equipment may compress carbon monoxide from exhaust fumes (or other gases nearby) along with the air. This is a recognized danger in the diving industry. Filling stations should have safeguards in place; however, the potential for injury still exists. According to the Dalton law, even small amounts of carbon monoxide in the tanks have higher partial pressures at depth that may exacerbate clinical effects.
Because the symptoms of carbon monoxide poisoning (eg, dyspnea, headache, fatigue, dizziness, visual changes, and unconsciousness) can mimic DCS or arterial gas embolization (AGE), differentiate these conditions by looking for carbon monoxide specifically with co-oximetry. Failure to recognize carbon monoxide poisoning is not a serious omission as long as the patient is recognized as having a diving injury. The hyperbaric treatment of DCS and AGE is also the treatment of choice for carbon monoxide poisoning. For more information on this topic, please see the article on Carbon Monoxide Toxicity.
Two other situations deserve mention. The first is related to the use of special "technical diving" gases such as Trimix (a combination of oxygen, nitrogen, and helium). The other situation relates to breath-hold diving (without scuba tanks). In the past, a breath-hold dive was simply a free dive from the surface without supplemental air.
Technical diving gases
There is a practical limit to the use of compressed air in scuba diving of around 132 ft (40 m, 4 atm) where the bottom times are so short (or actually nonexistent using standard tables) and the risk of nitrogen narcosis is high. Since many interesting sites, such as wrecks, are deeper than that, many divers have started using a Trimix that lowers the nitrogen load to avoid narcosis, decreases the oxygen content to avoid toxicity, and replaces the two with helium that also is a lighter gas.
Depending on the goal depth, multiple tanks with different mixes for different depth ranges are carried. This is a highly technical and riskier activity.
Even with the Trimix, the limit is still fuzzy as the overall gas density increases. This increases the work of breathing and thus respiratory fatigue. Added to the additional load of general physical exertion, a situation of hypercapnia (increasing carbon dioxide in the bloodstream) can ensue that causes worsening of the overall fatigue. If not corrected by ascending, death can occur.
Trimix has been used in HBO treatment to shorten treatment courses with success.
Breath-hold diving
The average person is limited by his or her physical prowess for how deep he or she could go, or the length of time he or she could stay under. Neither was a major concern except in the circumstance of forced hyperventilation thinking this would help just before the dive. The result here could be hypoxia with loss of consciousness before the hypercapnic, elevated carbon dioxide, need to take a breath.
The addition of fins increased the depth and distance but again not to a concerning level. In recent years, oversized fins have appeared on the market, as have motorized underwater scooters. Both of these have allowed much greater depths in the free dives and can allow more rapid ascent and then immediate dive again. Professional and recreation spear fisherman, especially in tournaments, are now achieving depth and underwater times where they can start accumulating nitrogen loads and with the rapid ascents, DCS has been reported.
Another group of note are the extreme-depth unlimited free divers. They use a weighted sled to achieve record depths measured in the several hundreds. The combination of extreme depth and 5- to 7-minute times involved allow sufficient nitrogen loads that again can result in DCS.
The risk is even greater in those that are preparing for a competition where in the course of a day they can have repeated weighted free dives to increasing depths with limited surface intervals. Frequent Valsalva on descent to equalize pressure also can unmask a previously unknown patent foramen ovale (PFO) or atrial septal defect (ASD) and allow neurological DCS. Morbidity and mortality is increasing in these extreme free divers who keep pushing physiologic limits to dangerous extremes due to reasons elucidated above plus various barotraumas causing disabling symptoms.
Pathophysiology
Gas laws
Changes in pressure affect only compressible substances in the body. The human body is made primarily of water, which is noncompressible; however, the gases of hollow spaces and viscous organs, and those dissolved in the blood, are subject to pressure changes. Physical characteristics of gases are described by the following four gas laws, which quantify the physics and problems involved in descending under water.
Boyle law
For an in-depth discussion on the Boyle law, please see the article on Dysbarism.
Dalton law
Pt = PO2 + PN2 + Px
(Pt = total pressure, PO2 = partial pressure of oxygen, PN2 = partial pressure of nitrogen, Px = partial pressure of remaining gases)
In a mixture of gases, the pressure exerted by any given gas is the same as the pressure the gas would exert if it alone occupied the same volume. Thus, the ratio of gases does not change, even though the overall pressure does. The individual partial pressures, however, change proportionally.
Dalton's problem
As an individual descends, the total pressure of breathing air increases; therefore, the partial pressures of the individual components of breathing air have to increase proportionally. As the individual descends under water, an increasing amount of nitrogen dissolves in the blood. Nitrogen at higher partial pressures alters the electrical properties of cerebral cellular membranes causing an anesthetic effect termed nitrogen narcosis. Every 50 ft (15 m) of depth is equivalent in its effects to one alcoholic drink. Thus, by 150 ft (46 m), divers may experience alterations in reasoning, memory, response time, and other problems such as idea fixation, overconfidence, and calculation errors. Even when no signs of nitrogen narcosis are noted, divers may significantly overestimate diving time during deep dives. See the image below.
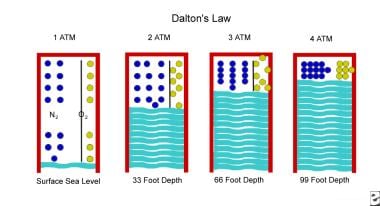 Illustration of Dalton gas law. As an individual descends, the total pressure of breathing air increases and the partial pressures of the individual components have to increase proportionally. Nitrogen at higher partial pressures alters the electrical properties of cerebral cellular membranes, causing an anesthetic effect. Oxygen at higher partial pressures can cause CNS oxygen toxicity.
