Background
Cysticercosis is a systemic illness caused by dissemination of the larval form of the pork tapeworm, Taenia solium. Encystment of larvae can occur in almost any tissue. Involvement of the central nervous system (CNS), known as neurocysticercosis (NCC), is the most clinically important manifestation of the disease and may present with dramatic findings. Moreover, neurocysticercosis is the most common helminthic infection of the CNS. [1] Neurocysticercosis is a major cause of seizure disorder in parts of the developing world, and its incidence is increasing within developed countries.
In impoverished countries and those in which pigs are raised, T solium is a significant etiology of seizures. Although neurocysticercosis is not widespread in the United States, it must be considered during the evaluation of a patient with newly onset seizure. Up to 10% of hospitalized patients in the United States with neurocysticercosis die of this preventable disease. [2]
See the image below.
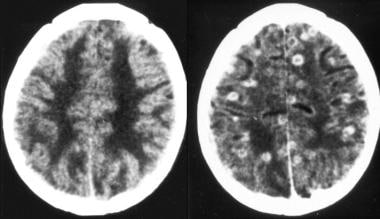 Nonenhanced (left) and enhanced (right) CT scans of the brain in a patient with neurocysticercosis show multiple ring-enhancing lesions with perifocal edema.
Nonenhanced (left) and enhanced (right) CT scans of the brain in a patient with neurocysticercosis show multiple ring-enhancing lesions with perifocal edema.
Pathophysiology
Humans are the definitive T solium hosts and can carry an intestinal adult tapeworm (taeniasis), often without symptoms. Intermittent fecal shedding of egg-containing proglottids or free T solium eggs ensues, with the intention that the intermediate host (normally pigs) will ingest the excreted eggs in contaminated food or water. T solium embryos penetrate the GI mucosa of the pig and are hematogenously disseminated to peripheral tissues with resultant formation of larval cysts (cysticerci). When undercooked pork is consumed, an intestinal tapeworm will again be formed, completing the life cycle of the worm.
Human cysticercosis occurs when T solium eggs are ingested via fecal-oral transmission from a tapeworm host. The human then becomes an accidental intermediate host, with development of cysticerci within organs. Cysticerci may be found in almost any tissue. The most frequently reported locations are skin, skeletal muscle, heart, eye, and the central nervous system (CNS). Involvement of the CNS leads to the most important manifestation of the disease, neurocysticercosis (NCC).
Symptomatology of neurocysticercosis (NCC) ranges from completely asymptomatic to severe disease and death. Symptoms largely depend on the presence of pericystic inflammation, the absence of which will usually manifest as asymptomatic disease. Lack of perilesional inflammation is seen with both "active" healthy parasites, which are able to evade host immunity (an adaptive feat that may be abetted by the immune privilege afforded to the CNS), and in "inactive" disease in which the cysticerci have completely involuted. As a corollary, inflammation is restricted to currently live but degenerating cysts whose ability to escape host defenses is faltering. Upon imaging, these inflamed degenerating cysts are typically seen as ring-enhancing lesions, an appearance that may be termed colloidal. Eventually, cysts will involute and either vanish or undergo granulomatous change and exhibit calcific scarring. Cysts in various stages of viability can be seen simultaneously in one host.
In patients with advanced HIV disease and compromised cell-mediated immunity, neurocysticercosis may exist without significant host response and is likely to be asymptomatic. For this reason, in symptomatic patients with CD4 counts under 200 cells/mm3, alternative diagnoses should be considered. [3]
Serious pathologic findings of neurocysticercosis (NCC) can include seizures, encephalopathy, obstructive hydrocephalus, meningoencephalitis, cognitive decline, focal deficits, and vascular accidents. Involvement of brain parenchyma is common and leads to the most frequent presentation of seizure or headache. Clinical expression of NCC depends primarily on the number and location of CNS cysticerci and degree of inflammatory response. As previously mentioned, host immune response and resultant pericystic inflammation are considered largely responsible for parenchymal disease manifestations. However, some evidence indicates that involuted calcific lesions may be epileptogenic as well and thus contribute to significant morbidity.
Extraparenchymal ventricular and subarachnoid cysts also are found. These carry a worse prognosis and often lead to obstructing hydrocephalus requiring surgical intervention. Cysticerci within the basilar cisterns or Sylvian fissures may become quite large. Those within the cisterns may also cause vasculitis and stroke. Spinal NCC is rare.
Ocular cysts are mostly vitreous, but they may be found in subretinal locations. Visualization of cysts via funduscopy may be diagnostic of the disease. Subcutaneous nodules represent cysticerci in the skin. Skeletal muscle encystment usually is asymptomatic but may cause muscular pseudohypertrophy with a heavy parasite burden. Cardiac cysts may lead to conduction system abnormalities.
Epidemiology
Frequency
United States
Incidence in the United States is increasing due to increased immigration from and travel to endemic areas and improved serologic testing and availability of diagnostic imaging. An estimated 1000 new cases are diagnosed per year in the United States. In southern California, with its large population of immigrants, neurocysticercosis (NCC) may account for at least 10% of seizures seen in some emergency departments and more than 2% of neurological or neurosurgical admissions. [4] The diagnosis of NCC should be considered in any patient from an endemic area presenting with new-onset seizures.
International
Cysticercosis affects an estimated 50 million people worldwide. Endemic areas include Mexico and Latin America, sub-Saharan Africa, India, and East Asia. NCC is a leading cause of adult-onset seizures worldwide. [5, 6, 7]
Mortality/Morbidity
Morbidity may result from seizures, strokes, or hydrocephalus and from effects of long-term treatment with anticonvulsants, steroids, or cerebrospinal fluid shunts.
Mortality from cysticercosis is generally limited to cases complicated by encephalitis, cerebral edema, hydrocephalus, and stroke. [8]
Race
Hispanic and Asian populations are more commonly affected due to immigration patterns from endemic areas. The disease is prevalent in South Asia as well, where patients more commonly present with a solitary cyst.
Age
People of any age may be affected. Children may be more likely to develop an unusual encephalitis-type variant.
-
Nonenhanced CT scan of the brain demonstrates the multiple calcified lesions of inactive parenchymal neurocysticercosis.
-
Enhanced CT scan of the brain in a patient with neurocysticercosis demonstrates a live cyst with a minimally enhancing wall and an eccentric hyperattenuating scolex.
-
Nonenhanced (left) and enhanced (right) CT scans of the brain in a patient with neurocysticercosis show multiple ring-enhancing lesions with perifocal edema.