Illustration of Dalton gas law. As an individual descends, the total pressure of breathing air increases and the partial pressures of the individual components have to increase proportionally. Nitrogen at higher partial pressures alters the electrical properties of cerebral cellular membranes, causing an anesthetic effect. Oxygen at higher partial pressures can cause CNS oxygen toxicity.
Descending also increases the amount of dissolved oxygen. Breathing 100% oxygen at 2 atm (33 ft, 10 m) may cause CNS oxygen toxicity in as few as 30-60 minutes. At 300 ft (91 m), the normal 21% oxygen in compressed air can become toxic because the partial pressure of oxygen is approximately equal to 100% at 33 ft (10 m). For these reasons, deep divers (usually professional or military but increasingly sport divers as well) use specialized mixtures that replace nitrogen with helium and allow for varying percentages of oxygen depending on depth.
Henry law
%X = (PX / Pt) X 100
(%X = amount of gas dissolved in a liquid, PX = pressure of gas X, Pt = total atmospheric pressure)
At a constant temperature, the amount of gas that dissolves in a liquid with which it is in contact is proportional to the partial pressure of that gas (ie, a gas diffuses across a gas-fluid interface until the partial pressure is the same on both sides).
Henry's problem
With increasing depth, nitrogen in compressed air equilibrates through the alveoli into the blood. Over time, increasing amounts of nitrogen dissolve and accumulate in the lipid component of tissues. As an individual ascends, a lag occurs before saturated tissues start to release nitrogen back into the blood. This delay creates problems. (See the image below.)
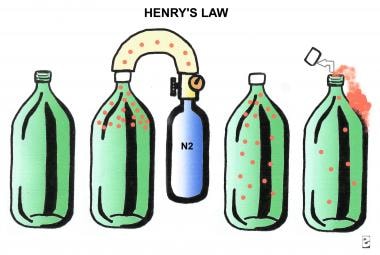 Illustration of Henry gas law. If nitrogen is added to a bottle, it diffuses into and equilibrates with the fluid. With a sudden release of pressure (decreased), such as when an individual ascends rapidly, a lag occurs before nitrogen can diffuse back to the nonfluid space. This delay causes nitrogen to bubble while still in the fluid.
Illustration of Henry gas law. If nitrogen is added to a bottle, it diffuses into and equilibrates with the fluid. With a sudden release of pressure (decreased), such as when an individual ascends rapidly, a lag occurs before nitrogen can diffuse back to the nonfluid space. This delay causes nitrogen to bubble while still in the fluid.
When a critical amount of nitrogen dissolves in the tissues, ascending too quickly causes the dissolved nitrogen to return to its gas form while still in the blood or tissues, causing bubbles to form. Further reductions in pressure while flying or ascending to a higher altitude also contribute to bubble formation. The average commercial airline cabin pressurizes to only 8,000 ft (2,438 m) to save fuel costs. If a person flies too soon after diving, this additional decrease in pressure may be enough to precipitate bubbling. If the bubbles are still in the tissue, they can cause local problems; if they are in the blood, embolization may result. (See the discussion under Prevention for more information.)
Charles law
For an in-depth discussion on the Charles law, please see the article on Dysbarism.
Bubbles
When bubbles are inside the body, such as a trapped gas bubble in the intestine or stomach, the results are uncomfortable. This is even truer for divers. The effects of trapped gas in various body cavities are discussed in Dysbarism. Microscopic bubbles, in particular those made of nitrogen that cause decompression sickness (DCS), are discussed here.
Not only does the quantity and size of the bubbles matter, but the type of reactions these bubbles cause is important as well. Location is also important. If bubbles end up in the lung and are not too large, they simple get filtered and exhaled. However, if a right to left shunt is present, such as from a PFO, they bypass the natural filtering effect of the lungs and continue on to the brain or other organs. Nitrogen bubbles are believed to start as minute gas nuclei present before the dive, rather than from supersaturation of the blood and tissues that acts as the seed for large bubble formation. [7] All divers have bubbles. [8] However, few divers develop DCS. Thus, more than bubbles have to be involved. The presence of bubbles alone does not increase the risk of DCS. [9]
Microbubbles precede larger venous gas emboli. [10] These emboli can occlude blood flow in smaller vessels and cause direct ischemia and damage. Bubbles have also been found to alter vascular endothelium through adhesion-molecule-mediated endothelial activation, in addition to activating platelets. In neurological tissue this leads to focal ischemia. The TREK-1 potassium channel mediates this effect in a neuroprotective manner. [11, 12] It was not clear whether the contact of the bubbles with the vascular epithelium (causing damage and platelet response) or if there was a direct mechanism for platelet activation. A glycoprotein (GP)–IIb/IIIa inhibitor inhibited platelet aggregation, suggesting that there is a direct effect. [13]
Microparticles, 0.1- to 1-μm diameter vesicular structures [14] derived from vascular walls, have been found to increase 3.4 times with dives and decompression stress. The microparticles may result from oxidative stress (see the next paragraph). [15] They appear to activate neutrophils and interact with platelet membranes. [8, 16] Endothelial cells, blood platelets, or leukocytes shed microparticles upon activation and cell apoptosis (normal programmed cell death). In particular, the release of platelet microparticles could reflect bubble-induced platelet aggregation. This could be the cause of coagulation and thrombosis, thus interfering with blood flow. [17] Once the bubbles form they create a foreign body interface to which platelets then adhere. [18] In severe DCS significant decreases in platelet count have been documented. These decreases may someday be used as a marker for severity of injury. [19, 20] Microparticles bearing proteins CD66b, CD41, CD31, CD142, CD235, and von Willebrand factor were found 2.4- to 11.7-fold higher in the blood from divers with DCS compared with non-DCS divers. [14]
Endothelial nitric oxide synthase produces nitric oxide through the combination of arginine and oxygen. It is a powerful vasodilator that, through relaxation of smooth muscles, inhibits platelet aggregation and inhibits inflammation. The combination contributes to blood vessel homeostasis. The presence of nitric oxide may reduce bubble formation. [21, 22] However, the increasing partial pressure of oxygen at depth drives the reaction towards nitric oxide. Once the body’s natural processes for dealing with oxidizers, which this is, are overwhelmed, it yields an excess of oxidative excitatory neurotransmitters. [22] Nitrogen dioxide, a nascent gas nucleation site synthesized in some microparticles, initiates decompression inflammatory injury. [16] It is also an oxidizer that exists in equilibrium with dinitrogen tetroxide. [22]
Another contributor to inflammatory vascular reaction lies within the microparticles. Interleukin-1beta concentrations increase in response to high-pressure environments and continue to increase for 13 hours afterwards. This corresponds to vascular damage. Other inflammatory factors adhere to the exterior of the microparticles. The combination of inflammatory agents contributes to the vascular damage. [23]
There appears to be a relationship among bubbles, microparticles, platelet-neutrophil interactions, and neutrophil activation. However, exactly what that relationship is still remains obscure. [8, 24]
Simulated diving conditions with air and oxygen adversely affect cellular respiration through mitochondrial function in fibroblasts. [25]
Organ involvement associated with decompression sickness
As discussed in the section describing the Henry law above, a reduction in pressure while ascending at the end of a dive can release dissolved gas (principally nitrogen), from solution in the tissues and blood, consequently forming bubbles in the body.
DCS results from the effects of these bubbles on organ systems. The bubbles may disrupt cells and cause a loss of function. They may act as emboli and block circulation, as well as cause mechanical compression and stretching of the blood vessels and nerves. The blood-bubble interface may act as a foreign body interface, activating the early phases of blood coagulation and the release of vasoactive substances from the cells lining the blood vessels. [26] DCS is divided into three categories: (1) type I (mild), (2) type II (serious), and (3) AGE.
Type I decompression sickness
Type I DCS is characterized by one or a combination of the following: (1) mild pains that begin to resolve within 10 minutes of onset (niggles); (2) pruritus, or "skin bends," that causes itching or burning sensations of the skin; and (3) cutis marmorata.
Cutis marmorata, cutaneous DCS, is a rash that generally is widespread mottling and/or marbling of the skin or a papular or plaquelike violaceous (blue-red) rash. On rare occasions, skin has an orange-peel appearance. Cutis marmorata typically starts as an intense multifocal itching, then hyperemia develops, followed by the already-described purplish rash. [27] In the past, it was thought to be a benign disorder from bubble formation, with theories for its presence of vascular occlusion ranging from right-to-left shunt (eg, from a PFO), to supersaturation of subcutaneous fat tissues. [28] A newer theory is gas emboli amplification in cutaneous capillaries. [29, 30] One study reports a near 100% presence of PFO on contrast echocardiography. [31] However, similarities of this rash with livedo reticularis or livedo racemose (due to sympathetic overloads), along with a small number of divers with cutis marmorata who also have vague neurologic symptoms, has led to more recent theories of the rash being centrally mediated in DCS. [29, 31] Specifically, a newer hypothesized theory is for gas embolization of the brainstem affecting autonomic control of vasodilation and vasoconstriction. [31]
Lymphatic involvement is uncommon and typically causes painless pitting edema. The mildest cases involve only the skin or the lymphatics. Some authorities consider anorexia and excessive fatigue after a dive as manifestations of type I DCS.
Pain (the bends) occurs in most (70-85%) patients with type I DCS. Pain is the most common symptom of this mild type of DCS often described as a dull, deep, throbbing, toothache-type pain, usually in a joint or tendon area but also in tissue. The shoulder is the most commonly affected joint. The pain is initially mild and slowly becomes more intense. Because of this, many divers attribute early DCS symptoms to overexertion or a pulled muscle.
Muscle splinting causes decreased function. Upper limbs are affected about 3 times as often as lower limbs. The pain caused by type I DCS may mask neurologic signs that are hallmarks of the more serious type II DCS. Dysbaric osteonecrosis is a phenomenon that occurs in divers with high numbers of dives. This is a persistent problem, suggesting that the mechanisms involved in the disorder are not yet understood.
Cutaneous abnormalities, joint and muscular pain, and neurologic manifestations (covered in the next section) were the three most common symptoms. The initial symptoms started within 6 hours of surfacing in 99% of cases with an overall mean delay to onset of 62 minutes. The shorter the time to onset, the more serious the symptoms. [32]
Delineation of mild type I DCS symptoms and signs can be useful when considering treatment (refer to the later section on HBO therapy). General fatigue, nondermatomal distribution skin sensory aberrations, rash, pruritus, isolated limb pain (not symmetric), and subcutaneous edema that are not progressive out to 24 hours are all examples. It is important that there are no concomitant spinal or central neurologic symptoms or signs (see the next section on type II DCS for details). [33]
Type II decompression sickness
The following characterizes type II DCS: (1) pulmonary symptoms, (2) hypovolemic shock, or (3) nervous system involvement. Pain occurs in only about 30% of cases. Because of the anatomic complexity of the central and peripheral nervous systems, signs and symptoms are variable and diverse. Symptom onset is usually immediate but may occur up to 36 hours later.
Nervous system
The spinal cord is the most common site affected by type II DCS; symptoms mimic spinal cord trauma. Low back pain may start within a few minutes to hours after the dive and may progress to paresis, paralysis, paresthesia, loss of sphincter control, and girdle pain of the lower trunk. Patients with the worst outcomes (still having multiple neurological sequelae with less than 50% resolution after hyperbaric oxygen therapy) were those who had onset of symptoms within 30 minutes of surfacing. [34]
Vertebral back pain after a dive is a poor prognostic sign and can be a hallmark of spinal DCS with anticipated poor long-term outcome. [35, 36]
Dysbaric myelitis occurs in half of the cases of neurological DCS. Venous ischemia is the most likely cause. Bladder problems, such as neurogenic bladder, may be common in the acute phase of DCS, may be the primary presentation, and may be prolonged. Intraspinal pressure and perfusion appear to play important roles in the injury. Just as the cerebrum is contained in a confined, nonexpandable, space, so is the spinal cord. Decreases in blood pressure and/or increases in CSF intraspinal pressure can compromise circulation, thus increasing ischemic injury. Despite improvement in examination findings with treatment, it has been found that there can be significant cord damage as a result. Similar to intracerebral pressure monitoring and drainage, consideration should be given for similar intraspinal pressure monitoring and drainage. [37]
Pulmonary filtration protects the nervous system by stopping bubbles at the lungs. A shortcut, such as a PFO or ASD, can bypass this filtration. Additionally, hypoxia may open intrapulmonary anastomoses, thus also allowing venous bubbles to pass into arterial circulation. [38] This filtration is size dependent. Tiny bubbles, or microemboli, that escape entrapment and continue to the brain do not cause infarction. Normal cerebral circulation starts with the highly oxygenated arterial blood flowing through the gray matter where much of the oxygen is extracted. This less oxygenated blood then flows to the long draining veins that supply the white matter of both the cerebral medulla and the spinal cord. At this level, even small additional decreases of oxygen content by embolization can be enough to damage the blood-brain barrier and initiate a cascade that ends with axonal damage. The result can be perivenous syndrome. [39]
DCS can be dynamic and does not follow typical peripheral nerve distribution patterns. This strange shifting of symptoms confuses the diagnosis of differentiating DCS from traumatic nerve injuries. Neurological deficits after a spinal cord injury can be multifocal. Sensory and motor disturbances can present independently, often resulting in a situation of "dissociation." This dissociation is found in most cases of spinal cord DCS.
MRI studies have seemingly revealed arterial patterns of infarction in spinal DCS. [34]
Eyes
When DCS affects the brain, many symptoms can result. Negative scotomata, devoid of any lights or shapes, are the earliest symptom. Negative scotomata become positive after a few minutes.
Other common symptoms include headaches or visual disturbances, dizziness, tunnel vision, and changes in mental status. However, isolated diplopia, without other neurologic or ocular symptoms, is not consistent with DCS. Mask barotrauma caused a periorbital hematoma in one diver. Physical examination and CT scan of the orbits confirmed the diagnosis. [40]
Ears
Head and neck issues account for 80% of diving illnesses. Of these 65% involve the ears. [41] (Also, see Dysbarism.) Labyrinthine DCS (the staggers) causes a combination of nausea, vomiting, vertigo, and nystagmus, in addition to tinnitus and partial deafness. This alternobaric vertigo can be difficult to differentiate from dysbaric eustachian tube dysfunction. [42] A history of eustachian tube problems depicted by past otitis media, past eustachian tube dysfunction, and problems equalizing pressure in the ears during the dive is associated with an increased prevalence of alternobaric vertigo. [43, 44] In inner-ear DCS (IEDCS), vertigo was the major presenting complaint in 77-100%. Hearing loss occurred in 6-40% and a combination of both in 18%. Additional skin and neurologic symptoms were present in 15%. Symptoms occurred within 120 minutes of surfacing with a median delay of 20 minutes. [45, 46]
In contrast to this, in dysbaric barotrauma, vertigo was not found to be the presenting complaint, or a significant problem. Instead, those patients complained of tinnitus and hearing loss. For more on dysbarism in the ear, please see the article on Dysbarism.
A study of offshore professional divers found higher incidence of dizziness, vertigo, and ataxia than in nondiver controls. With an incidence range from 14-28%, 61% of the divers had prior DCS, mostly type I, which was found to correlate more than the total number of dives. [47]
The pathophysiology for IEDCS is believed related to a left to right shunt in the labyrinthine artery. [43] However, such a shunt should also cause cerebral symptoms that do not happen. The reason may lay with a difference in nitrogen washout in the inner ear compared to the brain. Experimental models suggest that the washout time for the inner ear is about eight times as long compared with the brain (half-times of 8.8 and 1.2 min, respectively). [48] However, more recent research has found a correlation between IEDCS and the presence of a patent foramen ovale; 74-82% of those who sought screening were found to have a right-to-left shunt from PFO (compared with up to 25-30% incidence of PFO in the general population). [41, 45, 46, 49, 50] The vestibular tissue is more vulnerable than the cochlea because the cochlea has greater blood flow, smaller volume, and faster gas washout. This decreases the time that it is vulnerable to arterial bubbles compared with the vestibular tissue. [51]
IEDCS was found to respond slowly to hyperbaric oxygen therapy and incomplete recovery was noted in most (90%). [41] Time/delay to hyperbaric recompression did not change the clinical outcome. Paradoxical AGE is also hypothesized. [46, 49]
Another condition to consider in the differential diagnosis of postdive dizziness is superior semicircular canal dehiscence. It is difficult to differentiate. A key feature is sound- or pressure-induced (Valsalva) vertical torsional nystagmus. A high resolution CT scan of the temporal bones identifies it if it is present. [52]
Lungs
Pulmonary DCS (the chokes) is characterized by the following: (1) burning substernal discomfort on inspiration, (2) nonproductive coughing that can become paroxysmal, and (3) severe respiratory distress.
This occurs in about 2% of all DCS cases and can cause death. Symptoms can start up to 12 hours after a dive and persist for 12-48 hours.
Circulatory system
Hydration status is affected by scuba diving. Mild dehydration has been found to occur in both the intra and extracellular compartments during deep dives. [53] Numerous influences play a role. First, many scuba divers engage in their sport in hot tropical environments. This naturally increases fluid requirements as the body works harder to keep itself cool. The same effect can occur in colder climates where the diver uses a heated dry suit. Scuba diving is a physically demanding activity and thus utilizes more fluids. The breathing gases, whether they are compressed air or technical gas mixtures, are also dry thus robbing the body of moisture in the exhaled gases.
Most people underestimate their fluid requirements in these situations. Add to this the drying effect of commercial airliner altitude pressures and the vacationer's preferred beverages being alcoholic. The average diver is thus set up for the possibility of significant dehydration. In small arteries, the effects of decompression stress are amplified in a dehydrated state. [54]
A study of simple hematocrits after a single tropical dive found increases that were statistically significant and greater with the depth of the dive. [55] While the changes were overall small, they do highlight the drying effect of diving. Another study found significant increases in hematocrit with a median of 43 (the range was up to 60). They attempted to correlate more significant increases (to above 48) with neurological DCS. They did find this association in women but not in men. [56] In addition, a swine study found that dehydration significantly increased the risk of severe cardiopulmonary and CNS DCS and of overall death. [57] A human study also found a significant decrease in venous bubble formation with predive hydration. [58] The increase in hematocrit is also associated with capillary leakage. The bubbles can alter the blood vessel walls, allowing protein and fluid leakage. It can becomes so severe as to cause hypovolemic shock. [59]
Hypovolemic shock is commonly associated with other symptoms. For reasons not yet fully understood, fluid shifts from the intravascular spaces to the extravascular spaces. Treat the signs of tachycardia and postural hypotension with oral rehydration if the patient is conscious, or intravenously if the patient is unconscious. The treatment of DCS is less effective if dehydrated.
Thrombi may form because of the activation of the early phases of blood coagulation and the release of vasoactive substances from cells lining the blood vessels. [26] The blood-bubble interface may act as a foreign surface, causing this effect. Bubble formation in DCS has been believed not only to cause mechanical stretch or damage and blockage of blood flow by embolization but also to act as a foreign body and to activate the complement and coagulation pathways creating a thrombus. [60, 61, 62] Recent studies appear to leave this concept unresolved. Some of the studies' authors indicate that they have supported this hypothesis, while others could not find a correlation with degree of injury.
To assist with studying of DCS, classify type A for the more serious neurologic DCS (strokelike). Type B is for the mild, or doubtful, neurologic symptoms. Studies suggest that the etiology is different for the two types and not explained by patent foramen ovale with left to right shunting. [63, 64]
Right-to-left shunt
PFO or congenital ASD also come into play in DCS. [65, 66] These defects allow bubbles to pass from right to left circulation, bypassing the screening effects of the pulmonary circulation. This correlates with a higher prevalence of high spinal cord and head (brain)/neck DCS injury. This was more profound when a procedural violation during the dive led to DCS. As mentioned earlier, a significant incidence of IEDCS is associated with right-to-left shunt. [45, 46, 48, 49, 50] ASDs of greater than 10 mm were associated with shunt-mediated decompression injury/DCS. This accounts for only 1.3% of the general population. [67] Patients with only a large PFO had an increased risk of DCS when decompression rules were not violated. Smaller defects usually required a diving violation creating the environment where there are a large number of venous gas bubbles, delayed tissue nitrogen desaturation, and increased right atrial pressure from Valsalva-type straining. [68]
Although the overall prevalence of PFO in the general population is significant (about 15-30%), [69, 70, 71, 72] the prevalence of serious type II DCS is low. In a group treated for DCS, 63% had a right-to-left shunt through agitated saline contrast transcranial Doppler ultrasound examination. In the control group, only 32% had the anomaly. Patients with cerebral, spinal, inner ear, or cutaneous DCS had a higher incidence of the shunt. There is no recommendation for routine screening of general (never had DCS) divers for PFO or ASD. [73] However, in the face of a serious DCS episode, consider the evaluation, for a right-to-left shunt, to guide recommendations for future diving. Serious active divers and professionals might consider routine screening for either atrial defect (see Prevention). [74] Two women with breast pain after diving were found to have PFO. [75]
In two samples of divers, of which about half suffered significant DCS on ascent, a patent foramen ovale was found in 50-53% of those with DCS. All symptomatic divers had the neurological form of DCS from paradoxical embolization. In the other half, which did not suffer DCS, only 1 (statistically 8%) was found to have a PFO. Of note, only 1 out of 4 divers with serious DCS received any PFO screening. All divers who suffer neurological DCS; frequent divers in general, whether amateur or professional; and especially extreme divers; should be considered for screening for PFO or ASD. This should be done with agitated saline contrast echocardiogram testing (see later section on Diagnostic Studies). [71, 76, 77] Another survey of health issues in divers had a cohort of 268 respondents. Of the 27 who reported DCS, 25 had a not-known PFO. [78]
Another interesting feature of patent foramen ovale is the relationship with migraines, in particular those with aura. In limited studies, approximately 48% of migraine patients with aura had a PFO. Interestingly, for many years HBO physicians had noted that many patients with neurologic DCS had a prior history of recurrent migraines. When a group of divers was specifically studied for this condition, results showed that 47.5% of divers with a large right-to-left shunt at rest from PFO who had been victims of DCS had a history or migraines with aura. [79, 80]
The diagnosis of the shunt from an atrial defect is through transcranial Doppler scanning, after an injection of agitated sterile saline through the antecubital vein to create minute bubbles, and scanning at rest and with Valsalva. This was found more sensitive than transesophageal echocardiography using similar provocative maneuvers. Transcranial Doppler screening was found to have a negative predictive value of 100% and a positive predictive value of 92%. [81, 82] Therefore, a reasonable conclusion is that divers with a history of migraine, especially those with aura, should consider specific screening for PFO or ASD (see later section on Prevention).
Once found, patent foramen ovale closure in continuing divers appears to prevent symptomatic (major DCI) and asymptomatic (ischemic brain lesions) neurological event during long-term follow-up (see later section on Prevention). [83]
Arterial gas embolization
Pulmonary overpressurization (see article on Dysbarism) can cause large gas emboli when a rupture into the pulmonary vein allows alveolar gas to enter systemic circulation. Gas emboli can lodge in coronary, cerebral, and other systemic arterioles. These gas bubbles continue to expand as ascending pressure decreases, thus increasing the severity of clinical signs. Symptoms and signs depend on where the emboli travel. Coronary artery embolization can lead to myocardial infarction or dysrhythmia. Cerebral artery emboli can cause stroke or seizures.
Differentiating cerebral AGE from type II neurologic DCS is usually based on the suddenness of symptoms. AGE symptoms typically occur within 10-20 minutes after surfacing. Multiple systems may be involved. Clinical features may occur suddenly or gradually, beginning with dizziness, headache, and profound anxiousness. More severe symptoms, such as unresponsiveness, shock, and seizures, can quickly occur. Neurologic symptoms vary, and death can result. DCS of the CNS is clinically similar to AGE. Since the treatment of either requires recompression, differentiating between them is not of great importance. During the numerous dives involved in the recovery of wreckage from TWA Flight 800 (July 17, 1996 off the coast of East Moriches, Long Island, NY), rapid ascents resulting in AGE were uncommon even under stressful conditions (115-130 ft, 35-40 m; 3,167 dives; 1,689 h). [84, 85]
Acclimatization
Research is showing that experiencing DCS initiates a stress response in the body. The bubble formation causes the release of a stress protein (HSP70). The presence and preconditioning of HSP70 decreases the likelihood of developing DCS during a subsequent dive. This mechanism may be the cause for observed acclimatization with continued diving. [86, 87] Repeated compression-decompression stress acclimated (ie, developed reduced susceptibility) to rapid decompression. [88]
Etiology
Predisposing causes of decompression sickness (DCS) include the following:
-
Inadequate decompression or surpassing no-decompression limits: This includes increased depth and duration of the dives and repeated dives.
-
Doing a dive requiring decompression stops indicating longer and/or deeper dives [89]
-
Inadequate surface intervals (ie, failure to decrease accumulated nitrogen)
-
Failure to take recommended safety stops
-
Flying or going to higher altitude soon (12-24 h) after diving (increases the pressure gradient) [90]
-
Smoking [91]
-
Drinking alcohol the night before diving
-
Cold exposure after the dive
-
Prior history of DCS [89]
A principal cause of DCS is rapid ascent. A major cause of rapid ascent may be panic. Anxiety traits can be identified during instruction. [92]
Individual predisposing physiologic characteristics include the following:
-
Being male [93]
-
Obesity: Obesity had been thought to be a risk factor because nitrogen is lipid soluble. However, studies have shown that neither body fat or body mass index (BMI) correlates with venous gas embolism and resultant DCS. [94, 95] However, one study found a direct correlation between frequency and severity of DCS as BMI increased to obese levels. [96, 97] Another also correlated body mass with risk of DCS. [98]
-
Fatigue
-
Dehydration
-
Illness affecting lung or circulatory efficiency
-
Prior musculoskeletal injury (scar tissue decreases diffusion)
Predisposing environmental factors are as follows:
-
Cold water (vasoconstriction decreases nitrogen offloading)
-
Heavy work (vacuum effect in which tendon use causes gas pockets)
-
Rough sea conditions, strong current [93]
Divers who have been chilled on decompression dives (or dives near the no-decompression limit) and then take very hot baths or showers may stimulate bubble formation.
Improper use of decompression tables may increase the diver's risk. DCS may occur even if the decompression tables and no-decompression limits are strictly observed. The decompression tables and no-decompression limits list the maximum time allowed for a dive based on the maximum depth achieved (see the comment below about the US Navy tables). The limits take into consideration nitrogen saturation of lipid tissues. According to the Henry law, once nitrogen has saturated tissues, a standard ascent to the surface with decreasing ambient pressure can allow nitrogen to bubble out of solution. Once the no-decompression limit has been passed, one or more decompression stops are required during ascent to allow delayed diffusion of nitrogen out of the lipid tissues back into the blood. Nitrogen then exhales through the lungs. Current recommendations are for routine decompression stops, even if within the times of the tables. These tables also include calculations based on the surface interval between dives and residual nitrogen offloading during the time between dives.
The original tables have three problems. First, the tables are based on young, healthy, and fit US Navy volunteers. Since many civilian divers do not fit this profile, the tables have limitations. Second, the rapidly expanding use of dive computers takes into account the actual time spent at each depth, rather than just the maximum depth. This allows for more time under water and removes a built-in factor (the shorter maximum depth time) that helps keep divers in the conservative range. Third, the number of casual divers is increasing. This can lead to mistakes from lack of practice of the stringent routine/adherence to safety principles needed
See the discussion under Prevention for more information.
Epidemiology
Frequency
United States
Between 1987 and 2003 the Sports & Fitness Industry Association (formerly the Sporting Goods Manufacturers Association) estimated the number of scuba divers who dive at least once a year in the United States to have risen 32.1% from 2.4 to 3.2 million participants. However, over the 6 years of 2000-2006, a decrease of 23% to 3.2 million had occurred. Moreover, by 2012 there were 2.87 million divers. The peak year was 1998 at 3.5 million. Of equal importance is the breakdown of those divers. Only about one third of divers were active or regular participants. Approximately two thirds of divers were casual divers, with many as little as a single dive in a year. [103, 104, 105, 106] “As of 2015, more than 23 million scuba diver certifications have been issued across the globe.” [107] Worldwide, there are an estimated 7 million active divers. [108] Experience yields a safer diver, though at the other extreme, over confidence can lead to pushing too close to limits. [109, 110]
Due to variability in reporting and collection of information, mainstream medical journal publication of diving-related injury statistics is inconsistent. To improve statistical collection of information, the Divers Alert Network (DAN), based in North Carolina in the United States, acts as a medical information and referral service for diving-related injuries. In addition to this role, it provides education, acts as a clearinghouse for reports of diving-related injuries from around the world, and participates in studies related to diving injuries and illnesses.
Their efforts to be the clearinghouse and repository of injury reports have been hampered in recent years (from 2003 forward) in the United States because of a change in federal law that makes medical confidentiality more stringent and thus their abilities to obtain reports and follow-up that much more difficult. [111] They also have sponsored an ongoing long-term research study entitled Project Dive Exploration (PDE). According to DAN, fewer than 1% of divers experience DCS. [112]
International
See Morbidity and Mortality below.
Age
Many scuba divers start out in the sport young and relatively healthy. With time, they develop medical conditions. Likewise, other divers have significant medical issues upon entering the sport. An Australian study identified that a significant prevalence of medical conditions existed in experienced divers. Many conditions would be considered to disqualify these divers from future participation in scuba diving. [113] In 2001 in the United Kingdom, they did away with a requirement for mandatory diving physicals. They instead opted for a self-reporting format. An apparent consequence is that an increase in diving deaths in those older than 50 years in the United Kingdom has been noted since 2009. [114]
DAN data also notes a steadily aging trend in their data. [115, 116]
Mortality and Morbidity
Separating mortality data for decompression sickness (DCS) from those for barotrauma is impossible. Pathologists demonstrated little knowledge of diving accidents while performing autopsies and missed the more subtle diving injuries. [117, 118]
Divers Alert Network (DAN) has been tracking diving injuries since the 1980s. They started publishing that information in 1988. The information comes from a variety of sources. When they become aware of an incident, they do their best to investigate and obtain the details of the events and injuries. In 2015, DAN identified 127 recreational diving fatalities worldwide. Another 13 were found that were not recreational. Of those, 67 were either Americans or Canadians who died in those countries and related territories, or overseas. Florida had the most, double that of California, at number two. Males represented 80% of the fatalities, and 90% were older than 40 years. A top cause for fatality, in cases that had an enough information to draw conclusion, is health problems. Over the 28 years that DAN has collected fatality data, they have received reports of 3341 fatalities. During that time, the average number of annual deaths of Americans or Canadians, at home or abroad, has decreased from 90 to 80. In about half (1549) the cases, over 24 years since 1992, a cause of death was able to be determined. Drowning accounted for 66% (1,001), 16% (250) were cardiac related, AGE occurred in 13% (201), other varied issues at 3% (46), DCS at 1% (15), and immersion pulmonary edema was cited in 1% (15). During the approximately 23-28 years of data, the age of fatalities has steadily increased in the older-than-50-years segment. In addition, the body mass index for overweight and obese divers who died has also steadily increased. Between 2004 and 2015, DAN received reports of approximately 610 additional fatalities in the breath-hold (free-diving) community. [119]
In 1995, 590 cases of DCS were analyzed (of a total 1,132) by DAN. [112] Of these, 27.3% were type I (pain-only DCS) and 64.9% were type II (neurologic DCS). The remaining 7.8% were AGE cases. In 2015, DAN received 3,589 emergency calls of which 2,124 were determined to be a diving-related medical issue. Of those, 599 were classified. Type I DCS cases breakdown to be cutaneous at 173, pain only at 138 (23%), inner ear at 31, and pulmonary at 9. Type II DCS cases represent 279 (47%). Barotrauma cases accounted for 1,211 cases (see Dysbarism), of which 41 were due to AGE. [119]
A study from the US military in Okinawa reported 94 cases of DCS over 7 years. [120] The annual incidence of DCS was 13.4 cases per 100,000 dives or 1 per 7,400 dives.
Another study from Britain 1992-1996 found that the annual incidence of diving accidents increased from 4 cases per 100,000 dives to 15.4 cases per 100,000 dives during that time.
In another study, the lifetime incidence of DCS was 1 case per 5,463 dives. For severe DCS, it was 1 case in 20,291 dives. It was also found that the more experienced divers were less likely to get DCS, presumably through more meticulous adherence to safety concerns and safer diving profiles. [121]
Internationally, minor incidents related to diving occur in 1.3% of dives. Decompression injuries (not separated as to dysbarism or DCS) occurred at a rate of 2 cases per 10,000 dives. [122]
The DAN PDE (Project Dive Exploration) study has followed about 8,000 divers for around 100,000 dives since 1995. [115] The incidence of DCS in this population is 3.6 cases per 10,000 dives (or about 36 cases since the study began). Through the PDE study, two groups were specifically observed. One is for divers in the colder North Sea and the other for divers in temperate regions, primarily the Caribbean. The colder water group has seen a dramatic decrease in DCS from 400 to 100 cases per 10,000 dives over the most recent 3-year data period. For the warmer water group, the yearly incidence is 50 per 10,000 or less. A more recent summary of the PDE data reports 10,248 divers, of which 71% are male with a mean age of 41 years. They completed 122,129 dives of which over 17,000 involved Nitrox gas. There have been 38 episodes of DCS, for a rate of 3.1 cases per 10,000 dives. [119]
DAN also participates in a diver's insurance program for injuries while traveling in general (though most of the travel is diving related). [116] The incidence of diving-related injuries, although not just DCS, is around 20.5 claims per 10,000 insured over a 7-year period. [123] The annual death rate from the same data was between 12 and 23 deaths per 100,000 insured. [124]
DAN PDE data for 2004 is based upon almost 24,000 dives. [115] In this group, about 1,300 reported an incident during the dive that could have been equipment, procedural, or equalization issues. Twelve non-DCS injuries (of which some were dysbarism related) were reported. Two cases of type I DCS, 3 cases of type II, none of AGE (see article on Dysbarism), and 2 cases that were undetermined. DAN has analyzed their data in a very detailed manner.
A large New Zealand charter dive operation also keeps detailed records. During a 6-year period, they had 97,144 dives. Of these, there were 55 injuries from scuba diving. The majority, 35, were soft-tissue mechanical injuries. There was one cardiac-related death. Only four divers were diagnosed with DCS and received HBO therapy. The prevalence was 0.41 cases per 10,000 dives. [125]
Available mortality rates are as follows:
-
In South Africa, the mortality rate was found to be as low as 0.016%. [126]
-
The US military in Okinawa reported fatalities at 0.0013% (1.3 deaths per 100,000 dives). [120]
-
A New Zealand report states that the most common cause of death was drowning, but pathologists were frequently imprecise. [118]
-
In the United States, 3-9 deaths per 100,000 dives annually occur. The most common cause of dive-related death is drowning (60%), followed by pulmonary-related illnesses.
-
Diving fatalities in the United States and Canada have fluctuated year to year but have averaged around 83 over the past two decades.
-
The mortality rate is around 10-20 diving fatalities per 100,000 DAN members and increases by about one case per year.
-
In the breath-hold free-diving group, fatalities have steadily increased worldwide over a decade to 22 in 2004. Note that only 5 or less were related to free-diving competitive activities, either training or competition. Most fatalities were during snorkeling, spear fishing, or collecting of marine specimens.
-
Divers Alert Network (DAN) studied mortalities over an 11-year period (1992-2003) to try to identify causes. Not surprisingly, asphyxia was a common cause for death, with entrapment and insufficient gases as the two most common in this category. Arterial gas embolism (AGE), also a common cause of death, resulted overwhelmingly by emergency ascent with insufficient gases as a key contributing factor. For those older than 40 years, there was an association with cardiovascular disease. [127] In AGE, mortality and morbidity is directly related to time to hyperbaric oxygen (HBO) treatment. If recompression with HBO occurs within 5 minutes, the death rate is only 5% with little residual morbidity in the survivors. If delayed 5 hours, mortality increases to 10% with residual symptoms in half of the survivors. [128]
-
An increase in diving deaths in those older than 50 years in the United Kingdom has been noted since 2009. [114]
Prognosis
Early symptom recognition, prompt diagnosis, and appropriate treatment are key to a positive outcome with decompression sickness (DCS). With these, a success rate of greater than 75-85% is achievable.
Patient Education
Diver education is paramount. They must learn the symptoms, signs, and management of decompression sickness (DCS) and AGE to facilitate early recognition and treatment. Of 590 patients with DCS whose characteristics were studied (results discussed in Epidemiology), nine continued to dive after developing neurologic symptoms, including one patient with paralysis in both legs. Approximately 7% of patients who reported to DAN reported a delay in seeking treatment until more than 96 hours after symptom onset. In addition, 35% of all cases were reported to DAN more than 4 hours after symptom onset.
For patient education resources, visit the First Aid and Injuries Center. Also, see the patient education articles Barotrauma/Decompression Sickness and The Bends - Decompression Syndromes.
-
Illustration of Dalton gas law. As an individual descends, the total pressure of breathing air increases and the partial pressures of the individual components have to increase proportionally. Nitrogen at higher partial pressures alters the electrical properties of cerebral cellular membranes, causing an anesthetic effect. Oxygen at higher partial pressures can cause CNS oxygen toxicity.
-
Illustration of Henry gas law. If nitrogen is added to a bottle, it diffuses into and equilibrates with the fluid. With a sudden release of pressure (decreased), such as when an individual ascends rapidly, a lag occurs before nitrogen can diffuse back to the nonfluid space. This delay causes nitrogen to bubble while still in the fluid.







